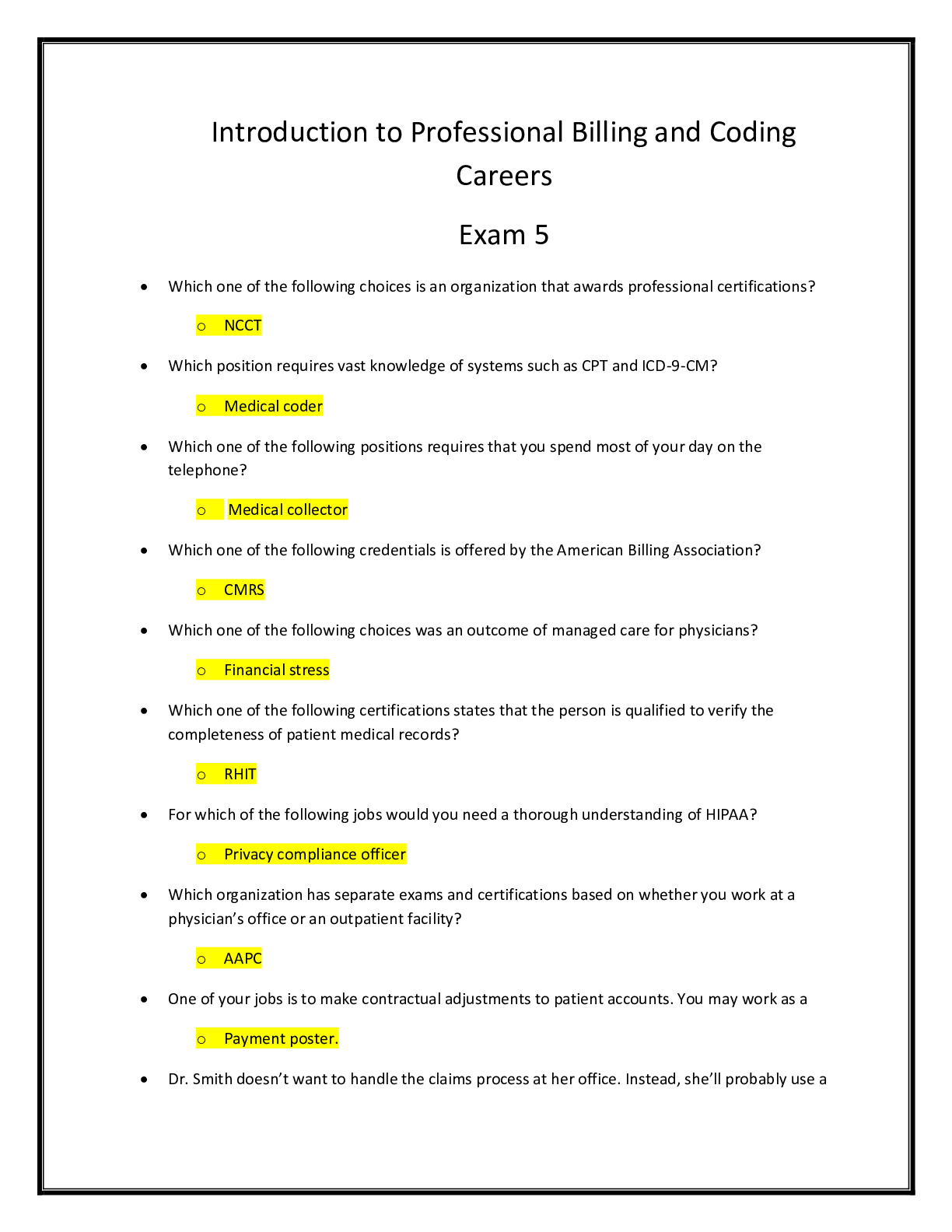
Health Care > EXAM > Medical Billing And Coding Or Mbc Exams>Ashworth College>All Exams Together (2019) 100% Graded (2019)
Medical Billing And Coding Or Mbc Exams>Ashworth College>All Exams Together (2019) 100% Graded A.
Document Content and Description Below
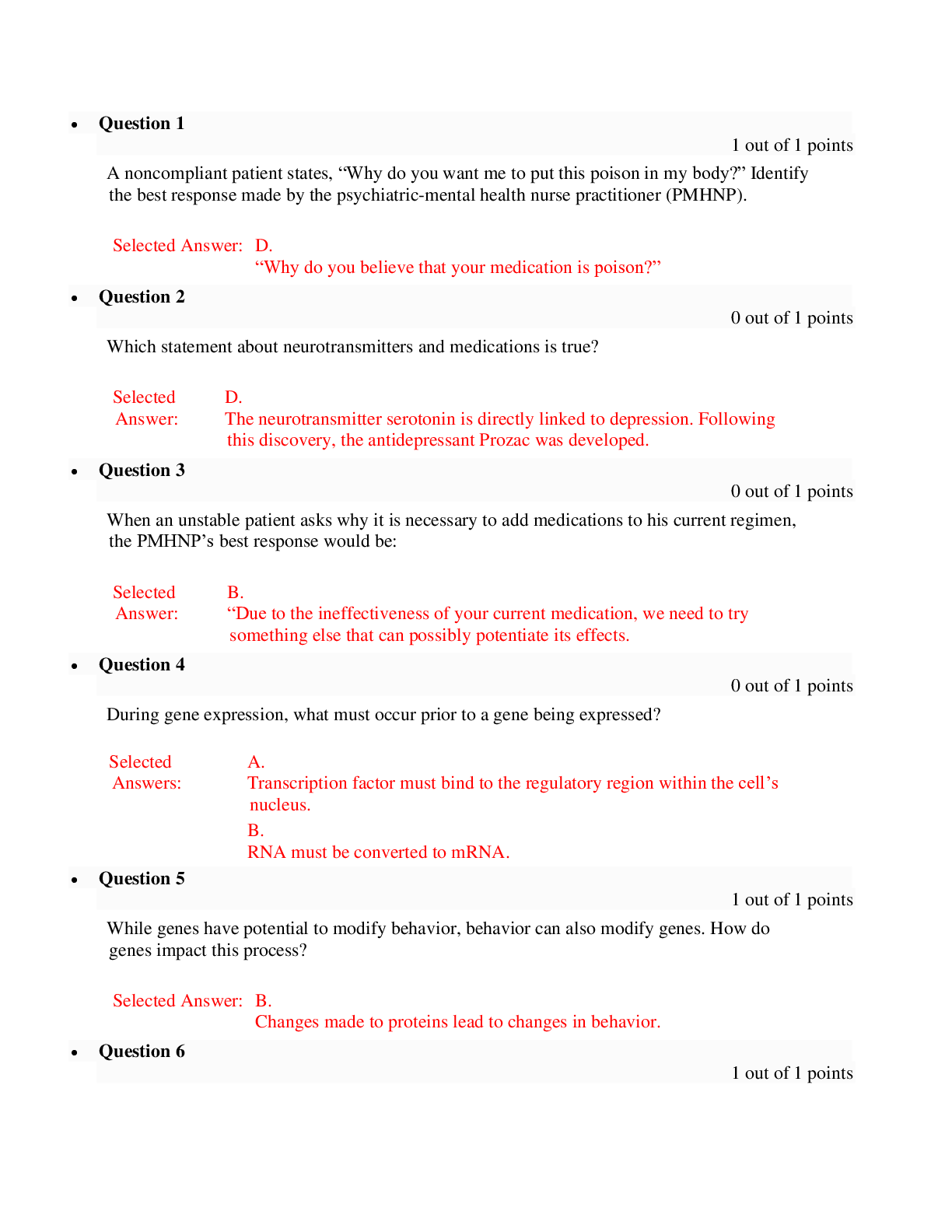
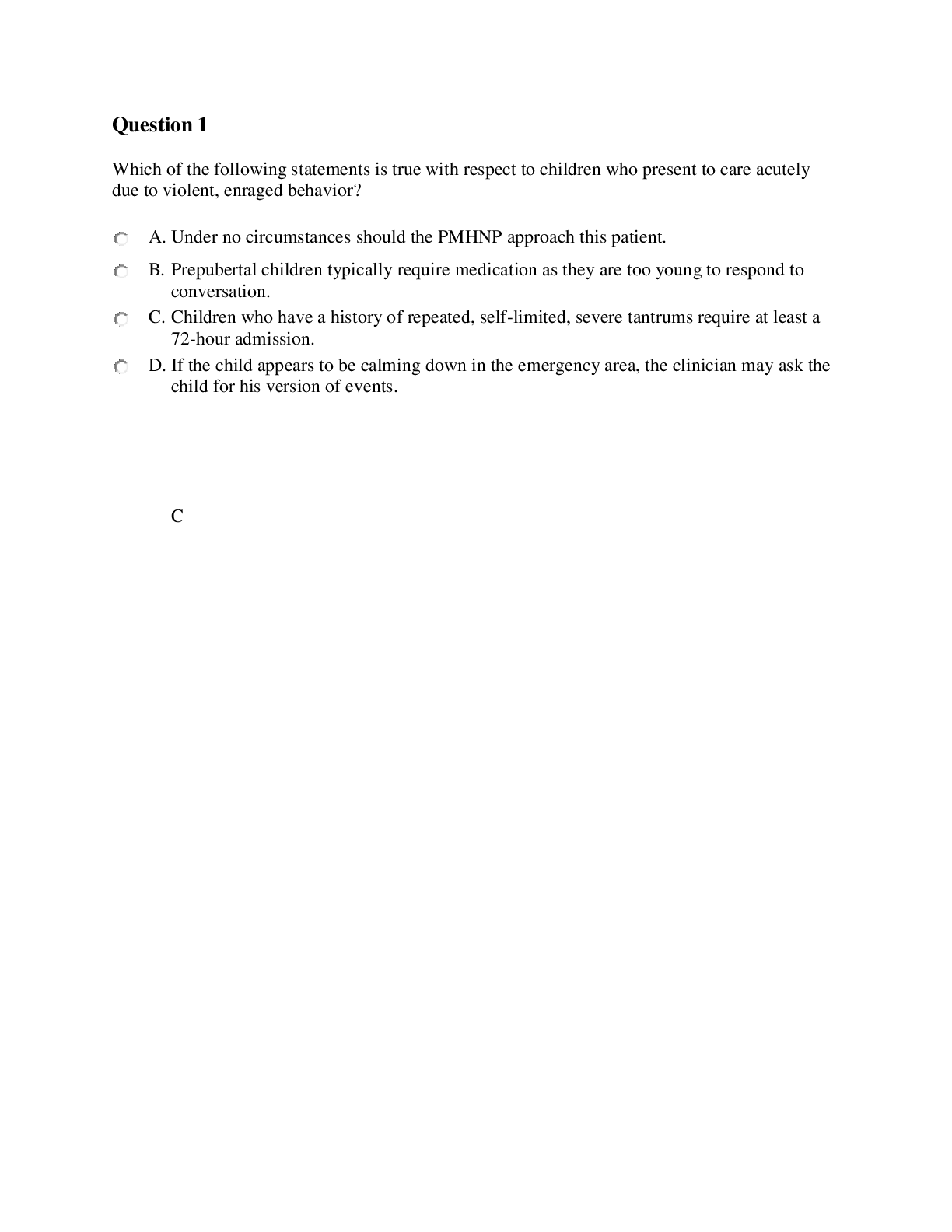
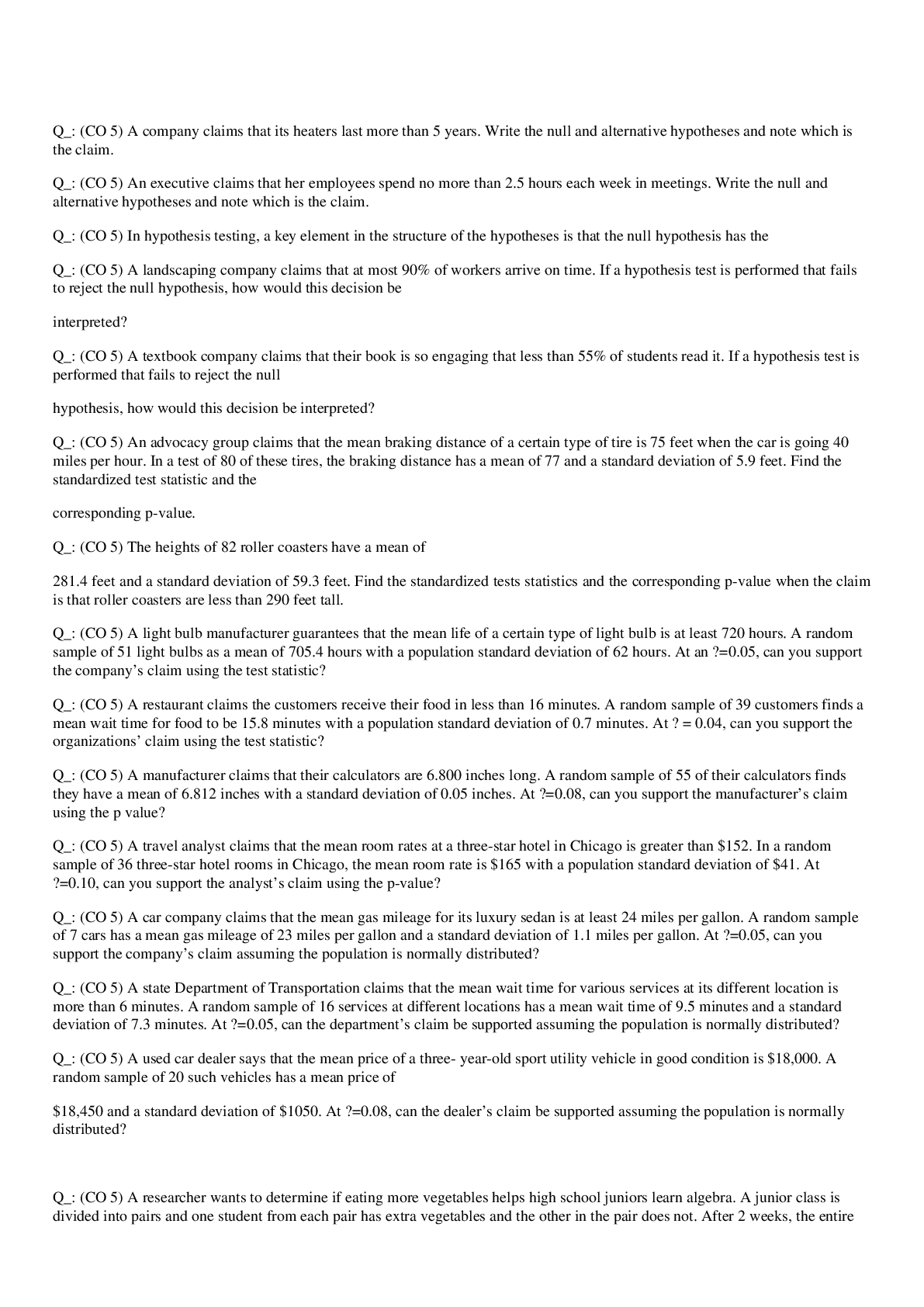
Introduction to Professional Billing and Coding Careers Exam 5 • Which one of the following choices is an organization that awards professional certifications? • Which position requires vast knowl... edge of systems such as CPT and ICD-9-CM? • Which one of the following positions requires that you spend most of your day on the telephone? • Which one of the following credentials is offered by the American Billing Association? • Which one of the following choices was an outcome of managed care for physicians? • Which one of the following certifications states that the person is qualified to verify the completeness of patient medical records? • For which of the following jobs would you need a thorough understanding of HIPAA? • Which organization has separate exams and certifications based on whether you work at a physician’s office or an outpatient facility? • One of your jobs is to make contractual adjustments to patient accounts. You may work as a • Dr. Smith doesn’t want to handle the claims process at her office. Instead, she’ll probably use a • A patient’s family has a question about a DNR order. Most likely, the family would speak to the hospital’s • Which one of the following choices is similar to a PAS, except that it focuses on physician offices instead of hospitals? • Which one of the following terms refers to monitored health care? • You’re a hospital medical coder who passed a certified medical coder examination, but you have no experience in the field. What certification might you be awarded? • Which one of the following specialists is the general cashier who must have a complete understanding of the Explanation of Benefits documents? • Which one of the following certifications would be good for a student coming out of college and entering the coding field? • If you wanted to show your mastery in coding above entry-level skills in a variety of settings, which one of the following certifications would you probably pursue? • For which of the following certifications must you have graduated from a program or have at least one year of on-the-job training? • You work in a physician’s office that has three physicians and a couple of different employees. This practice is probably classified as a _______ practice. • You want to show your dedication and commitment to the industry and your career as a medical biller. Which one of the following certifications will best help you improve your knowledge and skills? • Which one of the following choices may be an offsite service that handles a hospital’s claims and accounts receivable? • Part of your job duties includes entering patient data and charge information and contacting the insurance carrier when there are questions. You’re probably employed as a • It’s recommended that you join at least _______ professional membership(s) in your field to indicate that you’re involved and dedicated to the profession. • If a receptionist and medical biller are cross-trained for different positions, they probably work for a • Which one of the following choices was an outcome of managed care for physicians? • Which one of the following certifications is awarded through AHIMA? • Part of your job is to ensure that you determine the patient’s responsibility for charges before the patient receives treatment. You may work as a(n) • You’ve worked at a hospital for two years and just passed a coding certification exam. Which certification were you probably awarded? • You work in a physician’s office that has three physicians and a couple of different employees. This practice is probably classified as a _______ practice. • Which one of the following professionals probably has the most face-to-face contact with patients? • Physicians and nurses comprise _______ percent of all healthcare providers. Insurance Plans Exam 6 • Which one of the following types of insurance is considered some of the least expensive insurance? • Before 1993, how did many people pay for their healthcare services? • Which one of the following choices is a disadvantage of managed care? • Which one of the following outcomes was a result of physicians being excessively sued? • Which one of the following choices represents a disadvantage of managed care organizations? • If you want protection against a certain type of accident or illness, which insurance should you get? • Healthcare plans administered by a TPA are typically which type of plan? • When multiple doctors become employees of a group practice and contract with an MCO to deliver health care to members of the network, they’re probably participating in a (n) _______ model. • You pay additional expenses to cover the huge medical expenses that aren’t covered by your normal policy. Which type of insurance do you have? • A POS plan allows patients to • You’re a medical office specialist who just asked a patient if she has health insurance. What is probably your next step? • Which one of the following choices is an important reason for medical office specialists to understand the history of health care in America? • Mrs. Smith is a widow who had previously received coverage through her husband’s insurance. Mrs. Smith can continue to receive coverage under • How do you determine how much a carrier is responsible for paying? • The specified amount of out-of-pocket medical expenses that the insured pays annually before the health insurance policy provides coverage is called the • Which one of the following types of insurance plans is state licensed and has the most stringent MCO guidelines? • Which one of the following types of insurance plans combines features of a health maintenance organization and a preferred provider organization where the employers don’t contract with other plans? • Delivering high-quality care that manages costs is a goal of • In UCR fees, the portion that’s based on what doctors with similar training charge in a specific area is known as the _______ fee. • You have to pay $250 before your insurance begins. This amount is known as the • Options available through managed care organizations include the preferred provider organization (PPO), the point-of-service plan (POS), and the • In 1982, which one of the following choices made it easier for HMOs to work with Medicare? • A regularly scheduled payment made to purchase an insurance policy is known as the • When an MCO keeps a percentage of a physician’s revenue until year end, it’s referred to as • If an insurance carrier’s rate of benefit is 85 percent, what is the patient’s coinsurance? • Which one of the following choices represents a common criticism of MCOs? • If negotiated managed care fees are too low, how could a physician make up the difference in payments? • Which one of the following choices can increase costs in managed care? • When a physician agrees to accept a payment directly from the patient’s insurer, it’s called Medical Contracts, Ethics, and HIPPA Exam 7 • Under HIPAA, which one of the following choices can be given to a patient’s friend or relative without a signed authorization? • Procedures that document how to handle security breaches of patient information are an example of • Resources that are required for adequate health care are referred to as • A hospital has just signed a contract with a managed care organization. The hospital is known as the • Under a capitated agreement, the primary care provider is compensated based on • Which one of the following choices may use PHI to better understand and review product recall situations? • Each managed care contract has its own authorization and claims requirements, as well as its own • Which one of the following choices could present an increased financial risk to a physician? • After the provider credentialing process, the MCO • If someone obtains PHI under false pretenses, he or she may receive a penalty of up to • Which one of the following choices requires that an MCO plan being reviewed for accreditation demonstrates that it has done a thorough credentialing process for providers? • The primary intent of HIPAA is to provide better access to health insurance, to reduce administrative costs, and to • If someone violates HIPAA standards, they may receive a civil penalty of up to • Which one of the following choices is one of the main reasons that privacy complaints are filed? • You work in a hospital and you’re speaking with the person responsible for receiving complaints from patients about their health information. You may be speaking to the • A policyholder may also be called a • Managed care contracts contain a list of medical services covered in the contract under the • A patient is in a coma and can’t consent to or authorize release of information. The physician may disclose relevant information to family members or close friends if • The security sections of HITECH were meant to prevent PHI from • You had an appointment with Dr. Smith for an illness, but Dr. Smith isn’t a provider within the MCO. Dr. Smith is known as a(n) • Which one of the following choices identifies employer-sponsored health insurance? • Which one of the following choices was created to simplify submitting insurance claims electronically? • What is the key element of any managed care contract? • Which part of an MCO contract should contain a list of CPT codes and the rate for those services? • Electronic data interchange is the • Ethically, all providers and MCOs must abide by the • Which one of the following choices was created to improve HIPAA privacy and security? • One of the ways that medical office specialists can demonstrate ethical behavior is to ICD-9-CM Coding Exam 8 • To assign the correct code to a neoplasm (tumor), you should carefully study the _______ report to determine the type, site, and organ involved. • You’re using Volume 2 and notice that indented two spaces under the main term of a code there’s a description of the body site. This description is known as • Which one of the following choices may be used to determine medical necessity for services? • A patient has a keloid scar due to a laceration, which requires two separate codes. The keloid is known as a(n) • You’re looking up a code in Volume 1 and notice that the description includes a term in square brackets. The information in the brackets could be • Under coding conventions, Edwards’ Syndrome is an example of a(n) • A patient record has the code 47.01 for laparoscopic appendectomy. This coder probably used which part of the ICD-9-CM coding book to assign this code? • To ensure accurate ICD-9-CM coding and billing, code books should be purchased • In a working diagnosis, terms such as rule out, possible, and suspected • Which one of the following ICD-9-CM sections is used to find codes for use on medical forms and documents? • Which one of the following conditions always requires at least two codes? • Which one of the following choices required providers to submit a diagnosis code to be reimbursed? • A patient is diagnosed with brain cancer that has metastasized to the lymph nodes. The brain cancer is called • E codes are always used as secondary, never primary, codes in the case of poisoning or adverse effects because they’re • Which one of the following types of codes can’t be used alone or for additional follow-up care? • When you see the instructional note “code first underlying disease as” you know that the code can’t be used as the • If you’re unsuccessful in finding a code using main terms associated with V codes, you should • You should always consult the description in the Tabular List even if you’ve located a code in the Index to Diseases because • You’re reviewing patient documentation to learn why a patient is being seen. Which step are you probably performing in the coding process? • In the coding book, which instructional term does not have to be followed to ensure assignment of the correct code? • Which one of the following terms means that not enough detail has been given to assign a more specific code? • NEC is used at the fourth-digit level to indicate • A patient’s complaint of “pain and tightness in the chest” is referred to as • A patient came into the hospital complaining of pain and tightness in the chest for three days, which was coded to 786.59. Upon further examination, it was revealed that the patient had a myocardial infarction, coded to 410.11. The patient was also found to have diabetes (250.00) and was dehydrated (276.51). Which of the following codes are complication codes? • A patient came into the hospital complaining of pain and tightness in the chest for three days, which was coded to 786.59. Upon further examination, it was revealed that the patient had a myocardial infarction, coded to 410.11. The patient was also found to have diabetes (250.00) and was dehydrated (276.51). Which one of the following codes is the patient’s primary diagnosis? • A patient came into the hospital complaining of pain and tightness in the chest for three days, which was coded to 786.59. Upon further examination, it was revealed that the patient had a myocardial infarction, coded to 410.11. The patient was also found to have diabetes (250.00) and was dehydrated (276.51). On the final coding documentation and bill, how will the codes be listed? • A woman who is in her sixth month of pregnancy comes into the physician’s office. She hasn’t received any check-ups during her pregnancy and has insufficient weight gain. The primary diagnosis will be which type of code? • When coding multiple injuries, how do you determine what’s sequenced first? • A patient came into the hospital complaining of pain and tightness in the chest for three days, which was coded to 786.59. Upon further examination, it was revealed that the patient had a myocardial infarction, coded to 410.11. The patient was also found to have diabetes (250.00) and was dehydrated (276.51). Which one of the following choices is the patient’s admitting diagnosis? • A patient came into the hospital complaining of pain and tightness in the chest for three days, which was coded to 786.59. Upon further examination, it was revealed that the patient had a myocardial infarction, coded to 410.11. The patient was also found to have diabetes (250.00) and was dehydrated (276.51). Which one of the following choices is the patient’s principal diagnosis? ICD-10-CM Coding Exam 9 • Which one of the following choices is a disadvantage of using crosswalks in coding? • What happens to poisonings and other external cause codes in ICD-10-CM? • Which one of the following ICD-10-CM codes correlates to ICD-9-CM code 733.91? (Use the conversion tool located at • What is the correct ICD-10-CM code for the ICD-9-CM code 496? (Use the conversion tool located at • What organization publishes the International Classification of Diseases? • In ICD-10-CM, an “X” is used as the fifth character in some codes to • In ICD-10-CM, an “Excludes 2” note means • What important role does 3M play in the new ICD-10 system? • You’re reviewing ICD-10-CM diagnosis codes and see a “-” at the end of the alphabetic index entry. You know that this means you must • Code I50.9 translates to how many ICD-9-CM codes? (Use the conversion tool located at • The ICD-10-CM diagnosis code H65.119, acute and subacute allergic otitis media (mucoid)(sanguinous)(serous), unspecified ear, translates to how many ICD-9-CM codes? (Use the conversion tool located at • Acute appendicitis with generalized peritonitis (540.0) translates to which ICD-10-CM code? (Use the conversion tool located at • What is probably the main thing that will make the transition from ICD-9-CM to ICD-10-CM so difficult? • In the ICD-10-CM, to what does the seventh character in a code refer? • You’re using ICD-10-PCS to code procedures for patients. You probably work in a(n) • Code 496 is an example of an • Which one of the following choices can assist coders with translating and analyzing the differences between an ICD-9-CM code and ICD-10-CM code? • Which one of the following outcomes is expected to happen after ICD-10-CM is implemented in the United States? • Which one of the following organizations created the ICD-10-PCS? • In ICD-10-CM, when are three-character codes used? • When coding with ICD-10-CM, which step should you perform first? • What are the correct ICD-9-CM and ICD-10-CM codes for acute pharyngitis? (Use the conversion tool located at • Which one of the following organizations maintains the ICD-10? • You just assigned the code A02.21 for acute myeloid leukemia in remission. Which coding classification system are you using? • You’re looking up the code for congenital hydrocephalus in ICD-10-CM so you can assign the code. You notice this note below the code: “Excludes 1: Acquired hydrocephalus.” What does this note tell you? • Which one of the following choices is not used in ICD-10-PCS? • Incorporating standardized terminology, completeness, expandability, and multiaxiality are all goals of • Which one of the following choices provides a one-to-one match between an ICD-9-CM code and an ICD-10-CM code? • Which one of the following choices is a disadvantage of ICD-9-CM procedure codes? • Which one of the following choices is a disadvantage of ICD-9-CM? CPT and Place-of-Service Coding; Coding Procedures and Services Exam 10 • CPT descriptive terms, guidelines, and the identifying codes are referred to as • You’re ensuring that all procedures and services are documented in a patient’s health record. Which step of the coding process are you on? • Which one of the following tasks can be considered fraud? • What modifier should be used if a service required significantly greater effort or complexity than normal? • Which one of the following tasks helps establish medical necessity for procedures? • Which one of the following categories is reimbursed based on time? • You’ve looked up a CPT code that lists “see also” under it. What does this notation mean? • The number of days for a surgical package with all other services and procedures relating to that surgery is referred to as • Where is the primary procedure code listed on the CMS-1500? • Which one of the following code systems is an optional system developed mainly for performance tracking? • Extent of history documented, the extent of the examination documented, and the complexity of the medical decision making documented are key components for • When should physicians code and report supplies and materials used to treat patients? • A patient comes to the physician’s office. It has been a year since the doctor has seen her. The patient should be classified as a(n) • You see a CPT code with -TC as a modifier. This designation tells you that it probably is a _______ code. • Before you submit a medical claim with the modifier -57, you should • Which of the following organizations first developed and published the CPT? • You’re placing codes in the correct order so that the code with the highest reimbursement is first. Which step of the coding process are you probably on? • You code for an emergency department. You probably code mainly from which one of the following CPT code ranges? • You’re coding from the CPT book and notice a triangle next to a code. This symbol means • Dr. Smith has asked Dr. Brown to take a look at his patient and give an opinion. Dr. Smith is probably asking Dr. Brown for a • A concise statement describing a patient’s problem or condition is known as the • In terms of E/M codes, which one of the following choices could have the most significant impact on reimbursement? • Which one of the following categories is the largest section in the CPT book? • If you’re coding for ear procedures, you’re probably using which CPT code range? • Which one of the following organizations defines anesthesia services and procedures, including publishing updates? • Biopsies are performed on three separate skin lesions. How many CPT codes would be reported? • The practice of grouping related procedures into one code is known as • What is one benefit of using correct CPT modifiers? • CPT is part of • Which one of the following codes is an example of a CPT code? HCPCS, Coding Compliance, and Auditing Exam 11 • A coder doesn’t see a certain procedure performed, but the other items performed and documented infer that that particular procedure was performed. The coder codes the procedure anyway. This act is referred to as • When coding, which one of the following documents is one of the most important items you can reference in a patient’s record? • HCPCS was created in 1983 by the • A coder reports a procedure that has a higher reimbursement than the code supported by the documentation. This act is known as • A government investigator is performing an audit at a physician’s office to ensure that documentation and codes are complete. This procedure is known as • If you’re assigning the Level II HCPCS from the code range M0064–M0301, you’re probably working with • The law that states that the maximum penalty for fraud is $10,000 for each instance is an example of _______ law. • Knowingly submitting incorrect information to a payer is in violation of • Reducing the chance that a physician’s office will be audited is just one benefit of • Which one of the following choices is a common error encountered with code linkage and medical necessity? • The HCPCS modifier -TA tells the payer that the procedure is on the • Appliances or products used to assist in treating a patient are coded under • The complexity of establishing a diagnosis, including considering the number of management options, is known as • If a physician office coder needs clinical examples for the correct way to code E/M, where is the first place he or she should go? • Which one of the following parties has the ultimate responsibility for proper documentation in the patient’s record? • Healthcare organizations are required to develop and implement compliance programs due to • What kind of code is J0290? • A patient is seeing the doctor for an eye infection. The patient isn’t only being asked about the eye infection, but the provider also inquires about ten other body systems to gain a complete picture. What type of ROS is this? • What is the ultimate goal of submitting claims? • Which one of the following questions will help a physician better submit a clean claim? • Which one of the following choices occurs when a procedure that’s coded and reported is lower in reimbursement than the code that should have been reported? • Which one of the following outcomes could be a consequence of inaccurate coding? • How do payers know that the procedures being billed are medically necessary? • A patient presents to a physician’s office and says, “I’ve had a cough and fever for three days.” In the documentation, this statement from the patient is known as the • Which one of the following choices is a reason that physicians’ offices should regularly perform internal audits? • You’re performing an audit on patient records after the provider has already received payment. This procedure is known as a(n) _______ audit. • Each year the federal government announces billing codes that it will focus on to ensure that there are no occurrences of fraud. This strategy is known as the • Which one of the following choices is a key element of service? • When is an ABN required? • Which one of the following organizations helps investigate medical fraud and abuse? Physician Medical Billing Exam 12 • With the incoming ICD-10 changes, which one of the following choices is proposing changes to the CMS-1500? • You’re speaking with a patient’s insurance carrier who refuses to pay the claim even though the physician’s office provided all of the correct information. Which form could you refer to in the patient’s record? • When an insurance company is asked to send the payment directly to the physician instead of the patient, it’s referred to as • Which one of the following choices requires that those who transmit and store information electronically use a process of scrambling the information? • A patient was referred to Dr. Doe’s office by several physicians—Dr. Brown, who was the referring physician, Dr. Jones, who was the supervising provider, and Dr. Smith, who was the ordering provider. In what order would the referring physicians be listed on the CMS-1500? • On the CMS-1500, the insured person’s signature may be indicated by which one of the following designations? • You work for a company that provides claims processing for physician offices. You may work for a(n) • You have worked in physicians’ offices billing claims for five years. However, you just moved to another state to work for a new physician. With whom should you check to ensure that you understand the billing requirements for your new state? • Which one of the following individuals would use a FECA number when completing a CMS-1500? • You’re documenting a patient’s employer on the CMS-1500. Which one of the following form locators would you complete? • Which one of the following choices is an advantage of EMCs? • A child lives with both of his parents and is covered under both of their insurance plans. How do you determine which insurance is the primary insurance? • If the Medicaid resubmission number is missing on the CMS-1500, what should you do? • Jimmy is a 12-year-old boy who is seeing the doctor for a school checkup. He’s with his mom and his 18-year-old brother. Who is most likely the guarantor? • If a patient isn’t being seen on an emergency basis, what should be entered in the EMG form locator? • Patient Brown’s birthdate is January 1, 1964. How would this birthdate be entered on the CMS-1500? • Which one of the following choices may be cause for a claim to be marked as a dirty claim? • Which one of the following items would you probably not find on a routing slip? • A patient is seen in a birthing center. Which place-of-service code may be noted on the CMS-1500? • Electronic transmission of information standards, such as transaction and code sets and uniform identifiers, are covered under • You’re training a new employee about the CMS-1500 form. The employee calls the information input areas “fields.” You correct her by saying they’re called • A physician’s office needs more claim forms. Which one of the following choices could it contact? • Jane Doe has insurance through her work, but is also covered under her husband’s insurance. Her husband’s insurance may be referred to as the • Jane K. Doe is the patient and the insured. What should be entered in form locator 4 on the CMS-1500? • A claim was rejected because the patient’s insurance number on the CMS-1500 was entered incorrectly. Which one of the following choices could help to prevent this type of error? • Having a patient’s billing information available almost immediately after treating a patient is an advantage of • Which one of the following situations would require that an electronic claim be printed and submitted via paper? • You notice that a patient’s first name is misspelled on the CMS-1500 form. What should you do? • A physician’s office just saw a new patient but can’t submit a claim to the patient’s insurance. Which one of the following choices might be a reason for this? • Which one of the following choices is the correct way that an address would be entered on the CMS-1500? Hospital Medical Billing Exam 13 • Which one of the following choices will eventually replace ICD-9-CM Volume 3? • In the form locator for prior payments, what should you do when you have prior payments from other carriers? • Which one of the following choices is considered a major revenue code category on the UB-04? • Which one of the following choices pays actual charges based on treatment given to a patient? • Which one of the following choices is a payment system based on procedures that group together services? • If a patient dies at home while in hospice care, what discharge code might be used on the claim form? • Which one of the following choices represents the average resources used to provide inpatient treatment for specific diseases? • Which one of the following choices refers to patients who have been hospitalized for 24 hours or more? • Which one of the following form locators is not required by Medicare? • Which form locator describes the specific ancillary charges or accommodations? • For a Medicare patient, what happens when information is entered in form locator 72? • How are admission-type codes used on the UB-04? • In the type of bill code example of 0123, which number indicates the sequence of the bill for this hospitalization? • If you wanted to look at all of the patients in a hospital, you could access the • On the CMS-1450, what should you enter for inpatients in form locator 46? • Many hospitals converted to electronic health records to • What is the maximum number of services that can be billed on one UB-04? • A patient sees a healthcare provider for congestive heart failure. The healthcare provider will be reimbursed based on an expected amount to treat the congestive heart failure. The provider is being reimbursed based on which system? • A hospital’s CDM hasn’t been changed for the past year. Which one of the following outcomes could result from this? • Which one of the following choices is considered a major section for the UB-04? • Which one of the following physicians holds the primary responsibility for the patient’s care while the patient is in the hospital? • For reimbursement, Medicare determines a covered period for a patient by looking at which form locator? • A disabled child has insurance through his father’s employer. Which one of the following codes might be used on the CMS-1450 to indicate the relationship to the insurer? • Which one of the following choices usually increases a patient’s length of stay and may have a negative effect on the treatment? • Services listed with the corresponding HCPCS and revenue codes can be found on the • Which one of the following choices can help a hospital determine which DRG should be assigned to a patient’s account? • If you need to find the reimbursement rates for outpatient care, you might use • Which one of the following items on the inpatient record could cause an increase in reimbursement? • A hospital coder unethically assigns codes that are more severe than the patient’s true diagnosis to receive more reimbursement. This act is known as • Which one of the following choices is required for inpatient hospital claims? [Show More]
Last updated: 1 year ago
Preview 1 out of 25 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 17, 2019
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Sep 17, 2019
Downloads
0
Views
74




 (1).png)