*NURSING > iHuman > NURS 6550 and NURS 6560 IHuman Management Plan Template (Primary Diagnosis: Pneumonia, community-acq (All)
NURS 6550 and NURS 6560 IHuman Management Plan Template (Primary Diagnosis: Pneumonia, community-acquired Status/Condition: (Critical, Guarded, Stable, etc.) Stable)
Document Content and Description Below
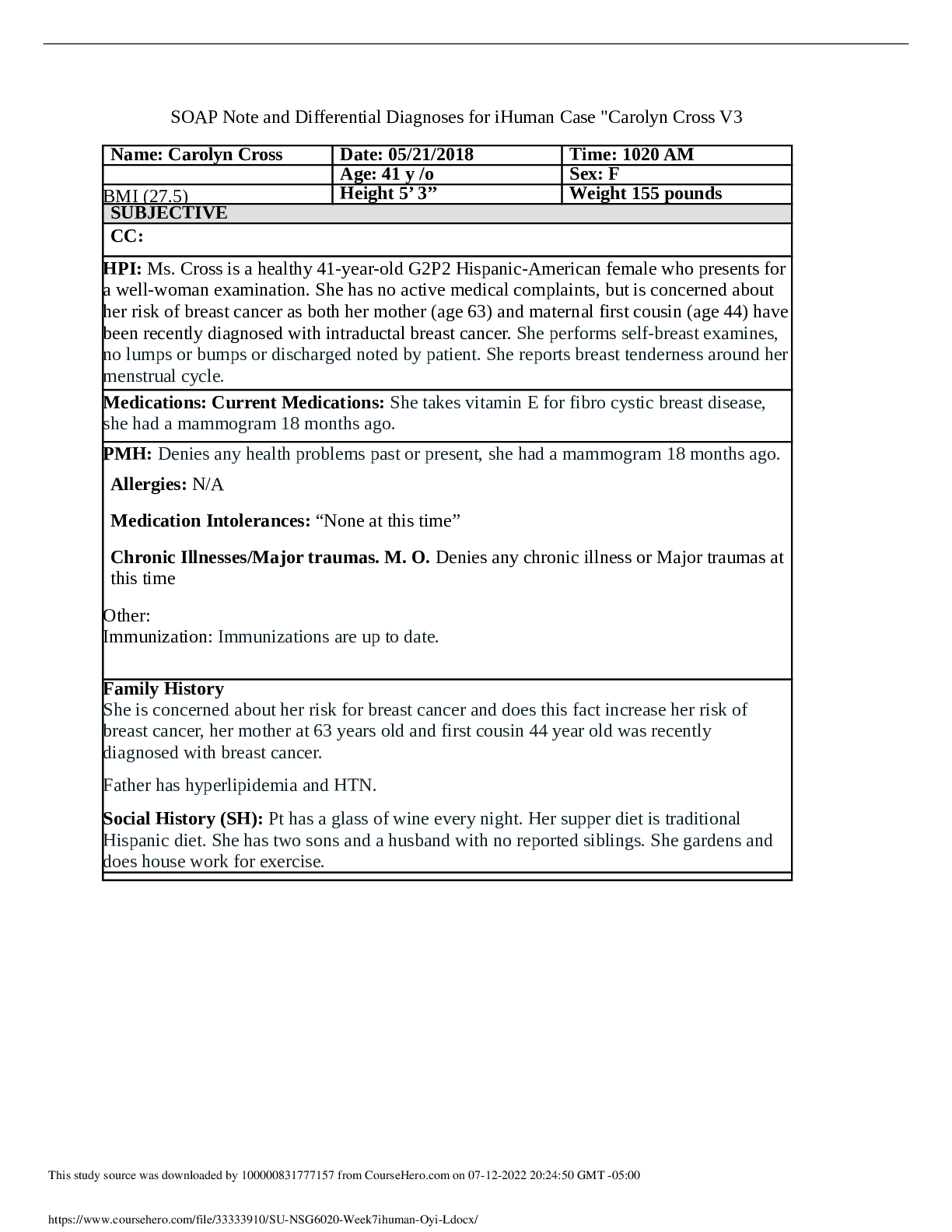
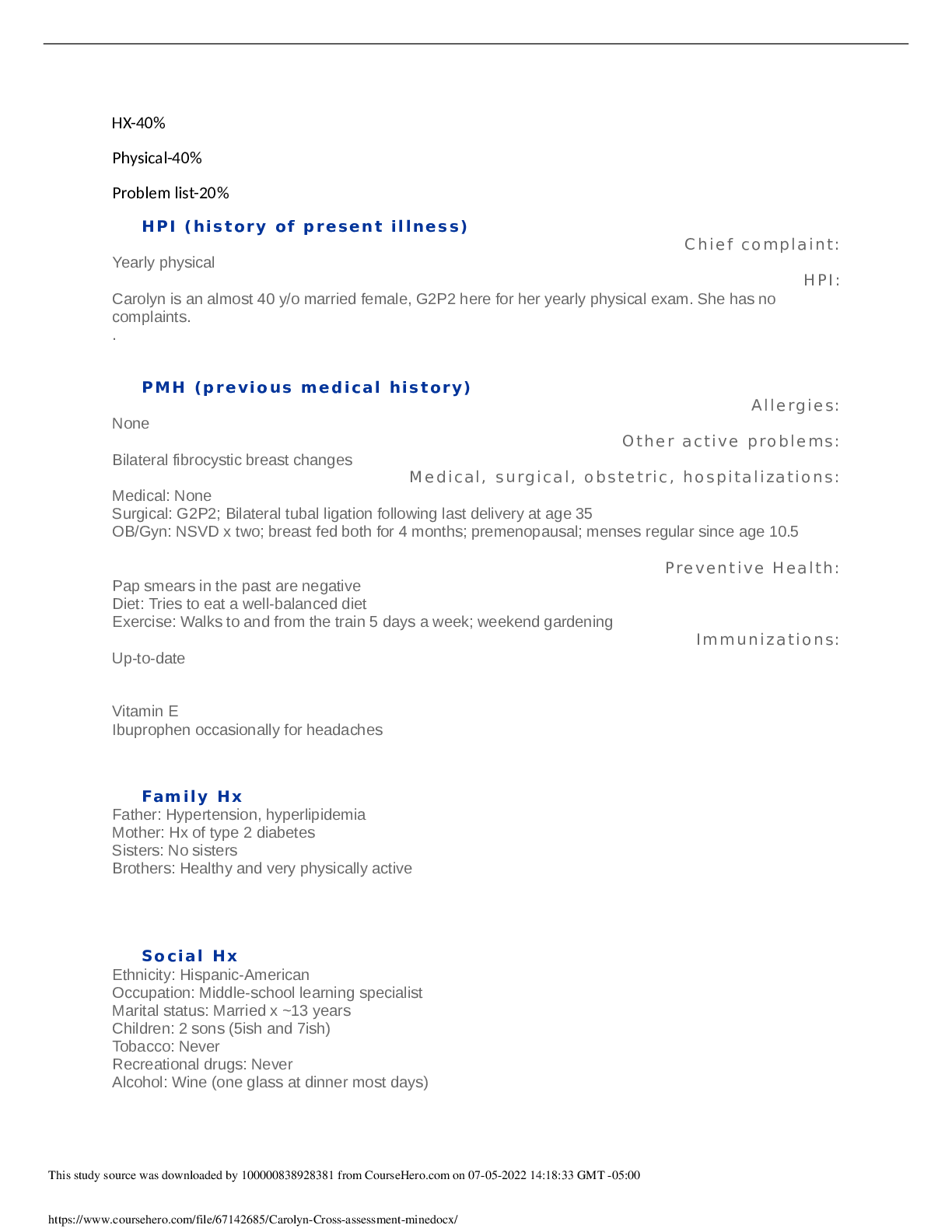
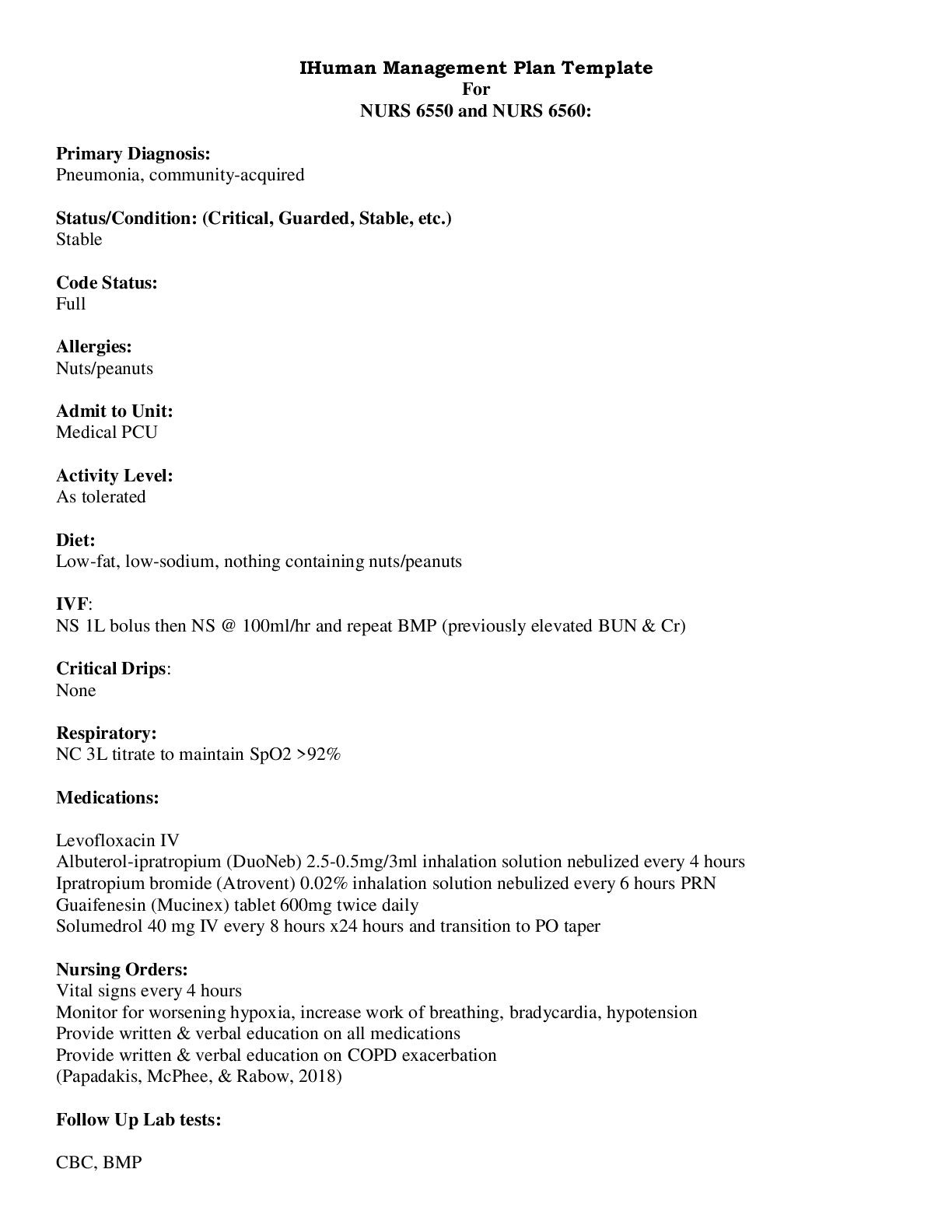
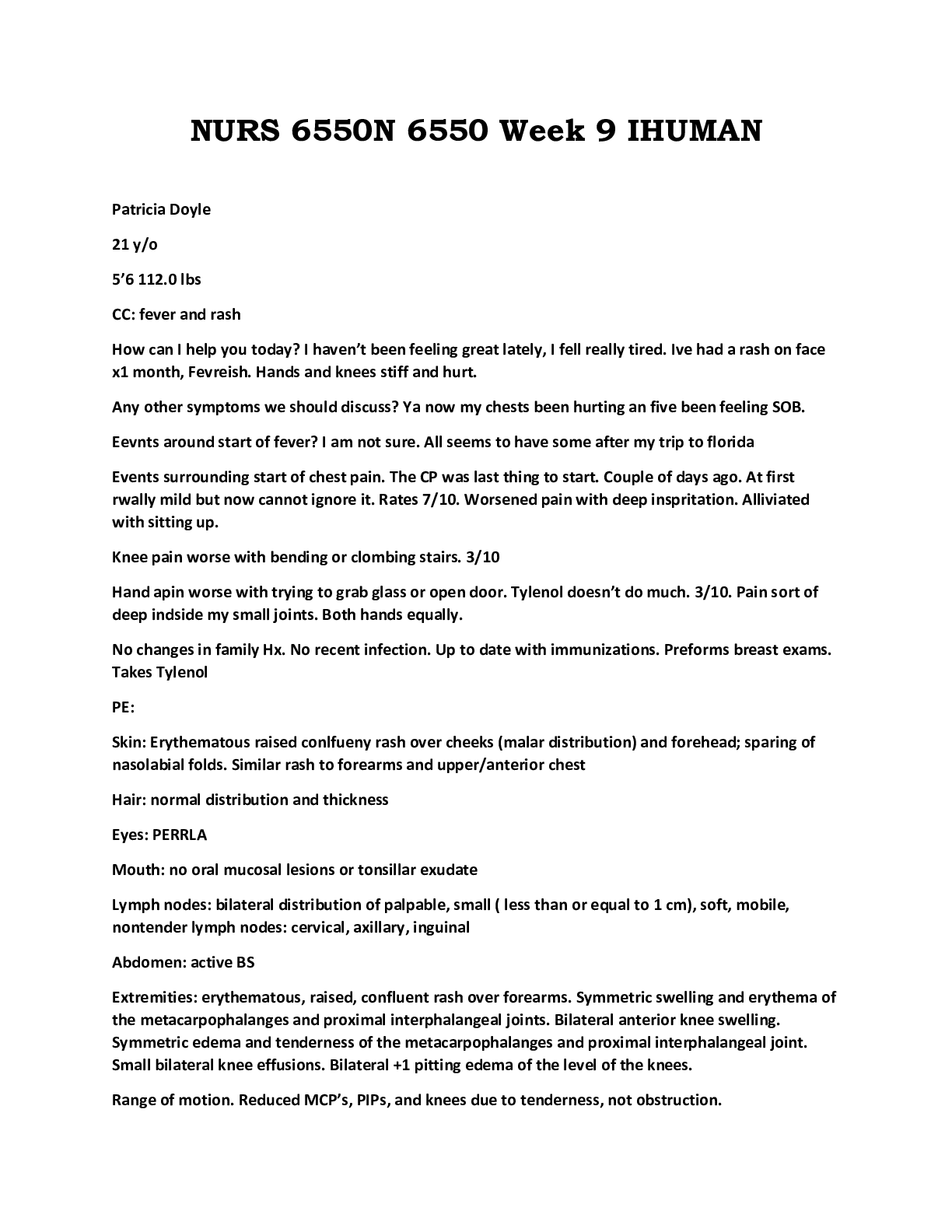
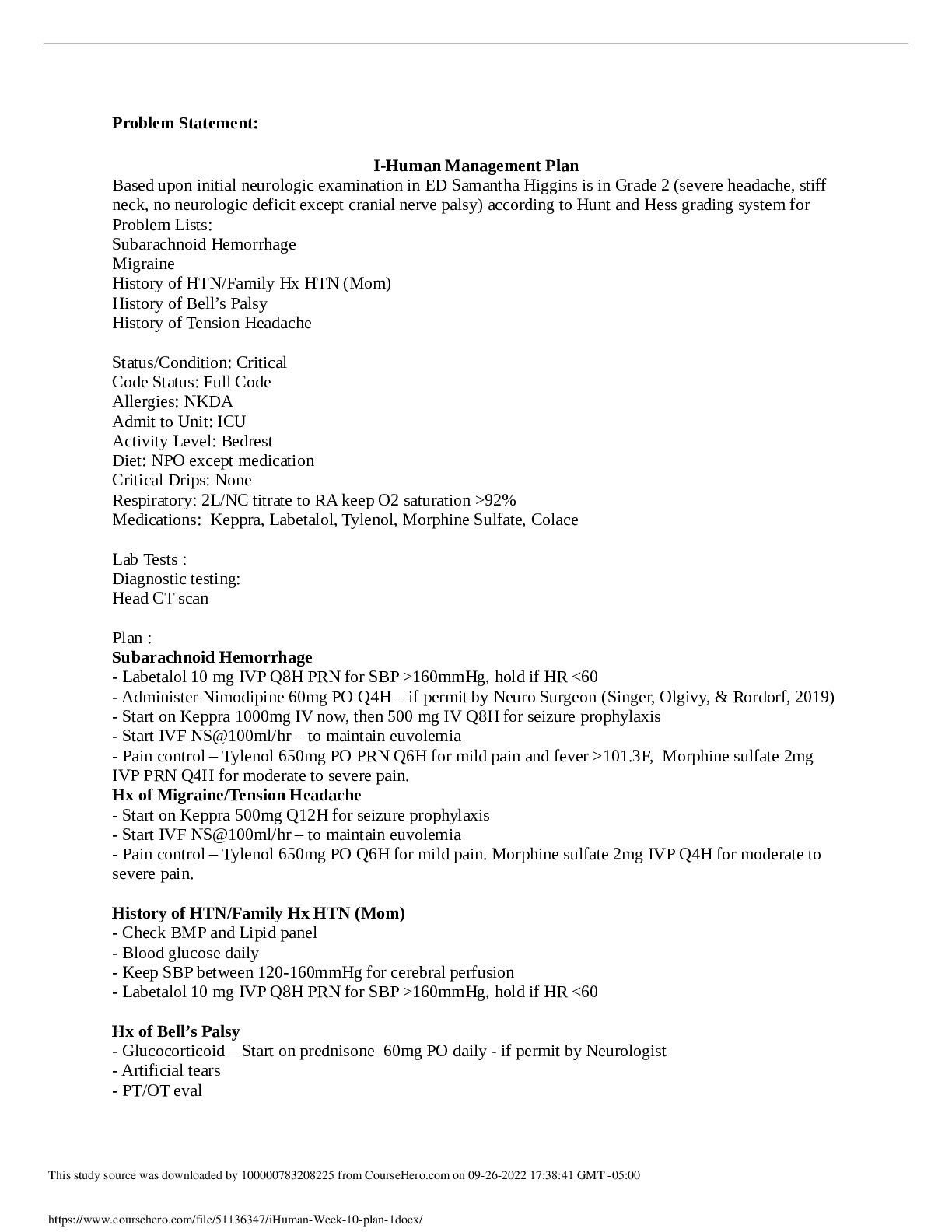
IHuman Management Plan Template For NURS 6550 and NURS 6560: Primary Diagnosis: Pneumonia, community-acquired Status/Condition: (Critical, Guarded, Stable, etc.) Stable Code Status: Full Alle... rgies: Nuts/peanuts Admit to Unit: Medical PCU Activity Level: As tolerated Diet: Low-fat, low-sodium, nothing containing nuts/peanuts IVF: NS 1L bolus then NS @ 100ml/hr and repeat BMP (previously elevated BUN & Cr) Critical Drips: None Respiratory: NC 3L titrate to maintain SpO2 >92% Medications: Levofloxacin IV Albuterol-ipratropium (DuoNeb) 2.5-0.5mg/3ml inhalation solution nebulized every 4 hours Ipratropium bromide (Atrovent) 0.02% inhalation solution nebulized every 6 hours PRN Guaifenesin (Mucinex) tablet 600mg twice daily Solumedrol 40 mg IV every 8 hours x24 hours and transition to PO taper Nursing Orders: Vital signs every 4 hours Monitor for worsening hypoxia, increase work of breathing, bradycardia, hypotension Provide written & verbal education on all medications Provide written & verbal education on COPD exacerbation (Papadakis, McPhee, & Rabow, 2018) Follow Up Lab tests: CBC, BMPDiagnostic testing: Chest x-ray (AP) (Papadakis, McPhee, & Rabow, 2018) Consults: Pulmonology for recommendations for ongoing management Patient Education and Health Promotion: Compliance with COPD medications & antibiotic therapy Ask how long she’s been taking the beta blocker for HTN and discussion changing this with her PCP Need for repeat Pneumovax 23 five years after initial vaccine Continue yearly influenza vaccine Early, frequent mobilization Discharge planning and required follow-up care: Once stable and antibiotics can be transitioned to PO, discharge home with follow-up at PCP and pulmonologist References: Mangen, M. J., Huijts, S. M., Bonten, M. J. M., & G Ardine, d. W. (2017). The impact of community-acquired pneumonia on the health-related quality-of-life in elderly. BMC Infectious Diseases, (17). Retrieved from doi:http://dx.doi.org.ezp.waldenulibrary.org/10.1186/s12879-017-2302-3 Musher, D. M., & Thorner, A. R. (2014). Community-acquired pneumonia. The New England Journal of Medicine, 371(17), 1619-1628. Retrieved from doi:http://dx.doi.org.ezp.waldenulibrary.org/10.1056/NEJMra1312885 Papadakis, M. A., McPhee, S. J., & Rabow, M. W. (2018). Current medical diagnosis & treatment (57th ed.). New York, NY: McGraw Hill. Wunderink, R. G., & Waterer, G. (2017). Advances in the causes and management of community acquired pneumonia in adults. BMJ: British Medical Journal (Online), 358. Retrieved from doi:http://dx.doi.org.ezp.waldenulibrary.org/10.1136/bmj.j2471 HPI: Mrs. Steinberg is a 69-year old female who presented to the ED with a 3 to 4-day history of progressive acute dyspnea at rest with associated fever, fatigue, productive cough with thick, dark yellow sputum, and stabbing right-sided pleuritic chest pain which worsened with deep inspiration, decreased appetite, and disturbed sleep r/t chronic cough. Significant PMH includes COPD and HTN and remote history of PUD. Physical exam was notable for hypoxemia, diaphoresis, tachypnea, right-sided course crackles in all lobes, expiratory wheezing auscultated in left upper & lower lobes. Heart rate is regular, S1 & S2 are normal. Risk factors include a 45 pack-year history of smoking tobacco and moderate alcohol consumption of approximately 2 bottles of wine/week.Health History HPI: 1. Why are you seeking help today? 2. Was the onset gradual or sudden? 3. When did the SOB start? (Duration?) 4. Have you experienced this in the past? Have a hx of respiratory illness? 5. Has it changed overtime? 6. Associated symptoms? (pain, wheezing, cough, sputum, fever) 7. Does anything make it better/worse? 8. What treatments have you tried? 9. How severe is the pain? Constant/intermittent? Worse w/ swallowing, speaking? PMH 1. Tell me about your PMH. 2. Have you been sick recently or have been around anyone that has been sick? 3. Any medical, surgical, or dental procedures? 4. Previous hospitalization? 5. Any medication changes? 6. Any prescription meds? 7. Any OTC meds or herbal supplements? 8. Any allergies? 9. Are immunizations up to date? 10. What childhood illnesses have you had? Family Hx 1. Tell me about your family medical hx? 2. Mom’s PMH? 3. Dad PMH? 4. Siblings? Social Hx1. Are you married? How long? Children? 2. Are you sexually active? 3. Do you or have you ever smoked? Drink alcohol? Use rec drugs? ROS 1. Do you have any problems with: itchy scalp, skin changes, moles, thinning hair, brittle nails? 2. Do you have any of the following problems: headaches that don’t go away with asa/Tylenol, double vision, blurred vision, difficulty with night vision, problems hearing, ear pain, sinus problems, chronic sore throat, difficulty swallowing? 3. Do you experience: chest pain, discomfort or pressure, pain, pressure, dizziness with exertion or getting angry, palpitations, decreased exercise tolerance, blue/cold fingers or toes? 4. Do you experience: SOB, wheezing, difficulty catching your breath, chronic cough, sputum production? 5. Do you have any of the following problems: muscle or joint pain, redness, swelling, muscle cramps, joint stiffness, joint swelling or redness, back pain, neck or shoulder pain, hip pain? 6. Have you noticed any bruising, bleeding gums, nose bleeds, or other sites of increased bruising? 7. Do you have any of the following problems: heat/cold intolerance, increased thirst, increased sweating, frequent urination, change in appetite? 8. Do you have any of the following problems: fatigue, difficulty sleeping, unintentional weight gain/loss, fevers, or nightsweats? 9. When you urinate, have you noticed: pain, burning, blood, difficulty starting/stopping, dribbling, incontinence, urgency or frequency? 10. Do you have any of the following problems: nausea, vomiting, constipation, diarrhea, coffe ground emesis, dark/tarry stools, BRB in stool, early satiety, bloating? 11. Do you have any of the following problems: dizziness, fainting, spinning room, seizures, weakness, numbness, tingling, tremors? 12. Do you have any of the following problems: nervousness, depression, lack of interest, sadness, memory loss, or mood changes, or hear voices or see things you know are not there? [Show More]
Last updated: 1 year ago
Preview 1 out of 4 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 25, 2021
Number of pages
4
Written in
Additional information
This document has been written for:
Uploaded
Apr 25, 2021
Downloads
0
Views
77




 2021.png)