*NURSING > Class Notes > NUR 114 Partial Focus Notes Final Fall 2019 (All)
NUR 114 Partial Focus Notes Final Fall 2019
Document Content and Description Below
NUR 114 Partial Focus Notes Final Fall 2019 CONCEPT OF SEXUALITY Recommendations for testing and assessment for PAP smears, Breast cancer, Prostate CA, Testicular CA. HPV ◦ PAP SMEAR: ▪ a... cytological study that is effective in detecting precancerous and cancerous cells within the female patient’s cervix. ▪ When to get tested: Not recommended for women under 21 (unless SEXUALLY ACTIVE) 21-29 every 3 years 30-65 every 5 years + HPV test 65+ whom has had normal Pap’s in the past should not receive pap test. Other’s suggest 60+ every 3 years Those who have had a Hx of cervical cancer should get tested yearly for at least 20 years after the diagnoses regardless of age. ◦ HPV test: can identify many high-risk types of HPV infections associated with the development of cervical cancer. ▪ When to get tested: At the time of a pap for women 30+ for any woman of any age who have had an abnormal pap result. ◦ PSA test: ▪ a prostate-specific antigen test is used to screen for prostate cancer and to monitor the disease after treatment. ▪ Normal lab value: 0-2.5 ▪ An elevated PSA should decrease a few days after a prostatectomy. If it has not it shows that it has reoccurred. ▪ Elevated numbers are associated with prostate cancer. ▪ Older men (Esp. AA men) often have a higher PSA. ▪ Should be drawn before a digital rectal exam because the exam can cause an increase in PSA due to prostate irritation. ◦ Mammogram: ** 40 is the magic number ▪ A mammogram is a x-ray of the soft tissue of the breast. Mammograms assess differences in the density of breast tissue. ▪ Helpful in evaluating poorly defined masses, multiple masses or nodules, nipple discharge or changes, skin changes, or pain. ▪ AGE INFORMATION: Women ages 40 to 44 should have the choice to start annual breast cancer if they wish – Women age 45 to 54 should get mammograms every year. Women aged 40 years and older be offered screening mammography annually Women age 55 and older should switch to mammograms every 2 years, or have the choice to continue yearly screening. American College of Obstetricians and Gynecologists recommends annual screening mammography for women age 40 and over Yearly screening is recommended at age 40 because younger women have higher density in breast tissue and the test is less effective. ▪ In older women, the amount of fatty tissue is higher. Therefore, fatty tissues appear lighter than cancer ▪ Cancer and cysts usually have the same density. However, cysts are smooth borders and cancers are usually star-burst shape ◦ Testicular Cancer: ▪ Rare form of cancer that most often effects men between ages of 20-35 years of age. ▪ With early detection there is a 95% cure rate ▪ Most common type is germ cell tumors arising from sperm-producing cells Seminoma tumors are usually localized, metastasize late, and respond to treatment. ▪ Least common type is non-germ cell tumors in stromal, interstitial, or Leydig cells Most do not metastasize Adroblastomas sometimes secrete estrogen, which causes feminization and gynecomastia ▪ Men with cryptocordism or HIV have higher risk of testicular tumors. ▪ Common tumor markers that confirm testicular cancer are alfa-fetoprotein, hCG, and LDH What are the types and s/s of benign breast disorders? Benign Breast disorders 1. Fibroadenoma o Most common benign tumor in women during reproductive years o Mass of connective tissue unattached to surrounding breast tissue o Tumors are oval, freely movable, rubbery 2. Fibrocystic Breast Condition (FBC) o Fibrocystic changes of breast (may involve lobules, ducts, stromal tissues) o Common in pre-menopausal women between 20 and 50 years of age o Thought to be caused by imbalance in normal estrogen-to-progesterone ratio o Symptoms: Breast pain, tender lumps, swelling (often before menstrual period) o Two main features of FBC: fibrosis and cysts Fibrosis made up of connective tissue and are hard and firm Cysts are fluid filled and glandular cells – Breast US is used to confirm presence of cysts. o Postmenopausal women taking hormonal replacement may develop FBC or have worsening symptoms.o This does not increase her chances of Breast CANCER; however, if a firm mass arises a mammogram may be done to rule out cancer o A needle biopsy may be done to rule out cancer IF: No fluid is aspirated Mammogram is positive Mass remains palpable after aspiration Aspirated fluid reveals cancer cells o Management of FBC: Analgesics Limit salt intake before menses Wear supportive bra at all times Ice or heat may help Reduce or eliminate caffeine, dairy product Needle aspiration may be necessary diuretics Oral contraceptives or selective estrogen receptor modulators may be prescribed o Explain to women the benefits and risks associated with hormonal drug therapy for FBC, such as stroke, liver disease, and increased intracranial pressure. Teach them to seek medical attention immediately if any signs or symptoms of these complications occur. 3. Ductal Ectasia o Benign breast problem of women approaching menopause o Caused by dilation and thickening of collecting ducts in subareolar area o Hard mass; irregular borders, tender o Greenish-brown nipple discharge, enlarged axillary nodes, redness and edema over mass o Management May improve without treatment Reduce anxiety regarding threat of breast cancer Warm compresses Antibiotics May require surgical removal 4. Intraductal Papilloma o Occurs most often in women 40 to 55 years of age o Benign process in epithelial lining of duct, forming a pedunculated outgrowth of tissueo Trauma and erosion within duct; bloody or serous nipple discharge o Mass is rarely palpable o Must rule out breast cancer Breast cancer types, S/S, High risk groups, risk factors, treatments, diagnostics Invasive VS noninvasive: There are two broad categories of breast cancer: noninvasive and invasive. Most of these cancers arise from the intermediate ducts. a. Non-invasive cancers account of about 20% of BC – occurs when the cancer remains within the duct. b. Invasive BC is the other 80% – occurs when the BC penetrates the surrounding tissue around the duct. Metastasis occurs when the cancer cells leave the breast via blood or lymph fluid – permits spread of cancerous cells to distant sites Common sites of metastasis are lung, bone, brain, and liver. Noninvasive Breast Cancers Ductal carcinoma in situ (DCIS) ◦ early noninvasive form of breast cancer ◦ cancer cells located within the duct – have not invaded the surrounding fatty breast tissue. ◦ mammography screening and earlier detection has caused the # of women diagnosed with DCIS to > ◦ left untreated, it is estimated that 14% to 53% of DCIS would become invasive and spread into the breast tissue surrounding the ducts over a period of 10 years ◦ Currently there is no way to determine which DCIS lesions will progress to invasive cancer and which ones will remain unchanged – causes anxiety and decisional conflict in many women diagnosed with this ◦ differs from invasive cancer – DCIS cells lack the biologic capacity to metastasizs lobular carcinoma in situ (LCIS) ◦ rare and occurs as an abnormal cell growth in the lobules (milk-producing glands) of the breast ◦ not a true cancer, but having LCIS increases one's risk for developing a separate breast cancer later ◦ usually diagnosed before menopause in women 40 to 50 years of age. ◦ Traditionally, treated with close observation only ◦ Women with LCIS and other breast cancer risk factors may want to consider prophylactic treatment options such as tamoxifen, raloxifene, or prophylactic mastectomy Invasive Breast Cancers Infiltrating ductal carcinoma ◦ most common type of invasive breast cancer◦ originates in the mammary ducts and grows in the epithelial cells lining these ducts ◦ Once invasive, the cancer grows into the tissue around it in an irregular pattern ◦ If a lump is present, it is felt as an irregular, poorly defined mass ◦ As tumor continues to grow, fibrosis (replacement of normal cells with connective tissue and collagen) develops around the cancer ▪ fibrosis may cause shortening of Cooper's ligaments – resulting typical skin dimpling – Late sign ▪ another late sign: edematous thickening and pitting of breast skin called peau d'orange (orange peel skin) inflammatory breast cancer ◦ rare but highly aggressive form of invasive breast cancer ◦ Symptoms include swelling, skin redness, and pain in the breasts. ◦ IBC seldom presents as a palpable lump and may not show up on a mammogram ◦ usually diagnosed at a later stage than other types of breast cancer – often harder to treat successfully Mutations 1. BRCA1 and BRCA2, are related to hereditary breast cancer 2. People who have specific mutations in either one of these genes are at a high risk for developing breast cancer as well as ovarian cancer 3. only 5% to 10% of all breast cancers are hereditary 4. Only women with a strong family history and a reasonable suspicion that a mutation is present have genetic testing for BRCA mutations. Other BC information Estrogen and progesterone receptor-negative cancers: ◦ harder to treat because the drug choices and treatment options are limited at they will not affect the cancer. HER2 receptors ◦ Human epithelial receptors are in normal breast and help them grow. ◦ In some breast cancers there are way too many and the cancer grows rapidly REMEMBER these are Signs in LATE stages cancers: dimpling may occur due to shortening of cooper’s ligaments ◦ caused by fibrosis which is the replacement of normal cells with connective tissue and collagen Peau d’orange is visible with edema of the breast (peeling of orange skin) ◦ Edematous thickening and pitting of the breast skin How to preform Self breast exam. Patient teaching. o Self-Breast EXAM steps: Lie down on your back and place your right arm behind your head Use the finger pads of the three middle fingers on your left hand to feel for lumps in the right breast. Use an overlapping dime shaped circular motion to feel for lumps Use three different levels of pressure to feel. Light feels closest to the skin, medium is a little deeper, and firm pressure feels close to the chest wall. It is normal to feel a curved ridge in the lower curve of each breast Move around the breast in an up and down pattern starting at an imaginary line drawn straight down your side from the underarm and moving across the breast to the middle of the chest bone. Be sure to check the entire breast area going down until you feel the ribs and up to the neck. Repeat on the left side While standing, exam the size, shape, contour, dimpling, and look at nipples. Stand with arms by your side in front of a mirror. Exam under the arms with your arm elevated only slightly. o Assessing a breast mass Identify the location of the mass by using the face of a clock method Describe the shape, size, and consistency of the mass Assess whether the mass is fixed or movable Note any skin changes ( dimpling, peau d’orange) Assess axillary and supraclavicular lymphatic nodes Ask patient if they experience pain or soreness in the area of the mass Care of the patient pre and post op Mastectomy and breast reconstruction postoperative care for a Mastectomy: o Sign in room and inform staff to not use the affected arm o Assess vitals every 30 mins for 2 hrs and every hour for 2 hours, and then every 4 hours. o Check dressing for bleeding o Monitor for amount and color of drainage o Assess position to make sure drainage system is not being pulled nor kinked o HOB 30 degrees o Elevated affect arm o Basic comfort measures o Analgesics o Ambulation and regular diet begin day after surgery o During a modified radical mastectomy the surgeon places one or two drainage tubes, usually Jackson-Pratt drains, under the skin flaps and attaches the tubes to a small collection chamber. Gentle suction is exerted, and fluid that would accumulate under the flaps and delay healing is collected. When taking vital signs, monitor for the amount and color of drainage. Add this information to the intake and output record. o Patients undergoing a lumpectomy may also have drainage tubes (usually Jackson-Pratt drains) placed if the lump is large or if axillary node dissection is performed. o Assess the incision and flap of the post-mastectomy patient for signs of bleeding, infection, and poor tissue perfusion. o With short hospital stays, drainage tubes are usually removed about 1 to 3 weeks after hospital discharge when the patient returns for an office visit. The drainage amount should be less than 25 mL in a 24-hour period Inform the patient that tube removal may be uncomfortable although these tubes lie just under the skin Provide or suggest analgesia before they are removed Document all findings, and report any abnormalities to the surgeon immediately. o Instruct the patient to avoid the hunched-back position with the arm flexed because of the risk for elbow contractures o Beginning exercises that do not stress the incision can usually be started on the first day after surgery. These exercises include squeezing the affected hand around a soft, round object (a ball or rolled washcloth) and flexion/extension of the elbow. Postoperative mastectomy exercises: o Hand-wall climbing: Face the wall and place hands on wall at shoulder level Flex your fingers so that your finger walk up the wall Stop when your arms feel fully exerted Slowly ―walk‖ back down the wall o PULLEY: drape a 6 ft long rope over a curtain or door. Grab the ends of the rope and extend your arms out to the sides Keeping your arms straight go down with the left and up with the right o ROPE turning: tie rope to knob of closed door Hold rope with arm extended out in front of you Swing the rope in a circular motion starting with small circles and increasing in size. Postoperative Care of the Patient After Breast Reconstruction o Assess the incision and flap for signs of infection (excessive redness, drainage, odor) during dressing changes. o Assess the incision and flap for signs of poor tissue perfusion (duskiness, decreased capillary refill) during dressing changes. o Avoid pressure on the flap and suture lines by positioning the patient on her nonoperative side and avoiding tight clothing. o Monitor and measure drainage in collection devices, such as for Jackson-Pratt drains. o Teach the patient to return to her usual activity level gradually and to avoid heavy lifting o Remind the patient to avoid sleeping in the prone position o Teach the patient to avoid participation in contact sports or other activities that could cause trauma to the chest. o Teach the patient to minimize pressure on the breast during sexual activity. o Remind the patient to refrain from driving until advised by the physician. o Remind the patient to ask at the 6-week postoperative visit when full activity can be resumed. o Reassure the patient that optimal appearance may not occur for 3 to 6 months postoperatively. o If implants have been inserted, teach the proper method of breast massage to enhance expansion and prevent capsule formation (consult with the physician). o Emphasize breast self-awareness; if the patient performs breast self-examination (BSE), review her technique. o Remind the patient of the importance of clinical breast examination and follow-up surveillance by her physician. Endometriosis s/s treatments diagnosticso Care: Assessment: menstrual history, sexual history, bleeding characteristics PAIN IS THE MOST COMMON SYMPTOM OF ENDOMETRIOSIS Usually peaks just before the menstrual flow; is usually located in the abdomen and causes a sense of rectal pressure Degree of pain not related to the extent, but it is related to the site Other s/s include: painful intercourse, painful defecation, low backache, infertility, nausea, diarrhea are also common Pelvic assessment may reveal pelvic tenderness, tender nodules in the posterior vagina, and limited movement of the uterus. Psychosocial assessment may reveal anxiety Diagnostic tests to rule out PID caused by chlamydia or gonorrhea. Serum CA-125 (cancer antigen) may be positive Transvaginal ultrasound-determine if masses are malignant or endometriosis a laparoscopy is the most definitive diagnosis in endometriosis o Interventions: Hormonal and surgical management may be used Collaborations consists of interventions that: Reduce pain Restore sexual function Alleviate anxiety r/t the disease and the uncertainty of the diagnosis Educate the pt about the disease and its treatment Alleviate fear r/t the possibility of laparoscopy or surgery Prevent self-concept disturbance r/t infertility Nonsurgical Management: Oral contraceptive to control menstrual cycle or progestins such as: o Oral medroxyprogesterone acetate and norethindrone acetate o Injectable forms of progestins: medroxyprogesterone acetate (depoprovera) Continuous low-level heat using wearable heat packs Relaxation techniques, yoga, massage, biofeedback Calcium and Magnesium supplements may relieve cramping Surgical Management: Ablation- a laprascopic removal of endometrial implants and adhesions; sameday surgery – unless you are like me and had complications :) Surgeon may use a laser to treat endometriosis by vaporizing adhesions and endometrial implants. Teach pt that temporary postop pain from CO2 used during laparoscopy to better visualize internal organs, can occurs in the shoulders or chest Toxic Shock syndrome s/s treatments diagnostics o Can result from menstruation and tampon use o Other conditions associated with TSS: Surgical wound infection Nonsurgical infections Gynecologic surgeries Use of internal contraceptives o Menstrual blood provides a growth medium for Staphylococcus aureus exotoxins produced from the bacteria cross the vaginal mucosa to the bloodstream via microabrasions from tampon insertion or prolonged use o Can be fatal o Usually develops within 5 days after the onset of menstruation o Most common s/s: Fever Rash Myalgias Sore throat Edema Hypotension Rash often looks like sunburn Broken capillaries in eyes and skin o Treatment: Removal of infection source (tampon, usually) Restore fluid and electrolyte balance Administer drugs to manage hypotension IV antibiotics Transfusion to reverse low platelet counts Corticosteroids to treat skin changes o Prevention: Wash hands before inserting a tampon Do not use a dirty tampon Inset the tampon carefully to avoid injuring the delicate tissue in your vagina Change your tampon every 3-6 hours Do not use superabsorbent tampons Use sanitary napkins at night Call HCP if you suddenly experience a high temperature, vomiting or diarrhea Do not use tampons at all if you have had TSS Not using tampons almost guarantees that you will not get toxic shock syndrome Menopause and Osteoporosis Menstrual disorders (amenorrhea, dysmenorrhea) Infertility Family Planning Contraception and Sterilization Premenstrual Dysphoric Disorder (PMDD) Leiomyomas s/s treatments diagnostics, Uterine Fibroids fibroids that are benign, slow-growing solid tumors of uterine myometrium Intramural leiomyomas ◦ are contained in the uterine wall within the myometrium Submucosal leiomyomas◦ protrude into the cavity of the uterus and can cause bleeding and disrupt pregnancy Subserosal leiomyomas ◦ protrude through the outer surface of the uterine wall and may extend to the broad ligament, pressing other organs Pedunculated leiomyomas ◦ are attached by a pedicle (stalk) to the outside of the uterus and occasionally break off and attach to other tissues Leiomyomas are the most common reason for hysterectomies. Prostatectomy Pre and post op care Surgical Management: ◦ Surgery is the most common intervention for a cure ◦ Minimally invasive surgery (MIS) or, less commonly, an open surgical technique for radical prostatectomy (prostate removal) is usually performed ◦ A bilateral orchiectomy (removal of both testicles) is another palliative surgery that slows the spread of cancer by removing the main source of testosterone Preoperative Care: ◦ Preoperative care depends on the type of surgery that will be done ◦ Minimally invasive surgery (MIS) ▪ most appropriate for localized prostate cancer and is used as a curative intervention ◦ The most common procedure is the laparoscopic radical prostatectomy (LRP) ▪ most often with robotic assistance ◦ Patients who qualify for LRP must have a PSA less than 10 ng/mL and have no previous hormone therapy or abdominal surgerie. ◦ Other newer procedures include transrectal high-intensity focused ultrasound (HIFU) and cryosurgery Operative Procedures: ◦ For the LRP procedure, the patient is placed in lithotomy positioning with steep Trendelenburg ▪ Nurses in the OR ensure that the patient maintains a balanced body temperature and positions the patient to prevent injury ▪ The urologist makes one or more small punctures or incisions into the abdomen ▪ A laparoscope with a camera on the end is inserted through one of the incisions while other instruments are inserted into the other incisions ▪ The robotic system may be used to control the movement of the instruments by a remote device ▪ The prostate is removed along with nearby lymph nodes, but perineal nerves are not affected. ◦ The open radical prostatectomy can be performed via several surgical approaches, depending on the patient's desired outcomes and the staging of the disease◦ The transperineal and retropubic (nerve-sparing) approaches are most commonly use ▪ The surgeon removes the entire prostate gland along with the prostatic capsule, the cuff at the bladder neck, the seminal vesicles, and the regional lymph nodes ▪ The remaining urethra is connected to the bladder neck ▪ The removal of tissue at the bladder neck allows the seminal fluid to travel upward into the bladder rather than down the urethral tract, resulting in retrograde ejaculations Postoperative Care: ◦ Nursing interventions include all the typical care for a patient undergoing major surgery ▪ Maintaining hydration ▪ caring for wound drains (open procedure) ▪ managing pai ▪ , and preventing pulmonary complications are important aspects of nursing care. Care of the Patient After an Open Radical Prostatectomy • Encourage the patient to use patient-controlled analgesia (PCA) as needed. • Help the patient get out of bed into a chair on the night of surgery and ambulate by the next day. • Maintain the sequential compression device until the patient begins to ambulate. • Monitor the patient for deep vein thrombosis and pulmonary embolus. • Keep an accurate record of intake and output, including Jackson-Pratt or other drainage device drainage. • Keep the urinary meatus clean using soap and water. • Avoid rectal procedures or treatments. • Teach the patient how to care for the urinary catheter because he may be discharged with the catheter in place. • Teach the patient how to use a leg bag. • Emphasize the importance of not straining during bowel movement. Advise the patient to avoid suppositories or enemas. • Remind the patient about the importance of follow-up appointments with the physician to monitor progress. Pelvic Inflammatory Disease: PID Clinical Diagnostic Criteria for PID: ◦ One or more of the following minimum criteria must be present on pelvic examination to diagnose PID: ▪ Cervical motion tenderness ▪ Uterine tenderness ▪ Adnexal tenderness ◦ The following criteria can improve the specificity of the diagnosis: ▪ Oral temperature > 101°F (> 38.3°C) ▪ Abnormal cervical or vaginal mucopurulent discharge▪ Presence of abundant numbers of white blood cells on saline microscopy of vaginal fluid Elevated erythrocyte sedimentation rate ▪ Elevated C-reactive protein level ▪ Laboratory documentation of cervical infection with gonorrhea or chlamydia ◦ The following test results are the most specific criteria for diagnosing PID: ▪ Endometrial biopsy with histopathologic evidence of endometritis ▪ Transvaginal sonography or magnetic resonance imaging techniques showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or Doppler studies suggesting pelvic infection (e.g., tubal hyperemia) ▪ Laparoscopic abnormalities consistent with PID Treatment: ◦ Antibiotic therapy, self-management measures and rarely surgery. If oral antibiotic therapy is not successful, hospitalization and IV antibiotic therapy is needed. ▪ Option 1 Ceftriaxone (Rocephin) 250 mg IM in a single dose plus Doxycycline 100 mg orally twice per day for 14 days with or without Metronidazole (Flagyl) 500 mg orally twice per day for 14 days ▪ Option 2 Cefoxitin plus 2 g IM in a single dose administered concurrently with probenecid (1 g orally) Doxycycline 100 mg orally twice per day for 14 days with or without Metronidazole 500 mg orally twice per day for 14 days ▪ Option 3 Other parenteral thirdgeneration cephalosporin (e.g., ceftizoxime [Cefizox], cefotaxime [Claforan]) plus Doxycycline 100 mg orally twice per day for 14 days with or without Metronidazole 500 mg orally twice per day for 14 days ◦ Teach: Patient to finish all of the antibiotics and to avoid sexual intercourse until treatment and symptoms are gone. Sexual partners should be treated regardless of their lack of symptoms. ◦ Screening for chlamydia and gonorrhea in young women has been shown to decrease the incidence of PID in high-risk populations STI’S (STD’s) • Syphilis, Herpes, Genital warts, HPV, Candidiasis, Trichomoniasis, chlamydia, Gonorrhea, s/s treatments diagnostics • Syphilis ◦ Syphilis is a complex sexually transmitted disease (STD) that can become systemic and cause serious complications, including death. ◦ The causative organism is a spirochete called Treponema pallidum ◦ The infection is usually transmitted by sexual contact and blood exposure, but transmission can occur through close body contact such as kissing. ◦ Syphilis progresses through four stages: primary, secondary, latent, and tertiary◦ 1st stage: ▪ The appearance of an ulcer called a chancre is the first sign of primary syphilis ▪ It develops at the site of entry (inoculation) of the organism from 10 to 90 days after exposure (3 weeks is average ▪ Chancres may be found on any area of the skin or mucous membranes but occur most often on the genitalia, lips, nipples, and hands and in the mouth, anus, and rectum ▪ During this highly infectious stage, the chancre begins as a small papule ▪ Within 3 to 7 days, it breaks down into its typical appearance: a painless, indurated, smooth, weeping lesion ▪ Regional lymph nodes enlarge, feel firm, and are not painful. ▪ Without treatment, the chancre usually disappears within 6 weeks; however, the organism spreads throughout the body and the patient is still infectious. ◦ 2nd stage: ▪ Secondary syphilis develops 6 weeks to 6 months after the onset of primary syphilis ▪ During this stage, syphilis is a systemic disease because the spirochetes circulate throughout the bloodstream ▪ Commonly mistaken for influenza, manifestations include flu-like symptoms (malaise, lowgrade fever, headache, muscular aches, sore throat) and a generalized rash ▪ There is no typical appearance of this rash except for its presence on the palms and soles of the feet and on mucous membranes ▪ It can appear as diffuse macules (reddish brown), papules (usually less than 5 mm) or pustules, scaly psoriasis-like lesions or gray-white wart-like lesions (condylomata lata) ▪ All of these lesions are highly contagious and should not be touched without gloves ▪ Patchy alopecia on the scalp or facial hair (missing part of the eyebrow, ―moth-eaten‖ appearance) is another symptom ▪ The rash subsides without treatment in 4 to 12 weeks. ◦ 3rd stage: ▪ After the second stage of syphilis, there is a period of latency ▪ Early latent syphilis occurs during the first year after infection, and infectious lesions can recur ▪ Late latent syphilis is a disease of more than 1 year's duration after infection ▪ This stage is not infectious except to the fetus of a pregnant woman ▪ Patients with latent syphilis may or may not have reactive serologic test (e.g., Venereal Disease Research Laboratory [VDRL]) findings) ◦ 4th stage: ▪ Tertiary, or late, syphilis occurs after a highly variable period, from 4 to 20 years ▪ This stage develops in untreated cases and can mimic other conditions because any organ system can be affected▪ Manifestations of late syphilis include: • Benign lesions (gummas) of the skin, mucous membranes, and bones • Cardiovascular syphilis, usually in the form of aortic valvular disease and aortic aneurysms • Neurosyphilis, causing central nervous system symptoms (e.g., meningitis, hearing loss, generalized paresis [weakness]) ◦ Conduct a physical examination, including inspection and palpation, to identify manifestations of syphilis. Wear gloves while palpating any lesions because of the highly contagious treponemes that are present. Observe for and document rashes of any type because of the variable presentation of secondary syphilis. ◦ After the physical examination, the health care provider obtains a specimen of the chancre for examination under darkfield microscope ▪ Diagnosis of primary or secondary syphilis is confirmed if T. pallidum is present. ◦ Blood tests are also used to diagnose syphilis. ▪ The usual screening and/or diagnostic nontreponemal tests are the Venereal Disease Research Laboratory (VDRL) serum test and the more sensitive rapid plasma reagin (RPR). ▪ These tests are based on an antibody-antigen reaction that determines the presence and amount of antibodies produced by the body in response to an infection by T. pallidum. ▪ They become reactive 2 to 6 weeks after infection ▪ VDRL titers are also used to monitor treatment effectiveness ▪ The antibodies are not specific to T. pallidum, and false-positive reactions often occur from such conditions as viral infections, hepatitis, and systemic lupus erythematosus ▪ If a VDRL result is positive, the health care provider requests or the laboratory may automatically perform a more specific treponemal test, such as the fluorescent treponemal antibody absorption (FTA-ABS) test or the microhemagglutination assay for T. palladum (MHA-TP), to confirm the infection Drug Therapy for Syphilis ◦ Benzathine penicillin G given IM as a single 2.4 million-unit dose is the evidence-based treatment for primary, secondary, and early latent syphilis ◦ Patients in the late latent stage receive the same dose every week for 3 weeks ◦ A different regimen, found in the CDC's STD Treatment Guidelines, is recommended for patients who are HIV-infected or pregnant. Genital Herpes Pathophysiology: ◦ Genital herpes (GH) is an acute, recurring, incurable viral diseases ◦ Two serotypes of herpes simplex virus (HSV) affect the genitalia: ▪ type 1 (HSV-1) and type 2 (HSV-2) ▪ Most nongenital lesions such as cold sores are caused by HSV-1, transmitted via oral-oral contact.▪ Historically, HSV-2 caused most of the genital lesions; however, this distinction is academic because the transmission, symptoms, diagnosis, and treatment are nearly identical for the two types ▪ Either type can produce oral or genital lesions through oral-genital or genital-genital contact with an infected person. ▪ HSV-2 recurs and sheds asymptomatically more often than HSV-1 ▪ Most people with GH have not been diagnosed because they have mild symptoms and shed virus intermittently ◦ The incubation period of genital herpes is 2 to 20 days, with the average period being 1 week. Many people do not have symptoms during the primary outbreak. When subsequent outbreaks of genital herpes occur, they are usually more severe and occasionally require hospitalization. ASSESSMENT OF GH ◦ The diagnosis of GH is based on the patient's history and physical examination ◦ Ask the patient if he or she felt itching or a tingling sensation in the skin 1 to 2 days before the outbreak, known as the prodrome ◦ These sensations are usually followed by the appearance of vesicles (blisters) in a typical cluster on the penis, scrotum, vulva, vagina, cervix, or perianal region at the site of inoculation ◦ The blisters rupture spontaneously in a day or two and leave painful ulcerations that can become extensive ◦ Assess for other symptoms such as headaches, fever, general malaise, and swelling of inguinal lymph nodes. ◦ Ask if urination is painful. External dysuria is a painful symptom when urine passes over the eroded areas. Patients with urinary retention may need to be catheterized. ◦ After the lesions heal, the virus remains in a dormant state in the sacral nerve ganglia. Periodically, the virus may activate and symptoms recur. ▪ These recurrences may be triggered by many factors, including stress, fever, sunburn, poor nutrition, menses, and sexual activity. Antiviral drugs are used to treat GH Acyclovir (Zovirax, Avirax image), famciclovir (Famvir), or valacyclovir (Valtrex) may be prescribed Condylomata Acuminata (Genital Warts): Encourage women to have a Pap test annually, starting at age 21 years; after they have had three normal smears, they should have a Pap test every 3 years if no new risk factors are present (e.g., new partner, other STDs) The presence of warts should increase suspicion that the patient may have had exposure to other STDs, which warrants additional testing VACCINES: ◦ Gardasil protection from human papilloma virus cervical cancer, genital warts, and cancer of the anus, vagina, and vulva ▪ Approved for use in male and female patients ages 9–26 ◦ Gardasil 9 same protection as the original Gardasil, plus protection against five additional types of high-risk HPV▪ Approved for use in male patients ages 9–15 and female patients ages 9–26 ◦ Cervarix protects against only the types of HPV that cause cervical cancer ▪ Approved for use solely in female patients ages 9–25 Chlamydia Trachomatis an intracellular bacterium & causative agent of genital chlamydia infections ◦ It invades the epithelial tissues in the reproductive tract. ◦ Incubation is 1 to 3 weeks but the pathogens may be presents for months without producing symptoms. ◦ Chlamydia is a reportable condition to health departments in all states. ◦ 20 – 40% of women who become infected with chlamydia develop Pelvic Inflammatory Disease (PID) Often asymptomatic but some signs and symptoms may include: ◦ *Vaginal or Urethral discharge ◦ *Dysuria (painful urination) ◦ *Frequent Urination ◦ *Pelvic pain ◦ *Irregular bleeding Diagnosis: ◦ Sampling cells from the endocervix, urethra or both. Gold standard is a tissue culture from cervical os or the urethra. ◦ Women ages 25 (sexually active) and younger should be screened yearly and women over 25 with multiple sexual partners should be screened yearly for chlamydia. Treatment: ◦ azithromycin (Zithromax) or doxycycline ◦ Expedited partner therapy (EPT), treating and testing sexual partners for other STD’s shows signs of reducing chlamydia infection rates. Gonorrhea: a sexually transmitted bacterial infection that occurs in both men and women ◦ The causative organism is Neisseria Gonorrhoeae, a gram negative intracellular dipococcus. ◦ It is transmitted by direct sexual contact with mucosal surfaces – (vaginal intercourse, orogenital contact, or anogenital contact) Gonorrhea bacteria can grow in the warm, moist areas of the reproductive tract, including: ◦ the cervix (opening to the womb) ◦ uterus (womb) ◦ fallopian tubes (egg canals) in women ◦ urethra (the tube that carries urine from the bladder outside the body) in women and men ◦ The bacteria can also grow in the mouth, throat, and anus The first symptoms of gonorrhea may appear 3 to 10 days after sexual contact with an infected person ◦ The disease can be present without symptoms and can be transmitted or progress without warning ◦ In women, ascending spread of the organism can cause pelvic infection (pelvic inflammatory disease [PID]), endometritis (endometrial infection), salpingitis (fallopian tube infection), and pelvic peritonitis ◦ Rare complications of gonorrhea in adults include arthritis, meningitis, hepatitis, and disseminated infection The infection can be asymptomatic in both men and women, but women have asymptomatic, or ―silent,‖ infections more often than do men. ◦ If symptoms are present, men usually notice dysuria and a penile discharge that can be either profuse, yellowish green fluid or scant, clear fluid. ◦ The urethra is most commonly affected, but infection can extend to the prostate, the seminal vesicles, and the epididymis. ◦ Men seek curative treatment sooner, usually because they have symptoms, and thereby avoid some of the serious complications. ◦ Women may report a change in vaginal discharge (yellow, green, profuse, odorous), urinary frequency, or dysuria. ◦ The cervix and urethra are the most common sites of infection. ◦ Anal manifestations may include itching and irritation, rectal bleeding or diarrhea, and painful defecation ◦ Assess the mouth for a reddened throat, ulcerated lips, tender gingivae, and lesions in the throat If fever ccurs, this may be a sign of an ascending (PID or epididymitis) or systemic infection (disseminated gonococcal infection). ◦ Symptoms could include joint or tendon pain, either in a single joint or as migratory arthralgias, especially of the knees, elbows, fingers or toes, and a rash usually on the palms and soles. The rash can be pustular or maculopapula Pelvic Floor Dysfunction cystocele: ◦ a protrusion of the bladder into the vaginal wall ◦ leading to urinary tract infection and urinary elimination problems, including stress incontinence. Rectocele: ◦ protrusion of the rectum through a weakened vaginal wall◦ leading to constipation, hemorrhoids, fetal impaction, and feelings of rectal or vaginal fullnessnary Incontinence Erectile Dysfunction Sexual and Gender Identity; Care of the transgender patient Concept of Immunity and Cellular Regulation: EXAM 2 & 3 Notes from conference Box 2-1; page 50 page 56 TNM grading scale ◦ understand how to answer questions related to TNM ◦ C ancer Markers ▪ CEA – lung and colon cancer ▪ PSA – prostate cancer ▪ positive tumor markers do not prove you have cancer ▪ BIOPSY IS THE NUMBER ONE REASON TO DIAGNOSE CANCER page 97 – chart for leukemia (look at picture made) ◦ primary forms of leukemia is correct ◦ AML is most common in older adults ◦ ALL – younger adults and children – rapid progression ◦ CML – philadelphia ◦ CLL often requires no treatment – depending on rate of progresssion Lymphomas – look at picture made ◦ non hodgekin – EBV and Burkitt lymphoma ◦ hodgekin – reed sternburg cell know that colorectal cancer ◦ look at chart page 91 ◦ risk factors Colitis and Chrons and age are risk factors for colorectal cancer ◦ rectal bleeding is a big sign for colorectal cancer ◦ other s/s: change in bowel habits, familal polypoisious, weight loss lung cancer ◦ know chart on 109 ◦ small cell (oat cell) carcinoma ▪ SIADH – hanging onto to your fluid; can not get rid of it – cushings syndrome and thrombophlebitis ◦ non small cell ◦ blood in sputum Brachytherapy ◦ lecture notes◦ nurses taking care of patients who is getting this should NOT BE PREGNANT ◦ NO X-RAYS TO PREGNANT WOMEN ◦ small pellet of radioactive material that is placed into the cancer or into the nearby airway ◦ very dangerous to bystanders for pts getting this treatment what is the difference between benign and malignant ◦ NORMAL: ▪ SLOW ▪ fibronectin says hey you are too close to me stop growing – helps keep that tightly together ▪ function ◦ BENIGN: ▪ CONTINUOUS AND SLOW; ▪ LOCALIZED ▪ tight adherence Function ◦ MALIGNANT: ▪ AGGRESSIVE GROWTHS ▪ RAPID CELL DIVISION ▪ METASTIZE ▪ INVADE/DESTROY SURROUNDING TISSUE ▪ NO Fibronectin – making them loose ▪ NO FUNCTION ▪ MIGRATE TLS – tumor lysis syndrome ◦ intracellular contents leak into circulation causing ▪ hyperkalemia arrythmias, dysrhythmias ▪ hyperuricemia ▪ hyperphosphatemia superior vena cava syndrome ◦ upper ext. edema ◦ postural hypotension ◦ dizziness, pallor, clamminess ◦ swelling of face – SOB ◦ check pulse ox, BP, and respiratory status – airway too cancer prevention cancer stages 7 signs and symptoms of cancer eye part of test 10-21 IOP snellen’s chart – jaeger for up close vision problems – ishy hara chart is for color blindnesschal do not give tropicamide (a dilation eye med) to someone who has increased IOP trachoma – chlamydia trachomatis chemical splash – irrigate check ph for chemical irritant to eye fluorescent light for trauma to eye to see if abrasion has occurred no cornea transplant if person has cancer at time of death – CANCER IS BIG ONE (small cell lung cancer) retinal detachment – DO NOT DO THINGS THAT INCREASE IOP know vocabulary words in notes glaucoma prostaglandins is given for glaucoma Gonioscopy – TO TEST WHICH TYPE OF GLAUCOMA ◦ know difference between the two ◦ one is chronic – open ▪ not a medical emergency ▪ slightly open canal of schlemn ◦ one is acute – closed ▪ medical emergency ▪ cornea starts to flatten and iris bulges ▪ avoid anticholinerics and mydriatics like tropicamide which cause pupil to dilate > IOP ear part kidney is something you look for if you have ear problems sensory hearing losses – vestibuochlear nerve 8 is damaged never irrigate ear infections – always look in ear before ear drops; warm solutions ototoxic – aminoglycoside antibiotics CAUTION s/s of cancer Changes in bowel or bladder habits. A sore that does not heal. Unusual bleeding or discharge. Thickening or lump in the breast or any other part of the body. Indigestion or difficulty swallowing. Obvious change in a wart or mole. Nagging cough or hoarseness Benign vs. Cancer cells: Grading and staging of cancer TNM: What does Tissue of origin mean with cancer? s/s of different cancers:EXAM 2 LECTURE NOTES – MADISON’S VERSION Principles of Inflammation and Immunity Overview Immunity: protection from illness or disease that is maintained by the body’s physiologic defense mechanisms ◦ this protection requires interaction of immunity and inflammation WORKING TOGETHER to control infection and other problems caused by harmful microorganisms or altered cells Self versus Non-Self Non-self proteins and cells: ◦ infected body cells ◦ cancer cells ◦ cells from other people ◦ invading organisms recognizing self vs. non-self: self tolerance ◦ this prevents immunity from harming healthy body cells ◦ possible because of different proteins on cell membranes This is where you see your HLAs (human leukocyte antigens) come into play ◦ each person’s cells have unique surface proteins that are specific to that person (HLAs) ◦ serve as ―universal product code‖ ◦ your HLAs are recognized as ―foreign‖ or non self by the immune system of someone else ▪ YOUR cell-surface proteins are non self to another adults immune system – they are antigens – proteins capable of stimulating an immunity response!! ◦ these HLAs are key for recognition and self tolerance ▪ immune system cells constantly come into contact w/other body cells and with any invader that enters the body at each encounter – immune system cells compare the surface protein HLAs to determine whether the encountered cell belongs to the body if they match – not attacked if they do not match – it is non self or foreign ◦ immune system cell takes action to neutralize, destroy, or eliminate foreign invader a key element for recognition of non self by cells involved in general immunity and those involved in specific immunity is the presence of TOLL-LIKE RECEPTORS (TLRs) on these cells ◦ known to be present on immune system cells of humans ◦ protective purpose – interact with the surface of any invading organism ◦ allows recognition that is non self so actions are taken to rid the invader from the body ◦ TLRs also help immune system cells recognize damaged or unhealthy cells Organization of the Immune System The three processes needed for human protection through immunity: ◦ inflammation ◦ antibody-mediated immunity (AMI) ◦ cell-mediated immunity (CMI) optimal function of all three divisions is necessary for complete immunity Chart describing immune functions of specific leukocytes – will talk about each section in detail Variable Leukocyte Function Inflammation Neutrophil Nonspecific ingestion and phagocytosis of microorganisms and foreign protein – Macrophage Nonspecific recognition of foreign proteins and microorganisms; ingestion and phagocytosis. Assist with antibody-mediated immunity and cell-mediated immunity – Monocyte Destruction of bacteria and cellular debris; matures into MACROPHAGE – Eosinophil Releases vasoactive amines during allergic reactions to limit these reactions – Basophil Releases histamine and heparin in areas of tissue damageVariable Leukocyte Function Antibodymediated immunity B-lymphocyte Becomes sensitized to foreign cells and proteins with the assisstance of macrophages and helper/inducer T-cells – Plasma cell Secretes immunoglobulins (antibodies) in response to the presence of a specific antigen – Memory cell Remains sensitized to a specific antigen and can secrete increased amounts of immunoglobulins (antibodies) specific to the antigen on re-exposure Variable Leukocyte Function Cell-mediated immunity Helper/inducer Tcell Enhances immune activity of all parts of general and specific immunity through secretion of various factors, cytokines, and lymphokines – Cytotoxic/cytolytic cell Selectively attacks and destroys non self cells, including virally infected cells, grafts, and transplanted organs – Natural killer cell Nonselectively attacks non self cells, especially body cells that have undrgone mutation and become malignant; also attacks grafts and transplanted organs GENERAL IMMUNITY – INFLAMMATION nonspecific – also called innate-native immunity or natural immunity with inflammation – general immunity provides IMMEDIATE protection ◦ against the effects of tissue injury and invading foreign proteins innate-native immunity ◦ any natural protective feature of a human ◦ barrier to prevent organism from entering body ◦ can attack organism that have already entered body this type of immunity CAN NOT be transferred from one adult to another – not an adaptive response Lines that compose general immunity: ◦ 1st line ▪ skin ▪ mucosa ▪ antimicrobal on the skins (normal flora) ◦ 2nd line ▪ Inflammation (inflammatory response) ▪ complement ▪ natural killer cells General immunity and inflammation differ from specific immunity IN TWO WAYS: ◦ inflammatory protection is immediate but short term ▪ it does not provide true immunity on repeated exposure to the same organisms ◦ inflammation is a nonspecific body defense to invasion or injury ▪ can be started quickly by almost any event – regardless of where it occurs/what caused it Infection – usually accompanied by inflammation; however, inflammation can occur without infection ◦ inflammation does not always mean that an infection is present ◦ inflammation seen where?: ▪ w/out infection can be caused by: joint sprains MI blister formation ▪ Non-infectious invasion: allergic rhinits contact dermatitis ▪ infection: otitis media appendicitis viral hepatitis Cell types involved in inflammation leukocytes (WBCs) ◦ neutrophils ▪ mature neutrophils make up between 55%-70% of normal total WBC count ▪ come from stem cells – complete the maturation process in bone marrow ▪ provides protection after invaders, especially BACTERIA, enter the body ▪ they destroy invaders by phagocytosis and enzymatic digestion ▪ THIS IS THE CELL WHERE YOU INDICATE A LEFT SHIFT the segmented neutrophil (mature cells at the far right) is no longer the most numerous type in circulation – more of the circulating cells are bands – the less mature cell type found farther left on the neutrophil pathway a left shift indicates: ◦ patients bone marrow cannot produce enough mature neutrophils (segs) ◦ cannot keep the pace w/continuing infection ◦ release immature neutrophils into the blood (bands) ◦ the bands are of minimal benefit ▪ not capable of phagocytosis ◦ also known as bandemia (immature neutrophils in the blood) ◦ macrophages ▪ monocytes move from the blood into body tissues where they mature into macrophages ▪ liver, spleen, and intestinal tract contain large # of these cells ▪ helps stimulate immediate inflammatory responses ▪ also stimulates the longer-lasting immune response of antibody-mediated immunity (AMI) and cell-mediated immunity (CMI) ▪ function: phagocytosis, repair, antigen presenting/processing, secretion of cytokines for immune system control ▪ inflammatory function: PHAGOCYTOSIS ◦ eosinophils ▪ contain many vasoactive chemicals ▪ most active against infestations of parasitic larvae ▪ also limits inflammatory reactions ◦ basophils ▪ these cause s/s of inflammation ▪ acts on blood vessels w/basophil chemicals (vasoactive amines) histamine is one of the vasoactive amines for example** focus on this one others include; heparin, serotonin, and leukotrines (if you wanted to know) ▪ when ALLERGENS bind to IgE on the basophils basophil membrane opens releases the vasoactive amines into blood most of the vasoactive amines act on smooth muscle and blood vessels walls **histamine (which is one of the vasoactive amines released) dilates arterioles and constricts small veins ◦ slowing blood flow and decreasing venous return ◦ causing blood to collect in capillaries and arterioles ▪ basophils stimulates both general inflammation and the inflammation of allergic reactions additional cell type important in inflammation ◦ mast cells – release histamine ▪ have binding sites for the stems of IgE molecules ▪ are involved in allergic reactions ▪ respond to inflammatory products released by T-lymphoctes▪ tissue mast cells maintain and prolong inflammation and allergic reactions Anti-microbial substances: ◦ Some books include the complement system, Interleukins, Interferons, lysozymes found in sweat saliva and tears (there are many many more) ◦ Basically these are proteins made by tissues or cells in the body that…The complement system is a part of innate immunity ▪ activate the immune system ▪ promote resistance to viruses ▪ oxidize bacteria ▪ inhibit growth ▪ lyse bacteria cell walls ▪ ect….. complement system: ◦ can kill bacteria and participate in the inflammatory process ◦ Group of proteins that are activated in sequential order to provide a link to the humoral response ◦ IgG and Igm are responsible for activating the complement cascade ◦ Complement assays diagnose immunodeficiency and autoimmune disease Interferons: ◦ proteins that come from virus laden cells and lymphocytes that help with resistance to the virus. Interleukins: ◦ proteins that come from macrophages and lymphocytes that cause fever and activation of the immune system Phagocytosis: key process in inflammation neutrophils and macrophages – most efficient at phagocytosis 7 STEPS:◦ exposure and invasion: ▪ first step in injury or invasion ▪ leukocytes engage in phagocytois and stimulate inflammation present in blood and ECF ◦ attraction: ▪ brings the WBC into direct contact with target (antigen, invader, foreign protein) ▪ damaged tissues – secrete chemotaxins which do the following: attracts neutrophils and macrophages release debris that binds to the surface of invading proteins ◦ adherence ▪ binds the phagocytic cell to the surface of target ▪ opsonins – substances that increase contact with the cell w/target by coating the target cell during inflammation coating the target makes it easier for phagocytic cells to stick to the antigen substances that are opsonins ◦ dead neutrophils ◦ antibodies ◦ activated complement components ◦ recognition: ▪ when phagocytic cell sticks to target cell recognizes it as non self phagocytic cell examines the HLAs (universal product codes) or whatever they encounter ▪ phagocytic cells only START phagocytosis when the target cell is RECOGNIZED as non self or foreign debris ◦ cellular ingestion: ▪ engulfment of the target cell (phagocytosis)◦ degradation: ▪ final step ▪ enzymes in phagosome digest engulfed target Sequence of inflammation five cardinal symptoms of inflammation: ◦ warmth ◦ redness ◦ swelling ◦ pain ◦ decreased function 3 stages ◦ stage 1: ▪ vascular response ◦ stage 2: ▪ cellular exudate part of response ◦ stage 3: ▪ features tissue repair and replacement SPECIFIC IMMUNITY – THIS INCLUDES ANTIBODY-MEDIATED IMMUNITY AND CELL MEDIATED IMMUNITY antibody-mediated immunity (AMI): our humoral immunity Uses antigen-antibody interactions to neutralize, eliminate, or destroy foreign proteins. ◦ Antibodies are produced by sensitized B-lymphocytes (B-CELLS) ◦ b-cells become sensitized to a specific foreign protein (antigen) and produce antibodies directed SPECIFICALLY AGAINST THAT ANTIGEN ◦ b-cells have the most direct roll in AMI T-lymphocytes and macrophages (main players in cell mediated immunity) work with the B-cells of our humoral immunity to generate antigen-antibody interactions describing the antigen-antibody interaction: the body learns to make enough of any specific antibody to provide long-lasting immunity against specific organism or toxins antigen recognition is the recognition of the antigen by unsensitized B-cells ◦ this action requires the help of T-Cells and macrophages recognition is started by the macrophages of innate immunity ◦ macrophages recognize the invading antigen as non self and attach to antigen ◦ once attached – macrophages may now present the attached antigen (foreign protein) to the helper/inducer T-cells The CD4 cell (your helper/inducer T-cells) and the macrophages TOGETHER process the antigen to expose the antigens recognition sites (universal product code) after processing the antigen ◦ CD4 T cell bring antigen into contact with the B-CELL ▪ now the B-cell is able to recognize the antigen as non self – now sensitization can occur the b-cell is now ―sensitized‖ to this antigen ◦ an un-sensitized b-cell can only be sensitized once (SO TO ONLY ONE TYPE OF ANTIGEN) immediately after it is sensitized ◦ b-cell divides into two types of b-lymphocytes (each one remaining sensitized to that specific agent) ▪ plasma cell starts immediately to produce antibodies against the sensitizing antigen antibodies are produced by plasma cells produces antibodies specific only to the antigen that originally sensitized the parent b-cell ▪ memory cell antigen presenting cells/MHC2 a sensitized b-cell but DOES NOT PRODUCE antibodies until the next exposure to the same antigen sustained immunity (memory) provides us with long-lasting true immunity to a specific antigen ◦ this results from memory b-cells made during lymphocyte sensitization Acquiring antibody-mediated immunity Antibody-mediated immunity (AMI) ◦ also known as Acquired immunity ◦ is a type of adaptive immunity in which a person's body learns to make as an adaptive response to invasion by organisms or foreign proteins. ◦ Adaptive immunity occurs: ▪ either naturally or artificially through lymphocyte responses ▪ can be either active or passive ▪ look at chart above ACTIVE IMMUNITY: ◦ occurs when antigens enter a person's body and it responds by making specific antibodies against the antigen ◦ this type of immunity is active because the body takes an active part in making antibodies. ◦ active immunity occurs under natural or artificial conditions ◦ Natural ACTIVE immunity:▪ immunity occurs when an antigen enters the body naturally without human assistance and the body responds by actively making antibodies against that antigen (e.g., influenza A virus) ▪ Usually, the invasion that triggers antibody production also causes the disease. However, processes occurring in the body at the same time as infection create immunity to that antigen. Thus the person will not become ill after a second exposure to the same antigen. Natural active immunity is the most effective and the longest lasting. ◦ Artificial ACTIVE immunity: ▪ protection developed by vaccination or immunization ▪ This type of immunity is used to prevent serious and potentially deadly illnesses (e.g., tetanus, diphtheria, polio) ▪ Small amounts of specific antigens are placed as a vaccination into a person ▪ The person's immune system responds by actively making antibodies against the antigen Because antigens used for this procedure have been specially processed to make them less likely to grow in the body (attenuated), this exposure usually does not cause the disease Artificial active immunity lasts many years, although repeated but smaller doses of the original antigen are required as a ―booster‖ to retain the protection. PASSIVE IMMUNITY: ◦ occurs when the antibodies against an antigen are transferred to a person's body after first being made in the body of another person or animal ◦ Because these antibodies are foreign to the receiving person, they are recognized as non-self and eliminated quickly ▪ For this reason, passive immunity provides only immediate, short-term protection against a specific antigen ▪ It is used when a person is exposed to a serious disease for which he or she has little or no actively acquired immunity ▪ Instead, the injected antibodies are expected to inactivate the antigen. ◦ Artificial PASSIVE immunity: ▪ may be used to prevent disease or death for patients exposed to rabies, tetanus, and poisonous snake bites. ◦ Natural PASSIVE immunity:▪ occurs when antibodies are passed from the mother to the fetus via the placenta or to the infant through colostrum and breast milk. REMEMBER: ◦ AMI (antibody-mediated immunity) works with inflammation to protect against infection ◦ it provides effective long-lasting immunity ONLY when the actions are combine with those of CMI (cell-mediated immunity) Cell-mediated immunity (CMI): also known as cellular immunity Cell mediated immunity is responsible for the mediation of transplant rejection Cell-mediated immunity (CMI), or cellular immunity, involves many white blood cell (WBC) actions and interactions. CMI is another type of adaptive or acquired true immunity that is provided by lymphocyte stem cells that mature in the secondary lymphoid tissues of the thymus and pericortical areas of lymph nodes. Certain CMI responses influence and regulate the activities of antibodymediated immunity (AMI) and inflammation by producing and releasing cytokines. For total or full immunity, CMI must function optimally. involve your T-cells 2 types of T cells: ◦ Helper/Inducer t-cells ◦ cytotoxic/cytolytic (will kill infected cells or abnormal cell) ◦ natural killer cells (NK cell) also contributes to CMI T-lymphocytes are made in the bone marrow but mature in the thymus T-lymphocytes recognize a specific histocompatibility complex (a group of proteins that participate in auto immune recognition and tissue rejection) ◦ bind them to elicit an immune response Protein markers on the surface of T-cell ◦ help define specific function receptor sites T-lymphocytes help protect the body from ◦ bacteria, viral and fungal infections (Humoral immunity is considered the long term process) T-Helper cells ◦ ―raises the Flag‖ and cries out ―help‖ ◦ Dendritic cells ( a type of phagocytic cell) works very well with helper t-cells to raise that alarm ◦ Dendritic cell will have a MHC 2 complex and present it to the t-helper cell with a specific receptor to the MHC2 complex on the outside of this phagocytic dendritic cell◦ T-helper cells get specific the same way B-cells doc-- by making many many many differentiated copies of itself ◦ Some become memory T-cells (looks just like the parent) and some become effector T-cells ▪ Effector T-cells start releasing cytokines when they want to sound the ―alarm‖ ▪ The cytokines enter the immune cells that have been activated already and makes them proliferate (divide) more (b-cells and cytotoxic-cells) ▪ ** Remember some B-cells will also have that same MHC2 complex on the outside. This is a double check system and prevents mutated immune cells from attacking healthy cells. Cell Types Involved in Cell-Mediated Immunity the WBCs with the most important roles in CMI include several specific T-lymphocytes (T-cells) along with a special population of cells known as natural killer (NK) cells ◦ T-cells have a variety of subsets, each of which has a specific function. Different T-cell subsets can be identified by the presence of ―marker proteins‖ (antigens) on the cell membrane's surface ◦ More than 200 different T-cell proteins have been identified on the cell membrane, and some of these are commonly used clinically to identify specific cells ◦ Most T-cells have more than one antigen on their cell membrane. The names used to identify specific T-cell subsets include the specific membrane antigen and the overall actions of the cells in a subset ◦ The three T-lymphocyte subsets that are critically important for the development and continuation of CMI are… ▪ helper/inducer T-cells ▪ suppressor T-cells ▪ cytotoxic/cytolytic T-cells ▪ An additional cell, the natural killer cell, although not a true T-cell, also contributes to CMI Helper/inducer T-cells: ◦ have the T4 protein on their membranes ◦ these cells are usually called T4+ cells or TH cells – most correct name for helper/inducer T-cells is CD4+ ◦ easily recognize self cells versus non-self cells ▪ When they recognize non-self (antigen): ▪ helper/inducer T-cells secrete cytokines that can enhance the activity of other WBCs and increase overall immune function ▪ These cytokines increase bone marrow production of stem cells and speed up their maturation ▪ Thus helper/inducer T-cells act as organizers in ―calling to arms‖ various squads of WBCs involved in inflammatory, antibody, and cellular protective actions Suppressor T-cells: ◦ have the T8-lymphocyte antigen on membrane surfaces ◦ These cells are commonly called T8+ cells, CD8+ cells, or TS-cells ◦ help regulate CMI◦ prevent hypersensitivity (immune overreactions) on exposure to non-self cells or proteins ▪ This function is important in preventing the formation of antibodies directed against normal, healthy self cells, which is the basis for many autoimmune diseases. ◦ The suppressor T-cells secrete cytokines that have an overall inhibitory action on most cells of the immune system ◦ Suppressor T-cells have the opposite action of helper/inducer T-cells ▪ For optimal function of CMI, then, a balance between helper/inducer T-cell activity and suppressor T-cell activity must be maintained ▪ This balance occurs when the helper/inducer T-cells outnumber the suppressor T-cells by a ratio of 2:1 When this ratio increases ◦ indicating that helper/inducer T-cells vastly outnumber the suppressor cells ◦ overreactions can occur, some of which are tissue damaging as well as unpleasant When the helper/suppressor ratio decreases ◦ indicating fewer-than-normal helper/inducer T-cells ◦ immunity is suppressed and the person's risk for infections increases Cytotoxic/cytolytic T-cells: ◦ also called TC-cells – because they have the T8 protein present on their surfaces, they are a subset of suppressor cells ◦ Cytotoxic/cytolytic T-cells destroy cells that contain a processed antigen's human leukocyte antigens (HLAs) ▪ This activity is most effective against self cells infected by parasites, such as viruses or protozoa. ◦ Parasite-infected self cells have both self HLA proteins (universal product code) and the parasite's antigens on the cell surface ▪ This allows the person's immune system cells to recognize the infected self cell as abnormal ▪ the cytotoxic/cytolytic T-cell can bind to it, punch a hole, and deliver a ―lethal hit‖ of enzymes to the infected cell, causing it to lyse and die. Natural killer (NK) cells: ◦ also known as CD16+ cells ◦ very important in providing CMI ◦ The actual site of NK cell differentiation and maturation is unknown, and it is not a true T-cell subset ◦ NK cells have direct cytotoxic effects on some non-self cells without first being sensitized ▪ They conduct ―seek and destroy‖ missions in the body to eliminate non-self cells. ◦ NK cells are most effective in destroying unhealthy or abnormal self cells ▪ The non-self cells most often harmed by NK cells are cancer cells and virally infected body cells Cytokines: Cell-mediated immunity (CMI) regulates the immune system by the production and activity of cytokines Cytokines are small protein hormones produced by the many WBCs (and some other tissues) ◦ Cytokines made by the macrophages, neutrophils, eosinophils, and monocytes are called monokines ◦ Those produced by T-cells are called lymphokines ◦ In addition, we now know that many other body cell types can produce and respond to cytokines. Cytokines work like hormones: ◦ one cell produces a cytokine – which in turn exerts its effects on other cells of the immune system and on other body cells ▪ The cells responding to the cytokine may be located close to or remote from the cytokinesecreting cell ▪ Thus cytokines act like ―messengers‖ that tell specific cells how and when to respond ◦ The cells that change their activity when a cytokine is present are ―responder‖ cells ▪ For a responder cell to respond to the presence of a cytokine – the responder cell must have a specific receptor to which the cytokine can bind ◦ Once the cytokine binds to its receptor, the responder cell changes its activity Cytokines control many inflammatory and immune responses and are controlled by interactions with other systems, especially the nervous system ◦ Cytokines include the interleukins (ILs), interferons (IFNs), colony-stimulating factors, tumor necrosis factors (TNFs), and transforming growth factors (TGFs) (do not have to know all of them...) ◦ There are many cytokines, and cytokine classification is undergoing changes ▪ Some are considered ―proinflammatory‖ and increase the actions of natural immunity (inflammation) ** the biggest thing to know about cytokines is that: neutrophils activate cytokines it is a big response to the inflammatory response CYTOKINE ACTIONS Pro-inflammatory Cytokines Interleukin-1 (IL-1) Induces fever Stimulates production of prostaglandins Increases growth of CD4+ T-cells Interleukin-2 (IL-2) Increases growth and differentiation of T-lymphocytes Enhances natural killer cell activity against cancer cells Interleukin-6 (IL-6) Stimulates liver to produce fibrinogen and protein C Increases rate of bone marrow production of stem cells Increases numbers of sensitized B-lymphocytes Tumor Necrosis Factor (TNF) Induces fever Major cytokine involved in rheumatoid arthritis damage Major cytokine involved in the acute inflammatory response to infectiousCYTOKINE ACTIONS bacteria and starts many of the systemic complications of severe infection or sepsis Participates in graft rejection Induces cell death Stimulates delayed hypersensitivity reactions and allergy Growth Factors Granulocyte Colony-Stimulating Factor (G-CSF) Increases numbers and maturity of neutrophils Granulocyte-Macrophage ColonyStimulating Factor (GM-CSF) Increases growth and maturation of myeloid stem cells Erythropoietin Increases growth and differentiation of erythrocytes Thrombopoietin Increases growth and differentiation of platelets ** know that cytokines are part of adaptive immunity Transplant Rejection Natural killer (NK) cells and cytotoxic/cytolytic T-cells also destroy cells from other people or animals ◦ Although this action is normal and is usually helpful – it is also responsible for rejection of tissue grafts and transplanted organs (also termed grafts)◦ Because the solid organ transplanted into the recipient is seldom a perfectly identical match of human leukocyte antigens (unless the organ is obtained from an identical sibling) between the donated organ and the recipient host… ▪ the patient's immune system cells recognize a newly transplanted organ as non-self ▪ Without intervention, the recipient's immune system starts inflammatory and immunologic actions to destroy or eliminate these non-self cells This activity causes rejection of the transplanted organ ◦ Rejection of transplanted solid organs and other grafts is a result of a complex series of responses that change over time and involve different components of the immune system ▪ Rejection can be hyperacute, acute, or chronic. Hyperacute Rejection: ◦ begins immediately on transplantation and is an antibody-mediated response ▪ Antigen-antibody complexes form in the blood vessels of the transplanted organ ▪ The recipient's (host's) blood has pre-existing antibodies to one or more of the antigens (including blood group antigens) present in the donated organ ▪ The antigen-antibody complexes adhere to the lining of blood vessels and activate complement ▪ The activated complement in the blood vessel linings triggers the blood clotting cascade, causing small clots to form throughout the new organ Widespread clotting occludes blood vessels and leads to ischemic necrosis, inflammation with phagocytosis of the 287 necrotic blood vessels, and release of lytic enzymes into the new organ These enzymes cause massive cellular destruction within the transplanted organ and graft loss. ◦ Hyperacute rejection occurs mostly in transplanted kidneys but is less common now as a result of greater efforts in HLA matching ▪ The patients at greatest risk for hyperacute rejection are those who have received... donated organs of an ABO blood type different from their own have received multiple blood transfusions at any time in life before transplantation have a history of multiple pregnancies or have received a previous transplant. ◦ The manifestations of hyperacute rejection: ▪ are apparent within minutes of attachment of the donated organ to the recipient's blood supply ▪ The process cannot be stopped once it has started ▪ the rejected organ is removed as soon as hyperacute rejection is diagnosed. Acute Rejection: ◦ Acute rejection first occurs within 1 week to 3 months after transplantation and may occur sporadically after that ◦ Two mechanisms are responsible:▪ The first mechanism is antibody mediated and results in vasculitis within the transplanted organ This reaction differs from hyperacute rejection in that blood vessel necrosis (not occlusion) leads to organ destruction ◦ The second mechanism is cellular ▪ The recipient's cytotoxic/cytolytic T-cells and NK cells enter the transplanted organ through the blood, penetrate the organ cells, start an inflammatory response, and cause lysis of the organ cells ◦ Diagnosis of acute rejection is made by laboratory tests that show impaired function of the donated organ and by biopsy of the donated organ ◦ Manifestations of acute rejection vary with each patient and with the specific organ transplanted ▪ For example, when acute rejection occurs in a transplanted kidney, the patient usually has some tenderness in the kidney area and may have other general manifestations of inflammation ◦ An episode of acute rejection after solid organ transplantation does not automatically mean that the patient will lose the new organ ▪ Drug management of the recipient's immune responses at this time may limit the damage to the organ and allow the graft to be maintained. Chronic Rejection: ◦ The origin of chronic rejection is similar to chronic inflammation and scarring ▪ The smooth muscles of blood vessels overgrow and occlude the vessels ▪ The donated organ tissues are replaced with fibrotic, scarlike tissue Because this fibrotic tissue is not organ tissue, the transplanted organ's function is reduced in proportion to the amount of normal tissue that is replaced by fibrotic tissue ◦ This type of reaction is long-standing and occurs continuously as a response to chronic ischemia caused by blood vessel injury ◦ The results of chronic rejection are unique to different transplanted organs ▪ For example, in transplanted lungs, chronic rejection thickens small airways ▪ In transplanted livers, chronic rejection destroys bile ducts ▪ In transplanted hearts, this process is called accelerated graft atherosclerosis (AGA) and is the major cause of death in patients who have survived 1 or more years after heart transplantation ◦ Although good control over the recipient's immune function can delay this type of rejection, the process probably occurs to some degree with all transplanted solid organs obtained from donors who are not identical siblings of the recipients ◦ Because the fibrotic changes are permanent ▪ there is no cure for chronic graft rejection ▪ When the fibrosis increases to the extent that the transplanted organ can no longer function – the only recourse is retransplantation. Management of Transplant Rejection ◦ Rejection of transplanted solid organs involves all three components of immunity▪ although cell-mediated immune (CMI) responses contribute the most to the rejection process. Usually, inflammation and immunity are protective and helpful responses ◦ However, when inflammation or immunity is prolonged or excessive or occurs at an inappropriate time, normal tissues are damaged ▪ These responses are ―overreactions‖ to invaders and foreign antigens and are known as hypersensitivity or allergic responses ◦ When these responses fail to recognize and protect self cells, normal body tissues are attacked and harmed. ▪ This type of reaction is known as an autoimmune response. ▪ Hypersensitivity and autoimmune responses can severely damage cells, tissues, and organs ANTIBODY CLASSIFICATION PICTURE – helps answer study guide question Reduci ng the risk of cancer: Screeni ng recom mendat ions E n d o m e t r i a l c a n c e r :◦ the most common gynecologic malignancy and grows slowly and has a good prognosis ◦ Adenocarcinoma is the most common type of tumor ◦ Stages: ▪ Stage I endometrial cancer is confined to the endometrium. – total hysterectomy and BSO ▪ Stage II cancer also involves the cervix.—radial hysterectomy ▪ Stage III reaches the vagina or lymph nodes. ▪ Stage IV endometrial cancer has spread beyond the pelvis. ◦ The main symptom of endometrial cancer is postmenopausal bleeding ◦ Some women also have ▪ watery ▪ bloody vaginal discharge ▪ low back or abdominal pain ▪ and low pelvic pain (caused by pressure of the enlarged uterus) ◦ Risk factors for endometrial (uterine) cancer ▪ Women in reproductive years ▪ family history of cancer ▪ diabetes ▪ hypertension ▪ obesity ▪ uterine polyps ▪ late menopause ▪ nulliparity ▪ smoking ▪ and tamoxifen (Nolvadex) given for breast cancer ◦ Transvaginal ultrasound and endometrial biopsy are the gold standard tests to determine the presence of endometrial thickening and cancer ◦ Surgical removal of the tumor and lymph nodes and cancer staging of the tumor with adjacent lymph nodes are the most important interventions for endometrial cancer – Radiation and chemotherapy are typically used postoperatively ▪ Women with stage II disease may use brachytherapy radiation to prevent recurrence of vaginal cancer and improve survival ◦ Pap tests sample cells from the cervix as a screening test for cervical cancer. ◦ The squamo-columnar junction is the transformation zone where most cell abnormalities occur ◦ Premalignant changes are described as continuum from atypic (suspicious) to cervical intraepithelial neoplasia (CIN) to carcinoma in situ (CIS), which is the most advanced premalignant change ◦ Most cervical cancers arise from the squamous cells on the outside of the cervix.◦ Risk factors for cervical cancer: ▪ Girls and young women ▪ infection with HPV ▪ multiparity ▪ smoking ▪ younger than 18 at first intercourse ▪ multiple sex partners ▪ african americans ▪ oral contraceptive use ▪ history of STDs ▪ obesity ▪ family history of cancer ▪ HIV/AIDS ▪ lower socioeconomic status ▪ intrauterine exposure to DES ◦ The human papilloma virus (HPV) vaccine provides some protection against the high risk HPV types that are responsible for most cervical cancers. ▪ Gardasil is indicated for ages 9 through 26. It is also given for boys and men (9 through 26 years of age) to prevent genital warts because it protects against the 6 and 11 HPV strains and to prevent anal cancer, which is caused by HPV strains 16 and 18 ▪ Cervarix protects girls and women ages 9 through 25 years against infection for HPV strains 16 and 18 to prevent cervical cancer. ▪ The most frequent side effects are related to local irritation from the injections (e.g., pain, redness) – Other common side effects include nausea, vomiting, dizziness, headache, and diarrhea. ◦ AGES for PAP smear and HPV testing on diagnostics page – 1st few pages ◦ As the cancer grows: ▪ bleeding increases in frequency, duration, and amount may become continuous ▪ watery, blood-tinged vaginal discharge that becomes dark and foul smelling indicates disease progression. ▪ Leg pain (along the sciatic nerve) or swelling of one leg may be a late symptom or may indicate recurrent disease. ▪ Flank pain may be a late symptom of hydronephorsis – indicating advanced cancer pressing on ureters. ◦ Early stage I management techniques include local cervical ablation therapies of electrosurgical excision, laser therapy, or cryosurgery. ◦ Small tumors that are only micro invasive are managed with excision conization or hysterectomy ◦ Early-stage invasive cancers are managed with radical surgery and radiation.◦ Advanced inoperable cancers are treated with radiation. ◦ The loop electrosurgical excision procedure (LEEP) ▪ both a diagnostic procedure and a treatment, as it provides a specimen that can be examined by a pathologist. ▪ After local cervical ablation therapies remind patients to take showers rather than baths Ovarian cancers: ◦ grow rapidly, spread quickly, and are often bilateral – Ovarian cancer seems to be disordered growth in response to excessive exposure to estrogen ◦ The leading cause of death from female reproductive cancers is ovarian cancer, with low survival rates attributed to the late detection. ◦ CA-125 and alpha-fetoprotein (AEP) are both elevated when ovarian cancer is present ◦ Risk factors for ovarian cancer: ▪ Older than 40 years old ▪ family history of cancer ▪ diabetes ▪ nulliparity ▪ older than 30 years at first pregnancy ▪ breast cancer ▪ colorectal cancer ▪ infertility ▪ BRCA1 or 2 gene mutations ▪ early menarche or late menopause ▪ endometriosis ▪ and obesity. ◦ Nurses should teach women to ―think ovarian‖ when it comes to vague abdominal and GI symptoms, such as dyspepsia and gas. ◦ Diagnosis depends on surgical exploration. Exploratory laparotomy (abdominal surgery) is performed to diagnose, treat, and stage ovarian tumors. ◦ A total hysterectomy, bilateral salpingo-oophorectomy (BSO) (removal of the ovaries and fallopian tubes), and pelvic and para-aortic lymph node dissection are usually performed Prostate Cancer: ◦ Of all malignancies, prostate cancer is one of the slowest growing, and it metastasizes (spreads) in a predictable pattern ▪ Common sites of metastasis are the nearby lymph nodes, bones, lungs, and liver ▪ The bones of the pelvis, sacrum, and lumbar spine are most often affected ◦ Prostate cancer is caused by a number of factors: ▪ Advanced age is the leading risk factor▪ Race is the second most common risk factor: disease affects African Americans more often than other ethnic/racial groups, followed by Caucasians (Euro-Americans) and HispanicAmerican men. ▪ family history of prostate cancer is the third most common risk factor for this malignancy ▪ The risk increases twofold for men who have a first-degree relative (brother, father) with the disease ▪ Other risk factors that may play a role are eating a diet high in animal fat (e.g., red meat) and complex carbohydrates or having a low-fiber intake. ▪ Men who have had a vasectomy or those who were exposed to environmental toxins, such as arsenic, may also be at increased risk for the disease. ◦ Many gene mutations play a role in various types of prostate cancer ▪ Some men with the most aggressive prostate cancers have BRCA2 mutations similar to those women who have BRCA2-associated breast and ovarian cancers ▪ The most common genetic factor that increases the risk for prostate cancer is a mutation in the glutathione S-transferase (GST P1) gene – This gene is normally part of the pathway that helps prevent cancer ◦ Although not agreed upon by all authoritative sources, starting at the age of 50 years, men should discuss the options of having prostate-specific antigen testing with their health care provider Assessment for prostate cancer: ◦ Assess the patient's age, race/ethnicity, and family history of prostate cancer ◦ Ask about his nutritional habits, especially focusing on the intake of red meat, fish, and fruits and vegetables ◦ Assess whether the patient has any problems with urinary elimination ◦ Take a drug history to determine if he is taking any medication that could affect voiding ◦ The first symptoms that the man may report are related to bladder outlet obstruction, such as difficulty in starting urination, frequent bladder infections, and urinary retention ◦ Ask about urinary frequency, hematuria (blood in the urine), and nocturia (voiding during the night) ◦ Ask if he has had any pain during intercourse, especially when ejaculating ◦ Inquire if the patient has had or currently has any other pain (particularly bone pain), a symptom associated with advanced prostate cancer ◦ Ask him if he has had any recent unexpected weight loss – a huge difference in weight loss is a huge indicator of cancer ◦ Take a sexual history for recent changes in desire or function. Ask about current or previous sexually transmitted diseases, penile discharge, or scrotal pain or swelling. ◦ Most early cancers are diagnosed while the patient is having a routine physical examination or is being treated for benign prostatic hyperplasia (BPH) ◦ Gross blood in the urine (hematuria) is a common clinical manifestation of late prostate cancer◦ Prepare the patient for a digital rectal examination (DRE) ▪ On rectal examination, a prostate that is found to be stony hard and with palpable irregularities or indurations is suspected to be malignant Laboratory Assessment: ◦ Prostate-specific antigen (PSA): glycoprotein produced by the prostate ▪ used as a screening test for prostate cancer ▪ should be drawn before the DRE because the examination can cause an increase in PSA due to prostate irritation ◦ Most sources agree that the normal blood level of PSA in men younger than 50 years is less than 2.5 ng/mL ▪ PSA levels increase to as high as 6.5 ng/mL when men reach their 70s ▪ African-American men have a slighter higher normal value ▪ Because other prostate problems also increase the PSA level, it is not specifically diagnostic for cancer – some other problems that can > PSA levels are prostatitis and BPH ◦ An elevated PSA level should decrease a few days after a prostatectomy for cancer. ◦ An increase in the PSA level several weeks after surgery may indicate that the disease has recurred. ◦ Because PSA is not absolutely specific to prostate cancer, another test, early prostate cancer antigen (EPCA-2), may be a serum marker for prostate cancer ▪ It can detect changes in the prostate gland early and is a very sensitive test EPCA-2 may also eliminate the need to perform a biopsy of prostate tissue Testicular Cancer: ◦ Rare form of cancer that most often effects men between ages of 20-35 years of age. ◦ With early detection there is a 95% cure rate ◦ Most common type is germ cell tumors arising from sperm-producing cells ▪ Seminoma tumors are usually localized, metastasize late, and respond to treatment. ◦ Least common type is non-germ cell tumors in stromal, interstitial, or Leydig cells ▪ Most do not metastasize ▪ Adroblastomas sometimes secrete estrogen, which causes feminization and gynecomastia ◦ Men with cryptocordism or HIV have higher risk of testicular tumors. ◦ Leukemia, lymphoma, and metastatic carcinomas may also invade the testes. ◦ Common tumor markers that confirm testicular cancer are alfa-fetoprotein, hCG, and LDH ◦ Lymphangiography shows the body’s lymph systems to look for spread of cancer to other areas ◦ Oligospermia (low sperm count) and azoospermia ( absence of living sperm) are common in testicular cancer. ◦ Educate patient on sperm banking options ◦ Orchiectomy is removal of affected testicle▪ Teach patients having a minimally invasive surgery that carbon dioxide may be used as part of surgery and chest or shoulder pain may be expected after surgery ▪ An open orchiectomy results in sterility ▪ A silicone implant may be put in place after orchiectomy ▪ External beam radiation may be used after orchiectomy – The remaining testis is shielded by a lead cup during radiation but sperm count may still be reduced during treatment. Sperm count usually returns to normal around 24-30 months after treatment ◦ Hydrocele- Fluid around testicle ◦ Spermatocele- cystic mass on epididymis ◦ Varicocele- dilated veins Leukemia and Lymphomas- s/s nursing care and considerations treatments diagnostics Diagnostic Procedures 1. Genetic Tests- Breast Cancer 2. Tissue Biopsy- what is involved 3. Lab Studies a. Hemoglobin – Anemia ;-decrease may indicate malignancy. b. Hematocrit – Anemia; may indicate malignancy c. Leukocytes – elevated in Leukemia and lymphomas d. Platelets – elevated with CML, Hodgkins disease; decreased with bone marrow suppresion and multiple myeloma 4. Imaging 1. MRI 2. Computed Tomography (CT scan) 3. Ultrasonography 4. Endoscopy 5. Nuclear Medicine Imaging 6. PET (Positron Emission Tomography) Scan 7. Radioimmunoconjugates 5. Tumor Marker Assays a. Tumor Ma CA – 125 – should be less than 35 units- it will be elevated in ovarian cancer and pancreatic cancers b. CEA – 0-.5mg/ml for non-smokers and less than 3ng/ml for smokers – increased in colorectal cancer, breast cancer, stomach cancer, pancreatic and prostate cancer. c. PSA – 0-4 mg/ml – increased in prostate cancerd. CA 19 – 9 – increased in pancreatic, colon, and gastric cancers e. Markers (CEA, PSA) Oncologic Emergencies ONCOLOGICAL EMERGENCIES: • Sepsis and disseminated intravascular coagulation (DIC) • Syndrome of inappropriate antidiuretic hormone (SIADH) • Spinal cord compression • Hypercalcemia • Superior vena cava (SVC) syndrome • Tumor lysis syndrome (TLS) Care of the Patient with Myelosuppression and Neutropenia: The three components of myelosuppression management are: ◦ prevention of infection, ◦ frequent patient assessment for the early detection of infection, ◦ and aggressive management when such infection arises. Neutropenia: infection and bleeding precautions Radiation: • Radiation therapy is used to interrupt cellular growth • Radiation may also be used to control malignant disease when a tumor cannot be removed surgically or when local nodal metastasis is present Types 1. External Radiation: 2. Internal Radiation: Brachytherapy – Internal radiation therapy (brachytherapy) allows a higher dose of radiation in a smaller area than might be possible with external radiation treatment. It uses a radiation source that’s usually sealed in a small holder called an implant. Intracavitary radioisotopes Internal radiation with Implants: Because internal radiation emit radiation while the implant is in place, contacts should consider time, distance and shielding Patient must be placed in private room (at the end of the hall), with appropriate signs on doors, having staff members wear dosimeter badges, making sure pregnant staff members are not assigned to patient, and prohibiting children from visiting Visitor should stand at a minimal of 6 feet from patient Radiation Toxicity: • Altered skin integrity is a common effect and can include alopecia, erythema and shedding of skin (desquamation) • Xerostomia – dryness of mouth is from radiation as well as changes in taste and decreased salivation • Esophageal irritation with chest pain • Anorexia, nausea and vomiting • Bone marrow cells proliferate rapidly, leukopenia occurs (decrease in white blood cells) • Thrombocytopenia occurs (decrease in platelets) Nursing: Protecting the Skin and Oral Mucosa – during radiation should avoid ointments, lotions or powder to area Gentle oral hygiene to promote tissue healing Protecting the Caregivers with time, distance and shielding Chemotherapy: • Chemotherapy – the MD uses antineoplastic agents in an attempt to destroy tumor cells by interfering with cellular functions and reproduction • Toxicity of CHEMO • GI System • Hematopoietic • Renal System • Cardiopulmonary • Reproductive • Neurologic Acronym for remembering undesirable effects of neoplastic drugs: • B – Bone Marrow Depression • A – Alopecia • R – Retching with nausea and vomiting • F – Fear and anxiety• S – Stomatitis Acronym for Nursing Considerations with Cancer and neoplastic drugs • C – CBC, platelets • A – Antiemetics before drugs • N - Nephrotoxicity • C – Counseling regarding reproduction issues • E – Encourage handwashing, avoid crowds • R – Recommend a wig with alopecia • U-Unexplained weight loss • P-pernicious anemia Types of Bone marrow Transplants: • Three types of transplants: • Allogeneic – from a donor other than the pt of from a matched donor • Autologous – from patient • Syngeneic – from an identical twin SLE & DLE- Patho, s/s, diagnostics, treatments and nursing care, meds Rheumatoid Arthritis: patho and treatment,s/s, nursing considerations, meds HIV/AIDS Retrovirus that uses reverse transcriptase to convert a single strand of RNA to double stranded DNA making the viral DNA the same as the host’s DNA. LOVES CD4 cells (T-cells) o Gets inside the cell and L/T damage and destruction of the cell o Decreases in CD4 cells show progression of disease CD4 counts: Normal 800-1000 cells/mL with a lifespan of about 100 days With HIV invasion, this number decreases and lifespan goes to about 2 days. Integrase is used by HIV to INTEGRATE its genetic material into the host’s (CD4 cells) chromosomes o L/T particles of HIV that are made o This long strand is clipped by an enzyme- protease which PROMOTES or causes smaller strands to be made which can create an envelope around themselves fuse with the infected CD4 cell’s membrane and bud off to infect other CD4 cells. Changes CD4 cells to HIV factories Increased virus=decreased CD4 cell (decreased immunity) HIV and AIDS are NOT the same! o Person with HIV may or may not have AIDS The CD4 cell count and the presence or absence of opportunistic infections makes the difference Requirements for AIDS classification: HIV CD4 T-cell count of <200 cells/mm3 or less than 14% Opportunistic infections 4 Stages of HIV: virus can be transmitted at any stage but Stage 4 and those who do not know they have HIV with high viral loads with no ART therapy are the MOST infectious Highest concentration of HIV is in blood and semen o Can be found in many other bodily secretions Transmission via o Parenteral (dirty needles/ IV drug use/contaminated equipment) o Sexual (HIV infected partners, any form that the mucus membranes will be disturbed, no condoms, use of spermicides) HIGHEST RISK! Anal intercourse o Perinatal (birth, placenta, blood and secretions) o Occupational exposure (needle sticks) Viral loads o Virema=high viral load=increased risk of transmission o HAART decreases viral loads BUT this DOES NOT DECREASE the risk of transmission Teach prevention, safe sex practices, the 3 C’s, standard precautions, getting checked, and following drug therapy regimens ELISA and Western Blot detect HIV antibodies Donated blood is tested using NAT Opportunistic infections o PCP: common in AIDS patients o Candida albicans: stomatitis, esophagitis, vaginal yeast infections o Cryptococcosis: meningitis o MAC: Most common bacterial infection in those with AIDS o TB: skin test (PPD) o Varicella zoster o Kaposi sarcoma o AIDS dementia complex PeP and Pre Sensory Neuro Focus Notes – Maddie’s Version Assessment pt the Eye and Vision Anatomy and Physiology: ◦ Layers of the eyeball ◦ Three Layers▪ external layer sclera – white of the eye transparent cornea on front of the eye ▪ middle layer (uvea) heavily pigmented choroid ◦ dark brown membrane between sclera and retina ◦ has many blood vessels that supply nutrients to retina ciliary body ◦ connect choroid with iris ◦ secretes aqueous humor iris ◦ colored portion of external eye ◦ center opening is known as pupil ◦ iris contract and relax to control pupil size ▪ determining how much light enters the eye ▪ innermost layer retina ◦ made up of sensory photoreceptors ◦ begin transmission of impulses to the II cranial nerve (OPTIC) ◦ contains blood vessels ▪ rods – work at low light; peripheral vision ▪ cones – work at bright light; color and central vision ◦ Refractive structures and media ◦ aqueous humor ▪ clear watery fluid that fills the anterior and posterior chambers of the eye◦ IOP ▪ intraocular pressure ▪ to maintain the shape of the eye – vitreous humor gel in the posterior segment and the aqueous humor in the anterior segment must be present in set amounts that apply pressure inside the eye to keep it inflated ▪ normal ranges 10-21 for IOP ▪ has to be accurate!!! if low – eyeball is soft and collapses preventing light from getting to photoreceptors on retina if high – extra pressure compresses capillaries in eye and nerve fibers preventing blood from flowing ◦ photoreceptors and nerve fibers become hypoxic ◦ this is how glaucoma can occur ◦ continued retinal hypoxia – necrosis and death of photoreceptors plus nerve fiber damage ▪ permanently blind is the result KNOW CRANIAL NERVES RELATED TO EYE ◦ muscles around the eye are innervated by cranial nerves ▪ III (this is 3) – oculomotor ▪ IV (this is 4) – trochlear ▪ VI (this is 6) – abducens ◦ cranial nerve II (two – optic) is the nerve of sight; connecting optic disc to brain ◦ trigeminal nerve (V – five) stimulates blink reflex when cornea is touched ◦ VII (seven – facial nerve) innervates the lacrimal glands and muscles for lid closure KEY TERMS: ◦ emmetropia ▪ perfect refraction of eye ◦ hyperopia▪ eye does not refract light enough ▪ near vision is poor ▪ farsightedness ▪ images converge behind retina ◦ myopia ▪ nearsightedness ▪ images converge in front of retina ▪ distant vision is poor ◦ astigmatism ▪ refractive error caused by unevenly curved surfaces on or in eye ▪ happens mainly in cornea ▪ distort vision ◦ miosis ▪ pupillary constriction ◦ mydriasis ▪ pupillary dilation ◦ accommodation ▪ process of maintaining a clear visual image when the gaze is shifted from a distant to a near object ◦ convergence ▪ ability to turn both eyes inward toward nose at same time ▪ helps ensure only a single image of close objects is seen ◦ presbyopia ▪ near objects must be placed farther from the eye to be seen clearly ◦ exophthalmos ▪ proptosis▪ protrusion of eye ◦ enophthalmos ▪ sunken appearance of eye ◦ ptosis ▪ drooping of eyelids age related changes ◦ appearance ▪ eye appear sunken – do not use appearance of eyes as a sign for dehydration ▪ arcus senilis forms – this change does not affect vision ▪ sclera yellows or appears blue – do not use sclera to assess for jaundice ◦ cornea ▪ flattens which blurs vision – have regular eye exams, wear corrective lenses ◦ ocular muscles ▪ strength is reduced in muscles makes it more difficult to maintain upward gaze/focus on single image ◦ lens ▪ elasticity is lost – increasing near point of vision – wear reading glasses ▪ lens hardens, compacts, and forms cataract – annual vision checks and monitoring to detect early ◦ iris and pupil ▪ decrease in ability to dilate results in small pupil size and poor adaptation to darkness good lighting is important to avoid tripping ◦ color vision ▪ green, blue, violet discrimination decreases ▪ color-indicator with pills is not a good way to determine which pills to take** ◦ tears▪ production reduced – dry eyes is common which increases risk for corneal damage and eye infections saline drops importance increase humidity at home Using Eyedrops – main points ◦ if both eyes to receive drops and only ONE is infected ▪ two separate bottles labeled right and left for each eye ◦ wash hands and apply gloves ◦ pt. tilt head back and open eyes ▪ look up at ceiling ◦ pull lower lid down against cheek forming small pocket ◦ do not touch eye with tip of bottle and insert instilled amount of drops into pocket of lower lid ◦ gently close eye without squeezing lids ◦ if systemic drug ▪ hold the corner of eye nearest to nose (lacrimal fossa) to prevent drug from being absorbed ◦ blot away excess drug or tears with tissue ◦ keep eye closed for about 1 minute ◦ wash hands again Systemic conditions affecting eye and vision ◦ diabetes mellitus – retinal damage ◦ HTN ◦ lupus erythematosus ◦ sarcoidosis ◦ thyroid problems (bulging in hyperthyroid!! – remember exo..) ◦ acquired immune deficiency syndrome ◦ cardiac disease◦ multiple sclerosis ◦ pregnancy Drugs that affect eye and vision ◦ antihistamines, corticosteroids, and decongestants* ▪ *prescription and OTC ◦ antibiotics ◦ opioids ◦ anticholinergics ◦ cholinergic agonist ◦ adrenergic agonist ◦ beta blockers (adrenergic antagonists) ◦ oral contraceptives ◦ chemotherapy drugs Nutrition for eye health ◦ diet rich in fruit and red, orange, and dark green veggies is good for eye health ▪ kale ▪ bananas ▪ carrots ▪ spinach Consensual response ◦ PERRLA ◦ assess the response of each eye ◦ pupils equal, round, reactive to light and accommodation Some diagnostic assessments: ◦ Slit-lamp examination: ▪ magnifies the anterior eye structures▪ examiner can locate the position of any abnormality in the cornea, lens, or anterior vitreous humor ◦ Corneal staining: ▪ consist of placing fluorescein or other topical dye into conjunctival sac ▪ dye outlines irregularities of the corneal surface not easily visible ▪ test used for corneal trauma, problems caused by contacts, or presence of foreign bodies, abrasions, ulcers, or other corneal disorders ▪ noninvasive and aseptic conditions used ▪ eye is viewed by blue filter and non intact areas of the cornea stain a bright green color ◦ Tonometry: ▪ measures IOP using a tonometer ▪ applies pressure to the outside of eye until it equals pressure inside the eye ▪ normal range is between 10-21 *number not absolute, must be considered along with corneal thickness thickness of cornea affects how much pressure must be applied before indentation occurs thicker cornea – higher tonometer reading – falsely indicate increased IOP thinner than normal cornea – low reading – even when higher IOP is present ◦ Opthalmoscopy: ▪ views eyes using opthalmoscope ▪ this is where you see the red reflex A RED GLARE is seen in the pupil ◦ red glare is seen as a reflection of the light off of the retina when directing the opthalmoscope at the pupil if absent: ◦ may indicate a lens opacity or cloudiness of the vitreous ▪ avoid this test when patient is confused to prevent accidental injury to eye (or so you do not get hit) ◦ Gonioscopy:▪ test performed when high IOP is found ▪ determines whether patient has open-angle or closed-angle glaucoma Care of Patients With Eye and Vision Problems Blepharitis – ◦ inflammation of the eyelids ▪ causes itching, erythema, greasy scales on brows and eyelids Entropion – ◦ the inward turning of the eyelid ◦ lashes rub against eye and cause irritation ◦ surgical correction is needed Ectropion – ◦ the outward turning of the eyelid ◦ surgical correction is needed Hordeolum/Stye – ◦ can be internal or external ◦ results from bacterial infection of sebaceous gland around the eyelid margin ◦ characterized by tender bump on edge of eyelid Chalazion – ◦ pus-filled cyst on the eyelid caused by a blocked sebaceous gland; red, painless Keratoconjunctivitis Sicca – ◦ ―Dry Eye‖ ◦ caused by lacrimal gland dysfunction or poor tear distribution ◦ treated with artificial tears, ointment, or surgery Trachoma – ◦ chronic and bilateral conjunctivitis caused by Chlamydia trachomatis ◦ chief cause of preventable blindness treated with PO azithromycin or ophthalmic tetracycline Keratoconus – ◦ degeneration of corneal tissue, leading to abnormal corneal shape ◦ can occur due to trauma, an untreated corneal infection, or an inherited disorder ◦ Treatment: ▪ keratoplasty (corneal transplant) – from human donor Preoperative assessment is usually short because transplant is done when donor is available ◦ assess eye for drainage, edema, erythema ◦ prophylactic antibiotic eyedrops are instilled ◦ obtain IV access postoperatively ◦ after the procedure, instruct patient to lie on unaffected side to reduce IOP ◦ wear shield at night or at home around children and pets to avoid injury ◦ avoid activities that increase IOP ◦ complications: REPORT to HCP ▪ bleeding ▪ wound leakage ▪ infection ▪ graft rejection ▪ decreased vision ▪ increased reddening of eye ▪ pain and increased sensitivity to light ▪ presence of light flashes or floaters in field of vision Cataract ◦ clouding of the lens of the eye with restricted visual acuity; may have slow or rapid onset; severe cataract treated with surgery ◦ lens opacity that distorts the image▪ with aging; lens gradually loses water and increases in density ◦ Cataract Surgery – replace clouded lens with plastic lens or donor lens known as IOL (replacement intraocular lens) ◦ lens often extracted by phacoemulsification ▪ probe is inserted through the capsule and high-frequency sound waves break the lens into small pieces ▪ small pieces removed by suction ▪ in short: sound waves break up the lens, pieces are sucked ut, and the capsule remains largely intact ◦ Post-op Care after cataract surgery: immediately after surgery: antibiotics and steroid ointments are given priorities are to reduce IOP, prevent infection, and assess for bleeding subconjunctival antibiotics eye unpatched and discharge within about 1 hour dark glasses required mild itching is normal as well as ―bloodshot appearance‖, but pain indicates complications like increased IOP or hemorrhage ◦ contact HCP if pain occurs with N/V teach patient to avoid activities that increase IOP: ◦ bending from waste ◦ lifting objects more than 10lbs ◦ sneezing and coughing ◦ blowing the nose ◦ straining from BM ◦ vomiting ◦ sexual intercourse ◦ head in a dependent position ◦ wearing tight shirt collars teach patient to report: ◦ sudden, sharp eye pain, ◦ eyelid swelling, ◦ bleeding or increased discharge, ◦ decreased vision, ◦ flashes of light or floating shapes, ◦ reappearance of bloodshot sclera after initial appearance has cleared cold compresses may be beneficial avoid aspirin anti-platelet – use acetaminophens like tylenol ◦ cataract -- clouding of lens - may be unilateral or bilateral; one of the most common eye disorders ▪ first type: senile cataract - result of aging process ▪ second type: traumatic develops within a few months after eye trauma painless but progressive loss of sight in one or both eyes ◦ BOTH EYES MAY HAVE CATARACTS BUT THE RATE OF PROGRESSION IN EACH EYE IS DIFFERENT ◦ final best vision will not occur until 4-6 weeks after surgery Glaucoma ◦ group of eye conditions that lead to damage to the optic nerve (II) due to increased intraocular pressure (IOP) ▪ increased IOP caused by decreased expulsion of aqueous humor ◦ Types - 4 major types ▪ open-angle (chronic) glaucoma ▪ angle-closure (acute) glaucoma ▪ congenital glaucoma ▪ secondary glaucoma ◦ Open-Angle Glaucoma:▪ most common type ▪ chronic, with a slightly opened canal of Schlemm and overflow drainage of aqueous humor ▪ aqueous humor does not drain adequately, causing intraocular pressure (IOP) to increase this pressure on optic nerve causes destruction of nerve fibers in retina, with results of vision loss ▪ most clients are symptom-free until loss of vision ▪ peripheral vision is affected first ▪ three classic findings: elevated intraocular pressure visual field loss cupping of optic disk ▪ treatment: pharmacotherapy pilocarpine carbonic anhydrase inhibitors beta-adrenergic blocking agents epinephrine eye drops (contraindicated in clients with cardiac conditions) ◦ Closed-Angle Glaucoma: ▪ acute, considered a medical emergency ▪ canal of Schlemm is completely blocked ▪ no aqueous humor draining out of the eye, resulting in increased IOP ▪ (shallow, narrow-angle, primary, or congested glaucoma) - iris bulges and blocks trabecular network ▪ iris lies near drainage channel (canal of Schlemm) and bulges forward against cornea, blocking the trabecular network and increasing IOP ▪ affects more women; usually after age 45 ▪ sudden onset of blurred vision, halos or colored rings around white lights, frontal headache, severe eye pain ▪ profuse lacrimation; mildly dilated, nonreactive pupil, and nausea/vomiting, cornea appears hazy▪ findings may come and go, and resolve with rest or sleep ▪ emergency pharmacologic treatment: includes carbonic anhydrase inhibitors - Diamox miotic eye drops - constricts pupil intravenous osmotic agents systemic analgesics ◦ S/S of Glaucoma: ▪ headache, ▪ brow pain, ▪ nausea/vomiting, ▪ halos, ▪ blurred vision, ▪ decreased light perception ◦ Testing for Glaucoma: ▪ tonometry, perimetry, genioscopy, optic nerve imaging Treatment for glaucoma: atenolol 4% ophthalmic (can produce systemic effects – beta blocker) ◦ Surgery: ▪ laser trabeculoplasty (burns trabecular meshwork, scaring it and causing meswork fibers to tighten – increasing the size of spaces between fibers, improving outflow of aqueous humor and decreasing IOP ▪ trabeculectomy (creates new channel for fluid outflow) ▪ iridotomy or iridectomy (on her notes?) procedure is usually then repeated on unaffected eye Corneal Disorders: ◦ corneal abrasion – scrape or scratch injury of the cornea ▪ can be caused by small foreign body, trauma, or contacts ◦ corneal ulceration▪ deeper injury ▪ bacterial, protozoal, and fungal infections can lead to this ▪ EMERGENCY because cornea has no separate blood supply and infections that can permanently impair vision develop rapidly ◦ keratoconus – look at top of section covered Retinal Disorders ◦ Macular degeneration ▪ deterioration of the macula – area of central vision ▪ age related or exudative ▪ age related has two types: dry AMD (most common): ◦ caused by general blockage of retinal capillaries – allowing retinal cells in the macula to become ischemic and necrotic ◦ mild blurring and distortion at first – eventually all central vision is lost ◦ more common in smokers than non smokers ◦ HTN, female gender, and short stature other risk factors ◦ dry AMD can also develop exudative macular degeneration ◦ has NO CURE ◦ risk for dry AMD can be reduced by ▪ antioxidants ▪ vitamin B12 ▪ carotenoids lutein and zeaxanthin wet AMD: ◦ another cause of AMD ◦ growth of new blood vessels in the macula, which have thin walls and leak blood and fluid exudative macular degeneration is also a type of wet macular degeneration BUT CAN OCCUR AT ANY AGE ◦ can occur in only one eye or in both eyes ◦ sudden decrease in vision after a detachment of pigment epithelium in the macula ◦ newly formed blood vessels invade this injured area and cause fluid and blood to collect under macula ◦ Retinal holes, tears, and detachements ▪ retinal hole is break in retina ▪ retinal tear is a jagged and irregular shaped break in retina ▪ retinal detachment is separation of the retina from epithelium onset is sudden and painless may suddenly see bright flashes of light (photophobia) floating dark spots in affected eye partial detachment – sensation of curtain being pulled over part of visual field Reactive errors ◦ Myopia ▪ nearsightedness; eye over-refracts light and bent images fall in front of retina ◦ Hyperopia ▪ farsightedness; weak refraction, images are focused behind the retina ◦ Presbyopia ▪ age-related; lens loses its elasticity and is less able to change shape to focus on close work, and image falls behind the retina ◦ Astigmatism ▪ occurs due to an uneven curve of the cornea Trauma ◦ Foreign body ▪ eyelashes, dirt, dust, and airbone particles come into contact w/conjunctivia or cornea and irritate or abrade the surface▪ use eversion procedure to examine conjunctiva IF nothing seen on the cornea or conjunctivia ◦ Corneal abrasion ▪ disruption of the cells and loss of superficial epithelium ▪ caused by trauma, chemical irritant, foreign body, or lack of moisture ▪ severe pain, blurred vision, halo around lights, lacrimation, inability to open eye ▪ diagnosis by fluorescein sodium dye ▪ abrasions heal within 48 to 72 hours, usually with no scarring or visual deficit ▪ treatment includes short-acting analgesic drops, eye rest, anti-biotics or anti-inflammatories as indicated from cause ◦ Corneal laceration ▪ findings as abrasions, but lacerations are serious emergencies ▪ surgery is generally required enucleation is removal of the eye if eye contacts have prolapsed through laceration or if injury is severe Chemical irritants ◦ flush eye with plenty of water or sterile saline - flush for a minimum of 5 minutes ◦ get client to emergency room immediately ◦ acids coagulate the eye's proteins and often result in relatively superficial, reversible damage EYE DISORDERS CHART Disorder Eye trauma Location Cornea Etiology Abrasion Treatment Cover eye to protect and allow healing; eye drops (antibiotic, anti-inflammatory) Eye trauma Cornea Laceration Surgery; eye drops (antibiotic, anti-inflammatory) Glaucoma Aqueous humor increased Intraocular pressure increased Trabeculectomy, iridotomy, or iridectomy; eye drops (often miotics) Cataract Lens Cloudy Phacoemulsion** Disorders of refraction Lens Loses elasticity, or ciliary muscles weaken Corrective lens or various types of outpatient laser surgery Retinal detachment Retina Retina tears loose from back of eye; severs connection with optic nerve Laser surgery, cryotherapy, diathermy, scleral buckle or pharmacotherapy Retinal degeneration Retina Rod and cone cells deteriorate None Amblyoia Entire eye Strabismus, cataracts, disorders of refraction in children Glasses (for refractive error); patch on normal eye; eye drops Assessment and Care of Patients with Ear and Hearing Problems: External ear◦ develops in the embryo at the same time as the kidneys and urinary tract ◦ if there is a defect of the external ear, examine for possible problems of the kidneys and urinary system Middle Ear ◦ consists of the epitympanum ▪ which consists of the top opening of the eustachian tube and 3 bony ossicles (malleus, incus and the stapes) ◦ The bony ossicles move with vibrations causing sound waves to hit the eardrum ◦ The eustachian tube begins at the floor of the middle ear and extends to the throat ▪ allows the pressure on both sides of the eardrum to equalize ▪ secretions from the middle ear drain through the tube into the throat. ◦ Eardrum – ▪ shiny, transparent or opaque or pearly gray ▪ moves when air is injected into the external canal ▪ redness is seen on eardrum if otitis media is present Inner Ear ◦ contains the semicircular canals, cochlea, vestibule and distal end of the 8th cranial nerve (auditory) ◦ semicircular canals: connect to the sensory nerve fibers of the vestibular portion of the 8th cranial nerve. ▪ The fluid and hair cells of the canals help maintain the sense of balance. ◦ Cochlea: ▪ spiral organ of hearing ▪ fluids protect the cochlea and the semicircular canals by allowing the structures to float and be cushioned ▪ Organ of Corti is the receptor of hearing located on the membrane of the cochlea. ▪ Cochlea hair cells detect vibration from sound and stimulate the 8th cranial nerve.◦ Vestibule is a small, oval-shaped, bony-shaped chamber between the semicircular canals and the cochlea. ▪ It contains the utricle and the saccule, organs that are important for balance Assessment Methods: ◦ Hearing assessment begins while looking, listening and answering questions with the patient. ◦ Do not assume older adult has hearing problems. ◦ Ask about occupation and hobbies. ◦ Drug history for ototoxic medications such as ▪ antibiotics, diuretics, NSAIDs and many chemotherapy agents. ◦ Ask about: ▪ ear trauma or surgery, ▪ past ear infects ▪ Hx of health problems that can decrease the blood supply to the ear such as heart disease, HTN or diabetes. ▪ Hx of vitiligo (a pigment disorder that may include a loss of melanin-containing cells in the inner ear, resulting in hearing loss) ▪ Hx of smoking, ▪ Hx of Vit B12 and folate deficiency. ◦ Personal history includes past or current manifestations of ▪ ear pain, ear discharge, vertigo (spinning sensation), tinnitus (ringing), decreased hearing, and difficulty understanding people when they talk. C h a r t 4 8 - 2 P a t i e n t a n d F a m i l y E d u c a t i o n : P r e p a r i n g f o r S e l f - M a n a g e me n t Self–Ear Irrigation for Cerumen Removal • Do not attempt to remove earwax or irrigate the ears if you have ear tubes or if you have blood, pus, or other drainage from the ear. • Use an ear syringe designed for the purpose of wax removal (available at most drugstores). • The safest type of ear syringe to use is one that has a right-angle or ―elbow‖ in the tip. • Irrigating your ears in the shower is an easy method.• Always use tap water that feels just barely warm to you. Water that is warmer or colder can make you feel dizzy and nauseated. • If your earwax is thick and sticky, you may need to place a few warm commercial eardrops that soften earwax (or baby oil or mineral oil) into the ear an hour or so before you irrigate the ear. • Fill the syringe with the lukewarm tap water. • If you are using a syringe with an elbow tip, place only the last part of the tip into your ear and aim it toward the roof of your ear canal. • If you are using a straight-tipped syringe, insert the tip only about to inch into your ear canal, aiming toward the roof of the canal. • Hold your head at a 30-degree angle to the side you are irrigating. • Use one hand to hold the syringe and the other to push the plunger or squeeze the bulb. • Apply gentle but firm continuous pressure, allowing the water to flow against the top of the canal. • Do not use blasts or bursts of sudden pressure. • The ear canal should fill, and water will begin to flow out, bringing earwax and debris with it. • If a dental water-pressure irrigator is used, put it on the lowest possible setting. • This process should not be painful! If pain occurs, decrease the pressure. If pain persists, stop the irrigation. • Continue the irrigation until at least a cup of solution has washed into and out from your ear canal. (You may have to refill the syringe.) • Tilting your head at a 90-degree angle to the side should allow most, if not all, of the water to drain out of your ear. • Repeat the procedure on the other ear. • If you feel that water is still in the canal, hold a hair dryer on a low setting near the ear. • Irrigate your ears weekly to monthly, depending on how fast your earwax collects. C h a r t 4 8 - 1 N u r s i n g F o c u s o n t h e O l d e r A d u l t Age-Related Changes in the Ear and Hearing EAR OR HEARING CHANGE NURSING ADAPTATIONS AND ACTIONS Pinna becomes elongated because of loss of subcutaneous tissues and decreased elasticity. Reassure the patient that this is normal. When positioning a patient on the side, do not ―fold‖ the ear under the head.EAR OR HEARING CHANGE NURSING ADAPTATIONS AND ACTIONS Hair in the canal becomes coarser and longer, especially in men. Reassure the patient that this is normal. More frequent ear irrigation may be needed to prevent cerumen clumping. Cerumen is drier and impacts more easily, reducing hearing function. Teach the patient to irrigate the ear canal weekly or whenever he or she notices a change in hearing. Tympanic membrane loses elasticity and may appear dull and retracted. Do not use this finding as the only indication of otitis media. Hearing acuity decreases (in some people). Assess hearing with the voice test or the watch test. If a deficit is present, refer the patient to a specialist to determine hearing loss and appropriate intervention. Do not assume all older adults have a hearing loss!! The ability to hear high-frequency sounds is lost first. Older adults may have particular problems hearing the f, s, sh, and pa sounds. Provide a quiet environment when speaking (close the door to the hallway), and face the patient. If the patient wears glasses, be sure he or she is using them to enhance speech understanding. Speak slowly and in a deeper voice, and emphasize beginning word sounds. Some patients with a hearing loss that is not corrected may benefit from wearing a stethoscope while listening to you speak. Family History and Genetic Risk ◦ Family history, as well as personal history, is important in determining genetic risk for hearing loss. ◦ Most hearing loss is a result of genetic mutation is seen in childhood. ▪ Progressive hearing loss in adults: Down Syndrome, osteogenesis imperfecta have bilateral and progressive hearing loss by their 30s. ▪ Mutations in genes: GJB2, causes poor production of the protein connexin-26, which has a role in the function of cochlear hair cells. Cytochrome p450 slow the metabolism and excretion of drugs, including ototoxic drugs. ◦ This allows ototoxic drugs to remain in the body longer, thus increasing the risk for hearing loss. Current Health Problems ◦ Assess current ear-related problems by asking about any ear ―trouble,‖ ear pain, or discharge, including earwax. ◦ Ask about a change in hearing ▪ such as hyperacusis (the intolerance for sound levels that do not bother other people) ▪ tinnitus (ringing in the ears). Otoscope: ◦ hold upside down like a large pen. ◦ Pull the pinna up and back to straighten the canal. ◦ Observe the ear canal through the otoscope as you insert the speculum into the external canal to avoid the risk for perforating the eardrum. ◦ *Do not use otoscope to examine the ears of any patient who is unable to hold his or her head still during the examination or who is confused. ◦ Reflection of otoscope`s light from the normal eardrum is the light reflex, and it appears as a clearly outlined triangle of light. ▪ Appears on left lower quadrant on left side. ▪ Appears on right lower quadrant on right side. ◦ Cerumen is generally moist and tan or brown in Caucasians and African Americans. ▪ It is dry and light brown to gray in Asians and American Indians. General Hearing Assessment: ◦ voice test: whisper a statement in one ear and ask the patient to repeat it ◦ Air conduction of sound is normally more sensitive than bone conduction. ◦ If auditory sensory perception is decreased the hearing loss is characterized as:▪ Conductive hearing loss: resulting from obstruction of sound wave transmission. Ex: foreign body in external canal, retracted or bulging tympanic membrane, or fused bony ossicles. ▪ Sensorineural hearing loss: resulting from a defect in the cochlea, the 8th cranial nerve, or the brain. Exposure to loud noise or music causes this type of hearing loss by damaging the cochlear hair. ▪ Mixed conductive-sensorineural hearing loss: resulting from both conductive and sensorineural hearing loss. ◦ Audioscopy: testing involves the use of a handheld device to generate tones of varying intensities to test hearing ◦ Tuning fork test for hearing are Weber and Rinne Test: ▪ Weber tuning fork: performed by placing a vibrating tuning fork on the middle of the patient`s head and asking patient to indicate in which ear the sound is louder. Normal hearing result is sound heard equally in both ears. ▪ Rinne tuning fork: compares hearing by air conduction with hearing by bone conduction. Sound is normally heard 2-3 times longer by air conduction than by bone conduction. Preform by placing vibrating tuning fork stem on the mastoid process (bone conduction) and asking the patient to indicate when the sound is no longer heard; ◦ bring the fork quickly in front of the pinna (air conduction) without touching the patient. Patient should indicate when sound is no longer heard ◦ normally 2-3X longer in front of the pinna after not hearing it with the tuning fork touching the mastoid process. Diagnostic Assessments – *was in her notes but she did not heavy focus on this ◦ CT is helpful in diagnosing acoustic tumors. ◦ MRI most accurately reflects soft-tissue changes.▪ Patients with older internal metal vascular clips cannot have MRI (newer clips are made of titanium and not contradicted). ◦ Frequency is the highness or lowness of tones (expressed in hetz). The greater the number of vibrations per second, higher the frequency (pitch) of the sound. The fewer the number of vibrations per second, the lower the frequency (pitch). ◦ Intensity of sound is expressed in decibels (dB). ◦ Threshold the lowest level of intensity at which pure tones and speech are heard by a patient about 50% of the time. The lowest intensity at which a young, healthy ear can detect sound about 50% of the time is 0 dB. A person with a hearing loss of 90 dB may not be able to hear speech even with a hearing aid. ◦ **Audiometry is the most reliable method of measuring the acuity of auditory sensory perception. ▪ 2 Types of audiometry Pure Tone Audiometry: ◦ air conduction pure tone testing ▪ determines hearing sensitivity (through ear phones); tones of varying frequencies and intensities are delivered through the earphones, testing one ear at a time. ▪ The patient presses a button or raises a hand to indicate when he/she hears a tone. ◦ bone conduction pure tone testing ▪ is only used when air-conduction test results are abnormal. ▪ Test determines whether the hearing loss detected by air-conduction testing is due to conductive or sensorineural factors or to a combination of the two. ▪ Bone-conducting vibrator, placed firmly behind ear on the mastoid process, is used instead of earphones. ◦ Interpretation of audiometric evaluation determines whether hearing is within normal limits or shows hearing impairment and if present, whether the hearing loss is conductive, sensorineural or mixed. Clinician examines audiogram. Speech Audiometry: ◦ the patient`s ability to hear spoken words is measured. ◦ The speech reception threshold and speech discrimination are assessed. ◦ Speech reception threshold ▪ is the minimum loudness at which a patient can repeat simple words.▪ The test determines how intense (or loud) a simple speech stimulus must be before the patient can hear it well enough to repeat it correctly at least 50% of the time. ▪ Spondee is used, words in which there is equal stress on each syllable ex: airplane, railroad, cowboy ◦ Speech discrimination testing ▪ assess the patient`s understanding of speech. ▪ An auditory sensory perception loss decreases sensitivity to sound and impairs understanding of what is being said. ▪ Standard format contains lists of one syllable words through ear phones at a selected loudness level, generally about 30-40 dB about the speech reception threshold or at patient`s most comfortable listening level. ▪ The score indicates the percentage of words repeated correctly. ◦ Tympanometry ▪ assess mobility of the eardrum and structures of the middle ear by changing air pressure in the external ear canal. ▪ *This test is helpful in distinguishing middle ear problems. Ex: otosclerosis, ossicular disarticulation, otitis media and perforation of the eardrum. ▪ It can also assess patency of the eustachian tube and for checking recovery of middle ear function after surgery. ◦ Auditory Brainsteam-Evoked Repsonse (ABR) ▪ assess hearing in patients who are unable to indicate their recognition of sound stimuli during standard hearing tests. ▪ It helps diagnose conductive and sensorineural hearing losses. ▪ Electrodes placed on scalp during test with gel. Assessment of Balance * covered these ◦ Electronystagmography (ENG) ▪ a test to assess for central and peripheral disease of the vestibular system in the ear by detecting and recording nystagmus (involuntary eye movements). ▪ Eyes and ears depend on each other for balance.▪ Electrodes are taped to the skin near the eyes, and one or more procedures (caloric testing, changing gaze position or changing head position) are preformed to stimulate nystagmus. ▪ Failure of nystagmus to occur with cerebral stimulation suggests an abnormality in the vestibulocochlear apparatus, the cerebral cortex, the auditory nerve or the brainstem. ▪ PREPARATION FOR ENG: Tell patient to fast for several hours before the test and to avoid caffeine for 24-48 hours before the test Tell patients with pacemakers that they should not have the test because pacemaker signal interferes with the sensitivity of ENG Carefully introduce oral fluids after the test to prevent nausea and vomiting ◦ Caloric testing ▪ evaluates the vestibular (inner ear) portion of the auditory nerve. ▪ Water or air that is warmer or cooler than body temperature is infused into the ear. ▪ A normal response is the onset of vertigo and nystagmus within 20-30 seconds. ▪ Patient must fast for several hours before the test will also be on best rest after the procedure with careful introduction of oral fluids to prevent nausea and vomiting Conditions Affecting the External Ear: ◦ Cerumen (earwax) or foreign body is the most common cause of impacted canal. ▪ May have sensation of fullness in the ear, with or without hearing loss ▪ may have ear pain, itching, dizziness, or bleeding from the ear. ▪ Do not irrigate ear when the foreign object is vegetable matter, because this material expands when wet. Must be physically removed by an experienced HCP. ▪ Insects are killed (mineral oil or diluted alcohol to suffocate) before removal unless coaxed out by flashlight. ▪ If local irritation, an antibiotic or steroid ointment may be applied to prevent infection. ▪ Surgical removal of foreign body may be needed by using a wire bent at 90-degree angle looped around the object and pulled out. Procedure is painful and general anesthesia is needed. Self-Ear Irrigation for Cerumen Removal ◦ do not remove earwax or irrigate the ears if you have ear tubes or if you have blood, puss or other drainage from the ear. ◦ Use tap water that is barely warm. Warmer or colder water can make you feel dizzy or nauseated. ◦ If earwax is thick and sticky, instill a few drops of baby oil or mineral oil to soften an hour or so before irrigation ◦ If using a straight-tipped syringe, insert the tip only about ½ to ¾ inch into your ear canal, aiming toward the roof of the canal. -Otosclerosis is more common in women. -Vertigo: spinning sensation Mastoiditis ◦ Infection of mastoid air cells caused by progressive otitis media. ◦ If not managed appropriately it can lead to brain abscess, meningitis, and death. ◦ S/S: ▪ Swelling behind ear ▪ pain when moving the ear or the head ▪ Pain not relieved by myringotomy. ▪ Cellulitis develops on skin or external scalp over mastoid process. ▪ Ear drum red, dull, thick, and immobile. ▪ Hearing loss occurs ▪ CT scan shows fluid in air cells of mastoid process. ◦ Most common TX: ▪ Antibiotics ▪ most common surgery is Tympanoplasty ▪ All infected tissue must be removed so does not spreadNeoplasms Middle ear tumors are rare, and the most common type is the glomus jugulare, a benign vascular lesion. Malignant ear tumors also can occur. Condition affecting the inner ear Tinnitus: ◦ Continuous ringing or noise perception in the ear. ◦ Common in one or both ears. ◦ Factors that contribute to tinnitus include ▪ age ▪ sclerosis of the ossicles ▪ Ménière's disease ▪ certain drugs (aspirin, NSAIDs, high-ceiling diuretics, quinine, aminoglycoside antibiotics) ▪ exposure to loud noise ▪ other inner ear problems ◦ The problem and its management vary with the underlying cause. ▪ When no cause can be found or the disorder is untreatable, therapy focuses on ways to mask the tinnitus with background sound, noisemakers, and music during sleeping hours. ▪ Ear mold hearing aids can amplify sounds to drown out the tinnitus during the day. ▪ A drug that is helpful to some patients pramipexole (Mirapex), an antiparkinson drug.’ ▪ The American Tinnitus Association assists patients in coping with tinnitus VERTIGO ◦ Vertigo and dizziness are common manifestations of many ear disorders. ◦ Dizziness is a disturbed sense of a person's relationship to space. ◦ Vertigo is often used interchangeably with dizziness, but the definition and cause are somewhat different. ▪ True vertigo is a sense of whirling or turning in space. Drugs that reduce vertigo effects - Dimenhydrinate (Dramamine,Gravol) - Diazepam (valium,) - Meclizine (Bonamine) - Scopolamine (Transderm Scop, Transderm-V) Meniere’s disease: ◦ More common in MEN. ◦ Excess of endolymphatic fluid that distorts the entire inner canal system. ◦ Has 3 features –▪ Tinnitus, ▪ One-sided sensorineural auditory perception loss, ▪ Vertigo occurring in attacks that can last for several days ◦ Ménière's disease usually first occurs in people between the ages of 20 and 50 years. ◦ Hearing loss reversible at first, but repeated damage to cochlea from increased fluid pressure leads to permanent hearing loss ◦ *avoid foods and fluid with high sodium continent – CAN REDUCE AMOUNT OF ENDOLYMPHATIC FLUID ◦ feels fullness of the infected ear. ◦ avoid caffeine - limit alcohol to one serving/day - avoid monosodium glutamate (MSG). ◦ Mild diuretics are prescribed to decrease endolymph volume and antivertigimous drugs such as Meclizine (antivert). ◦ Pulse pressure treatments – meniett device ◦ Labyrinthectomy- total removal of labyrinth. ▪ Results in total auditory sensory perception loss on operative side. ▪ some pt report relief of vertigo with retention of hearing. Etiology and Genetic Risk For Hearing Loss ◦ Conductive hearing loss ▪ can be caused by any inflammation or obstruction of the external or middle ear. ▪ Changes in th eardrum such as bulging, retraction, and perforations may damage middle ear structures and lead to conductive hearing loss. ▪ Tumors, scar tissue, and overgrowth of soft bony tissue (otosclerosis) on the ossicles from previous middle ear surgery also lead to conductive hearing loss. ◦ Sensorineural hearing loss ▪ occurs when the inner ear or auditory nerve (cranial nerve VIII) is damaged. ▪ Prolonged exposure to loud noise damages the hair cells of the cochlea. ▪ Many drugs are toxic to the inner ear structures, and their effects on hearing can be transient or permanent, dose related, and affect one or both ears. When ototoxic drugs are given to patients with reduced kidney function, increased ototoxicity can occur because drug elimination is slower, especially among older patients. ◦ Presbycusis: ▪ Sensorineural auditory sensory perception loss that occurs with aging▪ Vit B12 and folic acid deficiency increase risk for presbycusis. ▪ Other causes: diabetes, atherosclerosis, HTN, infections, fever, Stapedectomy: ◦ can correct some hearing loss, especially in hearing loss related to otosclerosis. ◦ The patient must be free of external otitis at surgery to prevent infection. ◦ Hearing is initially worse after surgery and improvement may not occur until 6 weeks after surgery. ◦ Cranial nerves VII, VIII, X can be damaged. ▪ Assess for facial nerve damage or weakness (drooping of affected side). ▪ Ask about changes of facial perception of touch and taste. ◦ Vertigo, N/V usually occur after surgery. ▪ *Prevent injury by assisting the patient with ambulation during the first 1-2 days after stapedectomy. ▪ Keep top bedside rails up, and remind the patient to move the head slowly to avoid vertigo. Comparison of Features for Conductive and Sensorineural Hearing Loss Chart CONDUCTIVE HEARING LOSS SENSORINEURAL HEARING LOSS Causes Cerumen Foreign body Perforation of the tympanic membrane Edema Infection of the external ear or middle ear Tumor Otosclerosis Prolonged exposure to noise Presbycusis Ototoxic substance Ménière's disease Acoustic neuroma Diabetes mellitus Labyrinthitis Infection MyxedemaCONDUCTIVE HEARING LOSS SENSORINEURAL HEARING LOSS Assessment Findings Evidence of obstruction with otoscope Abnormality in tympanic membrane Speaking softly Hearing best in a noisy environment Rinne test: air conduction greater than bone conduction Weber test: lateralization to affected ear Normal appearance of external canal and tympanic membrane Tinnitus common Occasional dizziness Speaking loudly Hearing poorly in loud environment Rinne test: air conduction less than bone conduction Weber test: lateralization to unaffected ear Nonsurgical Management. ◦ Early detection helps correct the problem causing the hearing loss. ◦ Drug therapy Is focused on correcting the underlying problem or reducing the side effects of problems occurring with hearing loss. ▪ Antibiotic therapy is used to manage external otitis and other ear infections. ▪ Teach the patient the importance of taking the drug or drugs exactly as prescribed and completing the entire course. ▪ Antiemetic, antihistamine, antivertiginous, and benzodiazepine drugs can help reduce these problems. ◦ Assistive devices are useful for patients with permanent hearing loss. ▪ Cochlear implantation may help patients with sensorineural hearing loss. Although a superficial surgical procedure is needed to implant the device, the procedure does not enter the inner ear and thus is not considered a surgical correction for hearing impairment. A small computer converts sound waves into electronic impulses. Electrodes are placed near the internal ear, with the computer attached to the external ear. The electronic impulses then directly stimulate nerve fibers. Some patients have a 50% return of their hearing with this method Hearing Aid Care ◦ Keep the hearing aid dry. ◦ Clean the ear mold with mild soap and water while avoiding excessive wetting. ◦ Using a toothpick, clean debris from the hole in the middle of the part that goes into your ear. ◦ Turn off the hearing aid when not in use.◦ Check and replace the battery frequently. ◦ Keep extra batteries on hand. ◦ Keep the hearing aid in a safe place. ◦ Avoid dropping the hearing aid or exposing it to temperature extremes. ◦ Adjust the volume to the lowest setting that allows you to hear, to prevent feedback squeaking. ◦ Avoid using hair spray, cosmetics, oils, or other hair and face products that might come into contact with the receiver. ◦ If the hearing aid does not work: ▪ Change the battery. ▪ Check the connection between the ear mold and the receiver. ▪ Check the on/off switch. ▪ Clean the sound hole. ▪ Adjust the volume. ▪ Take the hearing aid to an authorized service center for repair. Tympanoplasty. ◦ Tympanoplasty reconstructs the middle ear to improve conductive hearing loss. ◦ The procedures vary from simple reconstruction of the eardrum (myringoplasty) ◦ to replacement of the ossicles within the middle ear (ossiculoplasty). ◦ Postoperative Care. ▪ An antiseptic-soaked gauze, such as iodoform gauze (NU GAUZE), is packed in the ear canal. ▪ If a skin incision is used, a dressing is placed over it. ▪ Keep the dressing clean and dry, using sterile technique for changes. ▪ Keep the patient flat, with the head turned to the side and the operative ear facing up (LAY ON YOUR UNAFFECTED EAR) for at least 12 hours after surgery Stapedectomy. ◦ A partial or complete stapedectomy with a prosthesis can correct some hearing loss, especially in patients with hearing loss related to otosclerosis. ◦ Although hearing usually improves after primary stapes surgery, some patients redevelop conductive hearing loss after surgery and revision surgery is needed. ◦ The surgical procedure is performed in an area where cranial nerves VII, VIII, and X can be damaged by trauma or by swelling after surgery. ▪ Assess for facial nerve damage or muscle weakness. Indications include an asymmetric appearance or drooping of features on the affected side of the face. Ask the patient about changes in facial perception of touch and in taste.▪ Vertigo, nausea, and vomiting usually occur after surgery because of the nearness to inner ear structures Communicating with a Hearing-Impaired Patient ◦ Position yourself directly in front of the patient. ◦ Make sure that the room is well lighted. ◦ Get the patient's attention before you begin to speak. ◦ Move closer to the better-hearing ear. ◦ Speak clearly and slowly. ◦ Do not shout (shouting often makes understanding more difficult). ◦ Keep hands and other objects away from your mouth when talking to the patient. ◦ Have conversations in a quiet room with minimal distractions. ◦ Have the patient repeat your statements, not just indicate assent. ◦ Rephrase sentences and repeat information to aid understanding. ◦ Use appropriate hand motions. ◦ Write messages on paper if the patient is able to read. Elimination RENAL Focus Note for Exam 5 – Elimination AKI: pre/intra/post; s/s/nutrition; oliguric phase ◦ Most common in acute care setting and more likely to occur in older adults who are hospitalized who have a preexisting condition. ◦ the severity of AKI is based on increases in serum creatinine and decreased Urine output. ▪ Why if GFR not the case here – NOT ACCURATE ENOUGH! ◦ CAUSED BY - Reduced perfusion to the kidneys ▪ The longer the patient is olguric or anuric the less likely they will recover from AKI ◦ SIGNS AND SYMPTOMS – the patient may have manifestations of fluid overload (because in AKI, fluid is not eliminated) including pulmonary crackles, dependent and generalized edema, decreased oxygenation (low peripheral oxygenation or SpO2), increased respiratory rate, and dyspnea – assessment related to fluid overload. ◦ TREATMENT: ▪ Fluid challenges are often used to promote kidney PERFUSION.▪ In patients without fluid overload, 500 to 1000 mL of normal saline may be infused over 1 hour. ▪ Patients with AKI often require central venous pressure (CVP) monitoring. ▪ Diuretics may be used to increase urine output in AKI if renal function is adequate Diuretic-induced urine output does not preserve kidney function or stop AKI They do rid the body of retained fluid and electrolytes in the patient with AKI that has not progressed to end staged renal disease ▪ Calcium channel blockers may be used to treat AKI resulting from nephrotoxins ◦ Types of AKI/etiologic categories: ▪ Prerenal – Caused by reduced perfusion/blood flow to the kidneys, Most common cause of AKI in acute care and can be reversible if detected early. – caused by severe dehydration, circulatory collapse – MI, hypovolemia, or shock ▪ Intrarenal – Damage to kidney tissues and reflects injury to the glomeruli, nephrons, and tubules. – ischemia, nephrotoxins, and conditions like acute glomerulonephritis or other severe infections are usually the cause ▪ Postrenal –Obstruction of urine flow – example would be BPH as a cause or renal calculi, tumors. ◦ Rapid decrease in kidney function leads to collection of metabolic wastes in the body ▪ Oliguria Urine output of less than 400ml/day ▪ Azotemia Retention and buildup of nitrous waste in the blood ◦ Calculation of Mean Arterial Pressure (MAP) ▪ MAP = (SBP + [2 × DBP]) ÷ 3 ▪ A normal range for MAP is 70-110 mm Hg for healthy adults. ◦ Nutrition therapy ▪ Patients who have AKI often have a high rate of catabolism (protein breakdown). Catabolism causes the breakdown of muscle for protein and increases azotemia. ▪ Many patients with AKI are too ill or their appetite is too poor to meet caloric goals For these patients, nutrition support is needed. Nutrition support can include oral supplements, enteral nutrition, or parenteral nutrition (hyperalimentation) ▪ a diet w/moderate protein restriction, high in carbohydrates (CHO) and RESTRICT potassium and sodium!! CKD: s/s; nutrition/labs. ESKD/very late signs: ◦ CKD BECOMES ESKD – end stage kidney disease or ESRD ◦ it is a progressive loss of renal function with a GFR of 60mL/min or less for 3 months or longer ◦ causes of CKD include ▪ DM, HTN, glomerulonephritis, autoimmune disorders, polycystic kidney disease, recurrent infection or urinary obstruction ◦ client will develop uremic syndrome because of accumulation of waste products in blood ▪ Azotemia – Buildup of nitrogenous waste in the blood. ▪ Uremia – Azotemia with clinical manifestations. Metalic taste in mouth, N/V, anorexia, ―Frost‖ on skin, edema, itching, dyspnea. ◦ Signs and symptoms: ▪ Early signs: nausea, apathy, weakness, and fatigue; declining UO leading to oliguria ▪ Late signs: possibly frequent vomiting, increasing weakness, lethargy, and confusion ▪ client may report restless leg syndrome, paresthesia, sensory loss ▪ kussmaul respiration’s with declining LOC (acidosis) ◦ Labs: ▪ elevated creatinine and BUN ▪ decreased creatinine clearance ▪ electrolyte imbalances hypernatremia, hyperkalemia, hypermagnesemia, hyperphosphatemia hypocalcemia metabolic acidosis occurs because impaired hydrogen ion exchange ▪ proteinuria, hematuria, and casts in urinalysis as well as fixed SP.G – 1.010 ▪ decreased platelets – causing anemia and fatigue due to loss of erythropoietin (think of the renin system!) ◦ Nutrition: ▪ diet low in protein w/supplemented amino acids – restrict fluids as prescribed ▪ diet low in potassium and sodium ▪ provide electrolyte replacement◦ prepare client for dialysis or kidney transplant ◦ medication therapy is limited by kidney’s inability to excrete Acute glomerulomephritis ◦ This is the leading cause for end stage kidney disease – a group of kidney diseases caused by inflammation of glomerular capillary membrane ◦ most often caused by infection (Usually strep infection); usually 10-14 days after infection ▪ immune system creates antigen antibody complexes – these complexes collect and inflame the glomeruli – leading to loss of renal function ▪ ages 2-10 is most common affected – pediatric ◦ SIGNS AND SYMPTOMS: ▪ Edema in hands, face, eyelids, crackles in lung fields, s3 (Gallop rhythm), neck vein distention. Assess for urine color….May be rust, smoky, cola colored. Mild to moderate hypertension. ▪ Think of this: H-A-D-S-T-R-E-P H – HTN A – ASO ―antistrepolysin‖ titer positive – TEST FOR STREP D – decreased GFR – low UO causing increase in potassium in body S – swelling in face and eyes/ mild edema – most common in the mornings T – tea colored urine, coke colored; hematuria!! R – recent strep infection E – elevated BUN and creatinine P – proteinuria (MILD) ◦ Laboratory assessment: ▪ Protein and red blood cells in the blood ▪ GFR may be decreased – causing HTN ▪ increased ASO titer and ESR ▪ increase waste in blood – BUN and creatinine (azotemia) ▪ serum potassium and BUN may be increased with patients with oliguria. ▪ Proteinuria – Protein in the urine – Patients with this will have 500mg – 3g in 24 hours for excretion.▪ Serum albumin levels are decreased because of the protein lost in the urine and the fluid retention causing dilution – hypoalbuminemia ◦ TX: ▪ Antibiotic therapy like PCN ▪ dialysis in extreme cases where uremic manifestations or fluid volume excess cannot be controlled – if disease promotes to renal failure ▪ diet high in CHO, potassium restriction in oliguria, sodium restriction for HTN/edema, protein restriction if azotemia is present ▪ Maintain hygiene, fluid and toileting. ◦ Plasmapheresis – Removal and filtering of the plasma to eliminate antibodies. Pyelonephritis – do not study heavy on ◦ acute or chronic infection of one or both kidneys ▪ usually begins in renal pelvis and may also affect parenchyma (functional portion of kidney) ◦ kidneys become edematous and abscesses may develop – tissue destruction primarily affects tubules ◦ acute form: ▪ active infection; bacterial infection – often from E.Coli ▪ usually ascends from lower urinary tract ▪ risk factors include: pregnancy, urinary tract obstruction from stones, congenital malformation – spinal cord injury, urinary tract trauma, catheter placement, calculi, diabetes mellitus, asymptomatic cystitis ▪ SIGNS AND SYMPTOMS fever, chills, tachycardia, tachypnea, flank, back, or loin pain – costovertebral pain, abdominal discomfort, nausea and vomiting, urgency, frequency, nocturia, general malaise or fatigue ◦ chronic form: ▪ associated with recurrent acute infections and sometimes with metabolic, chemical, or immunologic disorders ▪ SIGNS AND SYMPTOMS Hypertension, Inability to conserve sodium, Decreased ability to concentrate urine, Development of hyperkalemia and acidosis – also can see some S/S associated with acute Nephrotic syndrome◦ Condition of increased glomerular permeability, allowing larger molecules such as protein to pass through into the urine. ◦ Characterized by MASSIVE proteinuria, hypoalbuminemia, hyperlipidemia, and SEVERE edema of dependent tissues, face, and periorbital areas ▪ ** you see more edema in this than you do in glomerulonephritis because you lose more proteins in nephrotic syndrome – albumin in the blood stream messes with oncotic pressure ◦ Seen with renal condition that damages glomerular capillary membrane; glomerulonephritis, lipoid nephrosis, syphilitic nephritis, SLE, DM ▪ Most common causes are immune/inflammatory process and genetic defects ◦ Causes massive loss of protein, edema, and decreased albumin level ▪ albumin is the biggest protein we lose ▪ others lost: immunoglobulins and proteins that help decrease clot formation risk for infection and risk for clotting ◦ SIGNS AND SYMPTOMS ▪ Massive proteinuria – >36/day ▪ foamy/frothy urine – dark yellow ▪ hypoalbuminemia causing edema, lipduria, hyperlipidemia ▪ Increased coagulation ▪ reduced kidney functions. ▪ Liver will try and compensate because of the hypercoagulable state (antithrombin III) and it will also say hey I need to make more proteins and makes more lipids so in turn you will see hyperlipidemia, thrombosis in veins, DVTs or Pulmonary embolus ◦ TREATMENT: ▪ Immunosuppressive agent ▪ ACE inhibitors ▪ Heparin ▪ Diet changes Mild diuretics GFR...everything: what triggers it/inhibits it/etc. ◦ a test used to check how well the kidneys are working ▪ Specifically, it estimates how much blood passes through the glomeruli each minute. ▪ Glomeruli are the tiny filters in the kidneys that filter waste from the blood. ▪ A GFR of 60 or higher is in the normal range. A GFR below 60 may mean kidney disease. A GFR of 15 or lower may mean kidney failure. ◦ Creatinine (0.6-1.3) is a specific indicator of GFR and renal status ◦ BUN (10-20) rises with reduced glomerular filtration rate (GFR)◦ GFR is 125ml/min – is blood Nephrotoxic drugs ◦ cisplatin (platinol) ◦ acetaminophen (high doses) ◦ NSAIDS!! ◦ some antibiotics ▪ vancomycin, IV ▪ aminoglycocides – gentamycin ▪ acyclovir ▪ ciprofloxin ▪ sulfonamides ◦ methotrexate – cancer drug ◦ ace inhibitors – catopril ◦ radiologic contrast media and heavy metals – IV contrast dye ◦ myoglobin from body ◦ avoid alcohol – adds to nephrotoxicity drugs from Ticket-to-test – study work sheets ◦ Alucap ▪ (aluminum hydroxide) ▪ a phosphate binder which contains aluminum. ▪ It is very effective at binding phosphate, but if taken over a long period of time, aluminum can build up in the body, possibly causing memory problems. ▪ Your doctor will measure your aluminum levels if you take Alucaps. ▪ Side effects of Alucaps include constipation. ▪ Alucaps should be swallowed whole 10-15 minutes before meals. ◦ Phosex ▪ (calcium acetate) is another phosphate binder which contains calcium.▪ It should be swallowed whole and taken 10-15 minutes before meals. ◦ Renagel ▪ (sevelamer) is a phosphate binder which doesn’t contain calcium or aluminum. ▪ The tablets should be swallowed whole with meals. ◦ Medicines for electrolyte imbalances ▪ Kayexelate ▪ Potassium chloride ▪ Magnesium Sulfate ◦ Diuretics: ◦ Loop diuretics: ▪ Furosemide (Lasix) ▪ Bumex ▪ Demadex ◦ Thiazide and thiazide like diuretics: ▪ Hydrochlorothiazide (Hydrodiuril) ▪ Diuril ◦ Osmotic Diuretics: ▪ Mannitol ◦ Carbonic Anhydrase Inhibitors: ▪ Diamox ◦ Potassium Sparing diuretics: ▪ Aldactone ▪ Inspra ◦ Note that…..ACE inhibitors and ARBs may be used if you have protein in your urine (proteinuria) or have heart failure. Regular blood tests are required to make sure that these medicines don't raise potassium levels (hyperkalemia) or make kidney function worse. Review your hormones/what triggers them/inhibit them: aldosterone/Renin/ADH/etc. ◦ Renin: ▪ released primarily by the kidneys ▪ stimulates the formation of angiotensin in blood and tissues, which in turn stimulates the release of aldosterone from the adrenal cortex. ▪ Both renin and erythropoietin play a role in the function of the parathyroid hormones and vitamin D ▪ It also converts vitamin D to an active form for calcium absorption and regulation of parathyroid hormones ◦ Kidney Blood Supply: ▪ Renin - Hormone produced by granular cells. Raises blood pressure as result of angiotensin (local vasoconstriction) and aldosterone (volume expansion) secretion. Renin assists in blood pressure control. It is formed and released when there is a decrease in blood flow, blood volume, or blood pressure through the renal arterioles or when too little sodium is present in kidney blood. These conditions are detected through the receptors of the juxtaglomerular complex, DCT (macula densa). ◦ THE SYSTEM: HOW IT WORKS ▪ Renin changes Angiotensinogen to angiotensin I ▪ then ACE (angiotensin converting enzyme) converts Angiotensin I to Angiotensin II which is a potent vasoconstrictor. ▪ Angiotensin II also stimulated the production of aldosterone. ▪ Aldosterone then stimulates the DCT to reabsorb Sodium and excrete potassium. ▪ This additional sodium increases water reabsorption and increases volume and BP. ▪ Thus returning the BP to normal and once this happens the stimulus for renin production is removed. ◦ Aldosterone: – retains H2O and Na ▪ helps regulate FLUID AND ELECTROLYTE BALANCE by increasing kidney reabsorption of sodium and water and restoring blood pressure, blood volume, and blood sodium levels. ▪ It also promotes excretion of potassium. ▪ Increases in serum potassium stimulate the secretion of aldosterone. ▪ Aldosterone stimulates DCT to excrete the extra potassium and the serum potassium return to normal. ◦ ADH – antidiuretic hormone – retains H2O ▪ Vasopressin or antidiuretic hormone (ADH) is a nonapeptide that is synthesized in the hypothalamus▪ plays important roles in the control of the body’s osmotic balance, blood pressure regulation, and proper kidney function. ▪ ADH primarily affects the ability of the kidney to reabsorb water A slight elevations in osmolarity result in secretion of ADH; ADH then acts primarily in the kidneys to increase water reabsorption thus returning the osmolarity to baseline ▪ released when BP is decreased: dehyration, hypovolemia, shock – ADH will decrease urinary output and make urine darker Conference for Exam 5 – Elimination ADH – water ADH ◦ controlled by osmolality ◦ level: 280-300 ◦ decrease osmolality – you are more concentrated so you need to add water ◦ increase osmolality – you are more diluted so you need to take away water ◦ if you are dehydrated, or have a low BP – ADH is released; this is the trigger ◦ if you have a high BP, fluid volume overload – ADH is suppressed; it stops being released ◦ thirst kicks in first; ADH kicks in last; critically ill ◦ ADH comes from hypothalamus ◦ increased sodium retention thereby increasing osmolality in the Extra cellular compartment – water follows sodium – this makes us thirsty and then ADH is stimulated (LAST) renin – angiotensin – aldosterone system (R-A-A-S) ◦ controlled by blood volume ◦ hypovolemia ◦ angiotensin is made by the liver ◦ without Renin angiotensinigen can NOT convert to angiotensin 1 ◦ angiotensin 1 goes to 2 – angiotensin 2 triggers/stimulates aldosterone making tubules more pearmable to water ◦ aldosterone works where water can not move in and out – loop of henle and in the DCT – ▪ aldosterone excretes K and keeps Na and H2Oextra notes ****sympathetic activity increases blood volume thereby increasing cardiac output SERUM NOW with ADH ◦ decrease serum osmolality; ADH is suppressed it is stopped! – we lose water and then this will raise osmolality ◦ Increase serum osmolality; ADH is triggered – we get water and then this will decrease osmolality in the serum hypotonic – decrease osmolality; we will see thirst medullary is very salty place in kidney Nephritic syndrome (glomerulophelbitis) ◦ inflammation in glomeruli ◦ not filtering right so < GFR – because all cells are inflammed ◦ S/S: ▪ HTN, oliguria (<400ml in 24hr), azotemia (waste: >BUN/Creatinine), blood and mild protein in urine, hypervolemia – JVD, crackles in lungs, other signs and symptoms of fluid overload ◦ diet: restrict water if there is a negative fluid balance, low salt and potassium maybe, low protein – based on labs Nephrotic syndrome ◦ destruction of the potocytes in glomeruli ◦ massive protein will leak ◦ hypoalbuminemia – losing MASSIVE proteins into the blood ▪ hyperlipidemia – @risk for DVT, PE, and MI ◦ urine is a frothy/foam dark yellow ◦ massive edema due to albumin leaving and going into the blood vessels (albumin regulates oncotic pressure) ◦ diet: give water, give protein, decrease fat AKI ◦ high rate of catabolism ▪ very high rate of protein breakdown▪ look at uremia and azotemia – urea and nitrogenous waste ◦ DIET: decrease protein in AKI – decrease sodium and potassium; fluid retention is based on urine output – if it is a low UO then hold fluid, they get nepro – as a supplement CKI: ◦ protein and caloric intake – depends on status ◦ diet varies according to the degree of kidney function and type of medication treatment (dialysis) – control proteins, fluid retention depending on UO, K, PO, Na restrictions ◦ they look at your GFR, BUN, Creatinine – also look at uremia and azotemia ◦ ESKD – need more protein because protein is lost by dialysis; tailored by patients dry weight – weight post dialysis; restrict PO, K, Na Polycystic kidney disease – PKD ◦ genetic inherited ◦ fluid fill cyst on tubules – kidneys can enlarge really big; incurable ◦ cyst cause HTN – decrease sodium intake; control of HTN is the top priority with PKD ] ◦ give or increase fiber due to displacement of the kidney that is enlarged; constipation is a big symptom kidney biopsy – do not bleed; watch bleeding during this surgery since kidney is highly vascular Labs for renal and diagnostics Polycystic kidney disease Nephritis, Nephrotic syndrome Acute and chronic glomerulonephritis Chronic kidney disease AKI ESKD- Types of Dialysis, peritoneal dialysis, AV shunts, vas caths Nephrosclerosis Cardiac perfusion Cardiac cycle, afterload, pre-load, which meds increase or decrease afterload, pre-load, Contractillity, conduction, chronotropes, dromotropes. How do these ultimately effect cardiac output and tissue and organ perfusion. --- look at drugs at bottom of study guide Basic dysrhythmias; Sinus bradycardia, Sinus Tachycardia, PAC, PVC, Afib, Aflutter, SVT, V-tach, V-fib, Torsades, asystole, PEA, Heart blocks, paced rhythm. Causes of arythmias and immediate treatments. Which ones are more lethal than the others. – ******LOOK AT DYSRHYTHMIA SHEET Coronary artery disease and Myocardial Infarction: ST elevation, St depression, Q wave or non q wave MI, Cardiac biomarkers-which ones elevated first or stay elevated, Cardiac catheterization for diagnostic and intervention, Other diagnostic tests. Cardiac assessment: Heart sounds S1, S2, S3, S4, murmurs, angina, MAP, starlings law, Chest pain, Cardiac diet: prudent diet Pacemakers Basic heart failure; Right and left heart failure Valvular DZ Cardiomyopathies • PVD/DVT/PE • Brain attack (stroke) Focus Notes for Exam # 7 Perfusion Medications: Adenosine ◦ adenocar. ◦ vagal 1st though!! before giving this drug ◦ dosage is 6mg-12mg-12mg; give rapid, bolus, fast in a syringe ◦ for SVT Amiodarone ◦ specific function; antidysrhytmic ◦ Class III potassium channel blockers are meds that delay repolorization may cause – prolonged QTI ◦ has a lot of iodine in it and will affects the thyroid gland – Hypo or hyperthyroid gland; iodine helps make TSH thyroid. ◦ LONG TERM WILL CAUSE LUNG ISSUES; PULMONARY FIBROSIS ASA ◦ acute MI (plaque in artery – clot that forms afterwards causes blockage) ◦ ASA stops the clot – plt forms a plug ◦ reduces platelet aggregation - ◦ for STROKE ASA is used for prophylaxsis Atropine ◦ 0.5mg is the dose◦ used for bradycardia; to increase heart rate ◦ anticholinergic and antidysrhythmic BBB ◦ decreases afterload; ◦ increase ventricular filling; by decreasing systemic vascular resistance ◦ decreases heart rate, decreases BP, decreases afterload ◦ Decrease HR,Decrease Myocardial contractility, Decrease rate of conduction through AV node ◦ Reverse effects of prolonged exposure to increased levels of sympathetic stimulation and catecholamines CCB ◦ Diltiazem; cardizem ◦ lower BP by vasodilation ◦ increases cardiac output by decreasing the excitability of the heart Digoxin ◦ cardiac glycoside; ◦ inhibits sympathetic activity while enhancing parasympathetic activity ◦ do not block ion channels; slows heart rate (slows conduction through AV node – leading to increased SV/CO) ◦ increases force and efficiency of myocardial contraction/improving SV&CO ◦ SQUEEZE HEART; used for afib and aflutter Diltiazem ◦ used to treat rapid afib and aflutter ◦ watch for slowing of heart rate (bradycardia) ◦ can also drop BP ◦ AV node will reset and go back to NSR with IV diltiazim (cardizem) ◦ can take anticoagulants with this drug if they do not go back to NSR ◦ (those who are on afib and stable; GIVE ANTICOAGULANT) Dopamine ◦ (for heart failure…positive sign; positive inotrope) ◦ good for HF or shock ◦ in low doses very good to perfuse kidneys; high dose vagal constriction (emergency situations) ◦ IN HF IS GOOD; helps with low dose PERFUSE KIDNEYS ◦ renal perfusion – good urine output ◦ helps squeeze the heart and good for renal perfusion Epinephrine ◦ fight or flight drug; ◦ SYMPATHETIC NERVOUS SYSTEM;◦ adrenalin – give for anaphylaxis ◦ increases heart rate ◦ used in vtach and vfib; last resort if chest compressions or shock did not help ◦ saves heart tissue ◦ used in asystole too for cateocholamines ◦ dose 1mg repeat as necessary Heparin ◦ prevents clotting ◦ anticoagulant ◦ look at PTT (partial thromboplastin time) ▪ 60-70 seconds ◦ PROTAMINE SULFATE IS ANTIDOTE Lidocaine ◦ class I antidysrhythmics acts by blocking sodium ion channels in myocadia ◦ slows the spread of impulse of conduction across the heart ◦ ventricular dysrhythmias (like vtach) ◦ CAN NOT TREAT ATRIAL ARRYTHMIAS (CONTRAINDICATED IN SVT) ◦ IT IA LARGELY INEFFECTIVE OR HARMFUL Morphine ◦ MONA (morphine) acute myocardial infarction ◦ BP too low; can NOT give morphine Nitrostat/nitrates ◦ decrease both preload and afterload ◦ choose nitro over morphine if you had to choose ◦ (say someone had a low BP and did not want to bottom out – choose nitro over morphine) ◦ patch is long acting or can use sublingual; ◦ it is a vasodilator seen in MI or angina ◦ angina or chest pain is seen have EKG 1st and give nitro sublingual ◦ after giving nitro must assess PAIN FROM PAIN SCALE ◦ may give up to 3 tabs; after three tabs if pain still persist must sought HCP – ◦ ALWAYS ASSESS BP ◦ TAKE NITRO SITTING DOWN; wait 5 minutes and take 2nd dose if needed Warfarin ◦ coumadin; anticoagulant ◦ those who have DVT; ◦ look @ PT (prothrombin time) and INR for blood levels ▪ INR 1-2 (2-3 for those on drug)▪ PT 11-12.5 ◦ can give with heparin drip in order to get it to a therapeutic level ◦ know total cholesterol/HDL/LDL/Triglycerides HDL?? Nutrition/Teaching: CAD o blood flow is partially blocked – can result inschemia o artheroscleorsis – hardening of arteries Cardiomyopathy o teach to eat healthy heart diet; DASH diet – Low in Saturated fats/Total fats; High in fruits, veggies, and low fat dairy o Low cholesterol Procedures/teaching/pre-post op/nursing interventions: Angiography o replacing occluded coronary artery; trying to expand it Cardiac heart catheterization o diagnostically or cath done in EMERGENCY to open vessel – balloon o femoral arteries, know how to take care of patient with cardiac cath o head of the bed elevated up to 30° during bedrest o remain in bed for 2 - 6 hrs o vitals q15min for first hr then q30 mins for 2 hours or VS stable o look for hematoma o dorsal pedialis and posterior tibial pulses to see if still getting blood flow there/a PULSE can’t find it? check with a doppler before calling HCP Diagnostic testing for valvular disease o results – in notes; o valvular disease chest xrays o aortic stenosis o ventricular hypertrophy, o regurgitation, o large left ventricle caused by blood backing up because aortic valve is stenotic (chest x-ray shows anterior of the heart) Mitral valve replacement (assessment) o know what side of heart it is on; if valve is not working then you will have symptoms of aortic valve stenosis o Mitral stenosis MS- causes valve thickening by fibrosis and calcification. valve stiffens fusses, chrodea tendinae contract & shorten. opening narrows- LA pressure increases -LA dilates -Pulmonary artery pressure increases – RV hypertrophy o mitral regurgitation MR-(insufficiency) fibrotic and calcific changes prevent the MV from closing completely during systole! compensate for increase volume/pressure, the LA and LV dilate & hypertrophy primary cause- degeneration r/t aging & endocarditis – more common in women, takes years (decades to progress) SYSTOLE: backflow of blood into the LA when LV contracts DIASTOLE: regurgitant output again flows from the LA to LV (+) normal blood flow amount TEE o transesophageal --- tube down esophagus that echo can not show o must be NPO Be able to figure out cardiac output!! CO = HR x SV – normal cardiac output is between 4-7 L/min (varies on size of person; active) – MAP 60-70 mm Hg Labs: BNP o SEEN IN LEFT SIDED HF Cardiac enzymes o troponin T is <0.10 and troponin I is <0.03 this is too look at cardiac muscle; if elevated it can indicate heart attack o Creatine kinase (CK) : Females: 30-135 units/L Males: 55-170 units/L Values higher after exercise Elevations indicate possible brain, myocardial, and skeletal muscle necrosis or injury. Total cholesterol/HDL/LDL/Triglycerides: o Total cholesterol less than 200 mg/dL o Triglycerides: MEN: 40-160 mg/dL FEMALE: 35-135 mg/dL o HDL (―good‖ cholesterol) greater than 60 (average) o LDL (bad cholestrol) less than 130 Conditions related to PERFUSION: Preload/afterload: what can increase it or decrease it o increase preload: IV like NS – IV, blood, dopamine and epi and HTN can increase afterload (anything that increases BP) o NON-Surgical ways to REDUCE preload and afterload CPAP- improve sleep apnea & improve CO/decreases preload & afterload Nonsurgical management relies primarily on a variety of drugs – nitro/BB/anything that is a vasodilator o SURG ways to REDUCE preload and after load CABG VADs (ventricular assist devices) – has a battery! o Preload: STRETCH -amount of blood return to heart from venous system (right heart) & pulmonary system (left heart) *left ventricular end-diastolic [LVED] volume* o Afterload: PRESSURE -pressure/resistance the ventricles must overcome to eject blood through the semilunar valves & into the peripheral blood vessels Pulmonary Embolism – ddimer is lab assessment; d-dimer, a fibrin split product, rises with fibrinolysis. When the value is normal or low, it can rule out a PE o Pulmonary angiography is the ―gold standard‖ diagnostic test o other test include: CT-PA, or helical (spiral) CT, VQ scans (assess iodine allergy/contrast dye used) o S/S – Classic Manifestations Dyspnea, sudden onset, Sharp, stabbing chest pain Apprehension, restlessness/ Feeling of impending doom Cough/ Hemoptysis o Signs Tachypnea/Crackles/Pleural friction rub Tachycardia/S3 or S4 heart sound Diaphoresis/Fever, low-grade Petechiae over chest and axillae Decreased arterial oxygen saturation (Sao2) o teaching/preventions of DVT therefore reducing PE risk Ambulate patients soon after surgery Start passive and active range-of-motion exercises for the extremities of immobilized pts. SCDs – increase venous flow change positions q2hrs do not massage leg muscle do not cross legs quit smoking prophylactic drugs: anticoagulants and antiplatelets o treatment DO NOT USE SCDs or ambulate – if DVT has formed; this can cause it to break off forming a PE apply O2 by NC or Mask!! put high fowlers position assess lung sounds and cardiac sounds at least every 30 min drug therapy: anticoagulants to preven embolus enlargement and more clots LMWH or ariztra alteplase (fibrinolytic drugs/activase) is uesd when specific criteria is met – shock, hemodynamic collapse, or instability o this drug breaks up the existing clot! Surgery interventions: embolectomy or IVC filtration w/placement of vena cava filter Pericarditis/ Aortic Stenosis – o pericardial effusion: space btw the parietal & visceral layers of the pericardium fills w/ fluid o cardiac tamponade: excessive fluid w/in the pericardial cavity (EMERGENCY) S&S of cardiac tamponade: JVD paradoxical pulse (systolic blood pressure 10 mm Hg higher on expiration than on inspiration) Decreased heart rate, dyspnea, & fatigue Muffled heart sounds Hypotension o stenosis or regurgitation of the mitral & aortic valves – S&S Tachycardia Cardiomegaly (enlarged heart) Development of a new murmur or a change in an existing murmur Pericardial friction rub precordial painprolonged PR interval indications of HF Evidence of an existing streptococcal infection Heart sounds: S3, S4 what causes them – o S1: closure of the tricuspid and mitral valves (AV valves close, semi-lunar valves open) systolic!! CONTRACTION o S2: closure of the aortic and pulmonic valves (semiluner close, AV valves open) diastolic!! RELAXATION o heard with cardiomyopathy – S3 and S4 o S3 ventricular gallop (normal finding in those younger than 35 y.o.) decreased LV; left sided HF ventricular gallop heard with pulmonary edema o S4 atrial gallop HTN anemia ventricular hypertrophy MI aortic/pulmonic stenosis PE OR older stiffened ventricle o Murmurs reflect turbulent blood flow thru valves Cardiomyopathy: hypertrophic – normal heart rate; able to stretch that ventricle and cardiac output is great – too much stretching can be bad!! o Medication/Teaching/nursing interventions -- o dilated cardiomyopathy (DCM) most common type Fibrosis of myocardium & endocardium, Dilated chambers, Mural wall thrombi prevalent (sudden or asymptomatic for months-years) S&S Fatigue and weakness Heart failure (left side) Dysrhythmias or heart block Systemic or pulmonary emboli S3 and S4 gallops Moderate to severe cardiomegaly Treatment: Symptomatic treatment of heart failure Vasodilators Control of dysrhythmias Surgery: heart transplant o hypertrophic cardiomyopathy (HCM) asymmetric ventricular hypertrophy & disarray of the myocardial fibers grows too QUICK (muscle gets really thick, bottom of ventricles will pump same amount of blood; problem occurs when young person goes into exercise issue) S&S: Dyspnea Angina Fatigue, syncope, palpitations Mild cardiomegaly S4 gallop Ventricular dysrhythmias Sudden death common Heart failure treatment For both: nonobstructed & obstructed Symptomatic treatment Beta blockers Conversion of atrial fibrillation Surgery: ventriculomyotomy or muscle resection with mitral valve replacement Nitrates and other vasodilators contraindicated with the obstructed form o restrictive cardiomyopathy rarest- stiff ventricles that restrict filling during diastole S&S = same as left/right HF cause: endocardial or myocardial disease IE: sarcoidosis or amyloidosis o arrhythmogenic right ventricular cardiomyopathy (dysplasia) cause: replacement of myocardial tissue w/ fibrous & fatty tissue Deep venous thrombosis o teaching, – look at pulmonary embolism too for teaching/preventative measures o S/S include: Reddened, Discolored, Warm Skin, Swelling in the affected leg, Pain in your leg o VIRCHOW’S TRIAD 1. hypercoaguability: too many RBCs/plts, dehydrated pts cancer, estrogen therapy, PP period, acute phase post-op 2. endothelial damage: surgery from crush injury, CAD/plaque build up surgery, trauma, artherosclerosis, heart valve disease 3. venous stasis: immobility paralysis, HF, venous insufficient/varicose veins, venous obstruction (tumor, pregnancy, or obesity) Risks factor for CAD – know between modifiable or non-modifiable (ex: diet vs. genetics) o -non-mod: Age, Gender, Ethnicity, Family history, Genetics o -mod: Elevated lipid levels, HTN, Tobacco/smoking, Physical inactivity, Obesity, Diabetes Shock (look at box) o Warm fluids…why? keep from shivering on acidosis which causes vasodilation – so when we warm cause vasoconstriction; helps with perfusion o Hypovolemic hemorrhagic or severe fluid loss D/V decrease central venous pressure; compensate increase cardiac output//heart rate weak rapid pulse is a late sign that patient is getting more blood/body fluid depleted Hgb/Hct low MAP must be around 65 give IV or blood o Cardiogenic pump failure; heart itself – extensive heart attack ventricular arrhythmias that keep occuring; not the volume!!!!!! pump is failing!! low; dont fix with IV fluids; cardiac cath lab – positive inotropes; dopamine or amidorone; digoxin o Neurogenic spinal cord injury; our brain is the CNS it is how we do things; sympathetic tone is to blame; has bradycardia because CAN NOT COMPENSATE; treatment involves atropine, inotrops dopamin; vasopressors o Chemical anaphylaxis – epi!! histamines!! Sepsis; increase lactate levels, increase bands, increases BUN/Ct; skin goes from warm shock to cold shock (stops compensating) severe sepsis: increase CO, decrease CVP, BP normal septic shock decrease CO, CVP, BP, Pulse pressure, UO toxings and endotoxins release into blood causing SIRS metabolism becomes aerobic because of decreased MAP treat hyperglycemia because bacteria love sugar o Obstructive: pulmonary embolus or cardiac tamponade Heart Failure look in notes o S/S, Teaching daily weights!! – same time each morning! o Right and left heart failure (know differences) – if you have left sided HF you have Right sided problems (ex: pulmonary edema/crackles) – if you have right sided HF you have leftsided problems (ex: peripheral edema/weight gain) – if you have both sides then you have both S/S Know S/S, treatments! o Left sided: confusion, pulmonary congestion, crackles, frothy pink sputum TX: drugs that decrease afterload; vasopressor/epi/dopamine/nitrates o Right sided: weight gain, JVD, peripheral edema, decreased blood to lungs, tired and fatigue (due to decrease oxygen) TX: weight daily, decrease sodium in diet o S/S of activity intolerance generalized weakness, weak pulse, SOB, exertional dyspnea, failure to increase BP with activity Stroke – LOOK at notes o History of TIAs at risk for what – risk for stroke o Know what makes each stroke different: second major classification of stroke is hemorrhagic stroke. In this type of stroke, vessel integrity is interrupted and bleeding occurs into the brain tissue or into the subarachnoid space. hemorrhagic: has two types!! Intracerebral hemorrhage (ICH) describes bleeding into the brain tissue generally resulting from severe or sustained hypertension Elevated blood pressure (BP) leads to changes within the arterial wall that leave it likely to rupture. Subarachnoid hemorrhage (SAH) is much more common and results from bleeding into the subarachnoid space—the space between the pia mater and arachnoid layers of the meninges covering the brain. This type of bleeding is usually caused by a ruptured aneurysm or arteriovenous malformation It can also be caused by trauma. Ischemic: 2 types!! An acute ischemic stroke is caused by the occlusion (blockage) of a cerebral artery by either a thrombus or an embolus. A stroke that is caused by a thrombus (clot) is referred to as a thrombotic stroke o commonly associated with the development of atherosclerosis in either intracranial or extracranial arteries (usually the carotid arteries). o Atherosclerosis is the process by which fatty plaques develop on the inner wall of the affected arterial vessel. o Rupture of one or more plaques promotes clot formation. When the clot is of sufficient size, it interrupts blood flow to the brain tissue supplied by the vessel causing an ischemic (occlusive) stroke. a stroke caused by an embolus (dislodged clot) is referred to as an embolic stroke.o caused by a thrombus or a group of thrombi that break off from one area of the body and travel to the cerebral arteries via the carotid artery or vertebrobasilar system o Emboli can occur in patients with atrial fibrillation, heart valve disease, mural thrombi after a myocardial infarction (MI), or a prosthetic heart valve. o Emboli tend to become lodged in the smaller cerebral blood vessels at their point of bifurcation or where the lumen narrows. o middle cerebral artery (MCA) is most commonly involved in an embolic stroke o Community teaching/warning signs/cultures – BE FAST – balance, eyes, face, arms, speech, time balance: lost of balance, HA/dizzy eyes: blurred vision face: one side of the face is drooping arms: weakness speech: difficult time: transport! American Indian/Alaskan Native groups have the highest prevalence of stroke. African Americans have more risk of strokes than other cultures Black men and women have more strokes than white men and women. o stroke vocabulary: hemiplegia (paralysis on one side of the body) hemiparesis (weakness on one side of the body) a left hemiplegia or hemiparesis indicates a stroke in the right cerebral hemisphere and vis versa difficulty chewing or swallowing foods and liquids (dysphagia) dysarthria (slurred speech) Expressive (or nonfluent) – Difficulty speaking/Difficulty writing motor, aphasia – Broca’s Receptive – difficulty understanding spoken or written words sensory, aphasia – Wernicke’s o Teaching family about fibrinolytic treatment determine if the patient has had a recent bleeding event or is taking an anticoagulant is an important part of the rapid stroke assessment protocol. NIH stroke scale GCS: eye response/4, verbal response/5, motor response/6 – total of 15 open spontaneously, verbal command, pain, no eye open orientated, confused, inappropriate wrds, incomprehensible sounds, none obeys commands, localising pain, w/drawal from pain, extension to pain, none EKG/Rhythms/Meds/Treatment/Nursing Interventions Look at your patient 1st!!!!! Pulseless electrical activity (PEA)◦ Electrical activity can be observed on the ECG, but there is no mechanical activity of the ventricles and the patient has no pulse. ◦ The absence of a detectable pulse and blood pressure ◦ CPR followed by intubation and IV epinephrine ◦ Atropine is used if the ventricular rate is slow Pacemakers: Transvenous/external Teaching (go over teaching in lecture notes) EKG: P, QRS, T represents what? ◦ P: atrial depolarization ▪ The shape of the P wave may be a positive, negative, or biphasic (both positive and negative) deflection, depending on the lead selected. ▪ When the electrical impulse is consistently generated from the sinoatrial (SA) node, the P waves have a consistent shape in a given lead. ▪ If an impulse is then generated from a different (ectopic) focus, such as atrial tissue, the shape of the P wave changes in that lead, indicating that an ectopic focus has fired. ◦ PR segment: <0.20 seconds! ◦ QRS: <0.12 seconds! ▪ Ventricular depolarization ▪ The QRS duration represents the time required for depolarization of both ventricles. ▪ It is measured from the beginning of the QRS complex to the J point (the junction where the QRS complex ends and the ST segment begins). ▪ It normally measures from 0.04 to 0.12 second (up to three small blocks). ◦ T wave: ▪ ventricular repolarization ▪ It is usually positive, rounded, and slightly asymmetric. ▪ T waves may become tall and peaked, inverted (negative), or flat as a result of myocardial ischemia, potassium or calcium imbalances, medications, or autonomic nervous system effects. Strips on test ◦ Sinus bradycardia ▪ rate less than 60 beats/min ◦ Complete heart block ▪ No relationship between P waves and QRS complexes ▪ Relatively constant PP intervals and RR intervals ▪ Greater number of P waves than QRS complexes ▪ If symptomatic, transcutaneous pacemaker until a temporary transvenous pacemaker can be inserted ▪ Drugs (e.g., atropine, epinephrine): Temporary measure to increase HR and support BP until temporary pacing is initiated▪ Permanent pacemaker as soon as possible ◦ Symptomatic atrial fibrillation: treatment ▪ to convert AF to NSR: antidysrthmic drugs like CCB (diltiazem- cardizem) ▪ more difficult to control AF: amiodarone (cordarone) ▪ can also use digoxin ▪ Antidysrhythmic drugs used for conversion: Amiodarone, propafenone ▪ DC cardioversion may be used to convert atrial fibrillation to normal sinus rhythm ▪ If patient has been in atrial fibrillation for >48 hours anticoagulation therapy with warfarin is recommended for 3 to 4 weeks before cardioversion and for 4 to 6 weeks after successful cardioversion ◦ Atrial flutter ▪ Classic ―sawtooth‖ pattern ▪ Atrial rate fast and regular (250 to 350 beats/min) ▪ Ventricular rate slower ▪ Risk for stroke due to risk of thrombus formation in the atria ▪ Drugs to slow HR: Calcium channel blockers, Beta-adrenergic blockers ▪ Electrical cardioversion may be used to convert the atrial flutter to sinus rhythm emergently and electively ◦ Second degree heart block type 1/Wenkebach/Mobitz Type 1 ▪ Gradual lengthening of the PR interval ▪ then a drop in the QRS ▪ longer, longer, longer, DROP ▪ symptomatic, atropine or a temporary pacemaker ▪ asymptomatic, monitor with a transcutaneous pacemaker on standby ◦ Second degree type II/Mobitz II ▪ P-R intervals may be normal or prolonged, but they remain constant (will always be similar) ▪ Intermittent or unexpected blocked P waves you don’t know when QRS drops ▪ often progresses to 3rd degree (complete block) ▪ symptomatic (e.g., hypotension, angina) before permanent pacemaker can be inserted, temporary transvenous or transcutaneous pacemaker ◦ VT ▪ occurs with repetitive firing of an irritable ventricular ectopic focus ▪ Run of three or more PVCs ▪ Monomorphic, polymorphic, sustained, and nonsustained ▪ Considered life-threatening because of decreased CO and the possibility of deterioration ventricular fibrillation ▪ Rate: 101-250 beats/min▪ Rhythm: regular ▪ P waves: absent ▪ PR interval: none ▪ QRS duration: > 0.12 sec. often difficult to differentiate between QRS and T wave ▪ treatment include: CPR and rapid defibrillation; give EPI if defib is unsuccessful! ◦ VF ▪ result of electrical chaos in the ventricles and is life threatening! ▪ Impulses from many irritable foci fire in a totally disorganized manner so that ventricular contraction cannot occur. ▪ no recognizable ECG deflections ▪ patient becomes faint, immediately loses consciousness, and becomes pulseless and apneic (no breathing) ▪ DEFIB!!!! when I say V fib you say Defib – defib is the immediate action; if defibrillator is NOT READY; do high quality CPR until defibrillator arrives ◦ First degree heart block ▪ Prolonged AV conduction time ▪ PR interval > 0.20 seconds ▪ regular rhythm ▪ associated with: MI, CAD, Rheumatic fever, HyperTHY, vagal stimulation ▪ usually does not require treatment ▪ drugs: digoxin, BB, CCB, flecainide ◦ Asystole ▪ Immediate initiation of CPR and advanced cardiac life support (ACLS) measures with the use of defibrillation and definitive drug therapy ▪ can’t use a defibrillator because there are no electrical impulses! ▪ If carotid pulse is absent; 100 compressions/min depth of 2 inches ▪ give rescure breathes at a rate of 10-12/min ▪ ratio of 30:2 if standard airway is not in place ▪ 5 cycles or 2 minutes ◦ NSR/unifocal PVCs ▪ result from increased irritability of ventricular cells and are seen as early ventricular complexes followed by a pause ▪ unifocal: meaning that they are of the same shape ▪ multifocal: meaning that they are different shapes ▪ bigeminy (every other heart beat, 2nd is PVC) ▪ trigeminy (every two heart beats; 3rd is PVC) ▪ couplet: two sequential PVC – three or more are NSVT▪ MI, CHF, COPD, and anemia can be the causes for PVC – also hypokalemia or hypomagnesium ▪ Treatment Based on cause of PVCs; if no underlying heart disease; PVCs usually not treated (may avoid caffeine or stress) replace electrolytes (give MAG 1st when replacing electrolytes) ◦ Atrial fibrillation ▪ atrial fibrosis and loss of muscle mass ▪ Clinical associations Usually occurs with: Underlying heart disease, such as rheumatic heart disease, CAD Cardiomyopathy HF Pericarditis ◦ ST/SVT ▪ sinus tach: heart rate greater than 100 ▪ SVT is greater than 150 If SVT occurs in a healthy person and stops on its own, no intervention may be needed other than eliminating identified causes vagal maneuvers can be used 1st before drug adenosine is given (IV) DC cardioversion if vagal and drug therapy is innefective and/or if pt become hemodynamically unstable ◦ how to read a strip: ▪ Determine the heart rate ▪ Determine the heart rhythm – assess the R-R; is it regular or irregular ▪ Analyze the P waves are they present, are the occurring regularly, is there one for every QRS, are the absent or inverted ▪ PR intervals Are PR intervals greater than 0.20 second? Are PR intervals less than 0.12 second? Are PR intervals constant across the ECG strip? ▪ QRS interval are the less or greater tan 0.12 seconds are the complexes similar across strip ▪ T wave is it peaked or inverted MI and vent. Hypertrophy are seen with abnormal t waves ◦ pace maker terms ▪ Spike- electrical artifact noting electrical stimulation by pacer▪ Capture Pacer spike generates depolarization ▪ Sensitivity ability of pacer to recognize body’s intrinsic electrical activity ▪ Failure to pace pacer fails to initiate an electrical impulse ▪ Failure to capture pacer spike fires but no depolarization ▪ Failure to sense pacer does not sense patient’s own rhythm & initiates electrical impulse EXTRA NOTES FOR MADDIE TO REVIEW how blood flows through the heart: ◦ DE-OXY blood – SVC/IVC – RA – TRICUSPID – RV – PULM SEMI-L – Pulmonary trunk to lungs – OXY blood – 4 pulmonary veins – LA – MITRAL – LV – AORTIC SEMI-L – AORTA – TO BODY ◦ CORONARY SINUS – how blood flows to the myocardium (heart muscle) to get oxygenated ▪ coronary artery blood flow to the myocardium occurs primarily during diastole when coronary vascular resistance is minimized 3 mechanisms mediate/regulate BP: ◦ The autonomic nervous system (ANS), which excites or inhibits sympathetic nervous system activity in response to impulses from chemoreceptors & baroreceptors ◦ The kidneys, which sense a change in blood flow and activate the renin-angiotensin-aldosterone mechanism ◦ The endocrine system, which releases various hormones (e.g., catecholamine, kinins, serotonin, histamine) to stimulate the sympathetic nervous system at the tissue level Systolic BP- pressure/force generated by LV into aorta /each contraction Diastolic BP-pressure/force against the arterial walls during relaxation Hypertension (HTN) ◦ systolic 140 + ◦ diastolic 90+ ◦ take drugs to control BP Hypotension less than 90/60 ◦ Postural (orthostatic) hypotension decrease > 20 systolic or >10 diastolic; 10% - 20% increase in HR ▪ take BP pt supine at least 3 mins >>THEN>> pt changes position to sitting/standing Paradoxical BP- exaggerated decrease in systolic pressure by more than 10 mm Hg during inspiratory increased pulse pressure ◦ may occur in pts w/ slowHR, aortic regurgitation, atherosclerosis, HTN, & aging decreased pulse pressure ◦ heart failure, hypovolemia, shock, mitral stenosis or regurgitation hypOkalemia ◦ increased electrical instability, ventricular dysrhythmia, & increase risk for digitalis (cardiac glycosides i.e. DIG) toxicity hypERkalemia ◦ slowed ventricular conduction, peaked T waves & contraction followed by asystole (cardiac standstill) hypOcalcemia ◦ ventricular dysrhythmias, a prolonged QT interval, & cardiac arrest hypERcalcemia ◦ shortens the QT interval & cause AV block, digitalis (Dig) hypersensitivity, & cardiac arrest hypOmagnesemia ◦ ventricular dysrhythmias ―torsades de pointes‖, prolongs the QT interval, ventricular tachycardia Hematological Disorders – medical emergiences (exam 8)STUDY GUIDE FOR INCREASED ICP HEMATOLOGICAL, ANEMIAS, MEDICAL EMERGENCIES What is cushings triad? 3. Increased SBP 4. Decreased HR – BRADYCARDIA 5. Irregular slowed RESPIRATIONS – Bradypnea How does Mannitol work to reduce cerebral edema? • This osmotic diuretic produces selective diuresis used to reduce swelling and pressure inside the eye or around the brain. • May be rapidly administered IV to cause fluid to move by osmosis from the cranial cavity to the hyperosmolar concentration in the circulatory system • Increases the osmotic pressure of the glomerular filtrate, thereby inhibiting reabsorption of water and electrolytes. Why are hypotonic solutions avoided in increased ICP? • contraindicated because they add free water that might lead to cerebral edema and worsened ICP • hypotonic solutions (0.45% NaCl) causes solvent to move into cells outside of vascular bed; cell burst What is the Monro Kellie hypothesis? • ICP range: 5-15 mmHg (pressure with in the skull) • 3 components make ICP: brain tissue, CSF, and intracranial blood • the MONRO KELLIE HYPOTHESIS IS: that an increase in volume in any of the components must necessarily decrease the volume, in one or both of the other components • cerebral perfusion pressure (CPP) – blood flow to the brain • MAP – ICP = CPP • normal CPP range is 70-100 mmHg Complications of Increased ICP: • Brain Stem Herniation • Shifting of brain tissue from area of high pressure to area of low pressure; herniated tissue exerts pressure on the brain and disrupts blood supply in that area of the brain • Diabetes Insipidous • Occurs because there is not enough secretion of the Antidiuretic Hormone • SIADH (Syndrome of inappropriate ADH)• Occurs when there is TOO MUCH ADH secreted What are s/s of increased ICP? • Decreased LOC, behavioral changes, HA, N&V • changes in speech patter (aphasia, slurred speech) • changes in sensorimotor status ( Pupillary changes, dilated or blown pupils or contrictive non reactive pupils) • cranial nerve dysfuction, ataxia, seizure (usually within 24 hrs after stroke) • Cushing’s Triad • Abnormal Posturing (decerebrate or decorticate) • EARLY: deterioration of LOC, > Resp movements, weakness in 1 extremity, constant HA • LATE: LOC, changes in pupols, widening pulse pressure, pupil size, vomiting, seizures, impaired motor function HOB for ICP • The best HOB positioning has not yet been substantiated in the literature. • More studies are needed to determine best practice. • A reduced head elevation of less than 25 degrees can improve perfusion pressure to the damaged brain in ischemic conditions (most strokes). • However, a HOB elevation greater than 30 degrees can improve oxygenation and reduce aspiration risk. • So lets go with never lay them flat or in high fowlers. • keep HOB b/t 25 and 30 degrees. • Maintain head midline, neutral position, to help improve venous drainage from the brain. • Avoid sudden hip or neck flexion during positioning as this increases intrathorasic pressure leading to decreased cerebral venous outflow and increased ICP. • Extreme neck flexion also interferes with venous drainage from the brain and intercranial dynamics. Clotting • thrombin: • the principal enzyme of hemostasis • It catalyzes the conversion of fibrinogen to fibrin and activates procoagulant factors V, VIII, XI, and XIII.• Thrombin drugs act as clotting promoters, It can control minor bleeding during surgery. • Prothrombin: • a protein present in blood plasma which is converted into active thrombin during coagulation. • Prothrombin (factor II) is a vitamin K–dependent coagulation factor. • On activation, prothrombin is proteolytically cleaved to form thrombin, and in turn acts as a serine protease that converts fibrinogen to fibrin • fibrin • an insoluble protein formed from fibrinogen during the clotting of blood. • It forms a fibrous mesh that impedes the flow of blood. • When tissue damage results in bleeding, fibrinogen is converted at the wound into fibrin by the action of thrombin, a clotting enzyme. • Fibrinogen • a soluble protein that is produced by the liver and found in blood plasma. • a soluble protein present in blood plasma, from which fibrin is produced by the action of the enzyme thrombin • factor I • plasmin • an important enzyme present in blood that degrades many blood plasma proteins, including fibrin clots. • The degradation of fibrin is termed fibrinolysis. • plasminogen • the inactive precursor of the enzyme plasmin, present in blood. • Plasminogen is converted to plasmin by cleavage at the Arg561-Val562 peptide bond by tissue-type or urokinase-type plasminogen activator (tPA and uPA, respectively). Activation of plasminogen by tPA is the major pathway that leads to lysis of fibrin clots. How do these function in the clotting cascade. • Hemostasis is the multi stepped process of controlled blood clotting. It results in localized blood clotting in damaged blood vessels to prevent excessive blood loss while continuing blood perfusion to all other areas. Hemostasis starts the formation of platelet plug, end product is the formation of a fibrin clot. • Platelet aggregation begins forming a platelet plug by having platelets clump together. Activation causes platelet membranes to become sticky, allowing them to clump together – forming large, semisolid plugs in blood vessels disrupting local blood flow (NOT A CLOT THOUGH; last only a few hrs) • Blood clotting is a cascade triggered by the formation of a platelet plug • Intrinsic factors and Extrinsic factors: • look at picture • in summary: • there are two independent mechanisms for initiating blood coagulation and for activating factor X • (1) negatively charged surfaces that initiate blood clotting through the intrinsic pathway (factors XII, XI, IX, and VIII) • (2) tissue factor on cells outside the blood that participates in the extrinsic pathway (factor VII). • The common pathway (factor X, factor V, prothrombin, and fibrinogen) is shared by both systems.• Although both pathways provide the opportunity to acquire meaningful information about clotting proteins using the partial thromboplastin time and the prothrombin time, • it is most likely that the physiologically important pathway of blood coagulation is the extrinsic pathway initiated by tissue factor. • fribrin clot formation: last phase of blood clotting. Fribrinogen is an inactive protein made in liver; activated enzyme thrombin removes the end portions of fibrinogen – converting it to active fibrin that can link together to form fibrin threads making a meshlike base t form a blood clot • after fibrin mesh is formed – clotting factor XIII tightens up the mesh, making it more dense and stable – more plts stick to the threads of the mesh and attract other blood cells and proteins to from an actual blood clot. End result: formation of a fibrin clot and local blood clotting (coagulation) Drugs: Hydroxyurea, Mannitol: Ferrous Sulfate: o 30% elemental iron o antanemics; iron supplements; resolution or prevention of iron deficiency anemia. o An essential mineral found in hemoglobin, myoglobin, and many enzymes. o Enters the bloodstream and is transported to the organs of the reticuloendothelial system (liver, spleen, bone marrow) where it becomes part of iron stores. o Common symptoms: nausea, constipation, dark stools, epigastric pain o Oral preparations are most effectively absorbed if administered 1 hr before or 2 hr after meals – Take tablets and capsules with a full glass of water or juice. Do not crush or chew entericcoated tablets and do not open capsules. Liquid preparations may stain teeth. Dilute in water or fruit juice and administer with a straw or place drops at back of throat. B-12: Intrinsic factor is secreted by the gastric mucosa. It binds to B12 and takes it to the Ileum where B12 is normally absorbed into the body for use. folic acid: o Required for protein synthesis and red blood cell function. Stimulates the production of red blood cells, white blood cells, and platelets. Necessary for normal fetal development o Restoration and maintenance of normal hematopoiesis. Oprelvakin (neumenga): o interleukins, thrombopoietic growth factors – colony-stimulating factors o Stimulates production of megakaryocytes and platelets; increased platelet counto Prevention of severe thrombocytopenia and reduction of the need for platelet transfusions following myelosuppressive chemotherapy in patients with nonmyeloid malignancies at risk for thrombocytopenia. o SIDE EFFECTS: HA, dizziness, weakness, conjunctival hemorrhage, atrial fibrillation, dyspnea, edema, palpitations, vasodilation, ventricular arrhythmias, rash, chills, fever, bone pain o Therapy is continued until postnadir platelet count is ≥50,000 cells/mL. Rivaroxaban: o antithrombotics, factor xa inhibitors – anticoagulants o Acts as selective factor X inhibitor that blocks the active site of factor Xa, inactivating the cascade of coagulation; Treatment and prevention of thromboembolic events. Clopidogrel: o plavix; antiplatelet drug o interferes with platelet function; aggregation inhibitors ASA: o salicylates o Decreases platelet aggregation (for this purpose of the test); Decreased incidence of transient ischemic attacks and MI. Heparin: o inhibit clotting factors IIa (thrombin) and Xa o protamine sulfate – heparin antagonist; reversal drugs Coumadin: o inhibt vitamin K – dependent clotting factors II, VII, IX, and X o vitamin k – warfarin antagonist; reversal drugs Enoxaparin: o LMWH; also inhibits clotting factors IIa (thrombin) and Xa Alteplase: (what does this drug do to plasminogen and plasmin and what does that mean for a clot) o activase; tissue plasminogen activators; thrombolytics (dissolves thrombi); lyse a performed clot o Alteplase is most effective when given within 4.5 hours after the onset of manifestations of a stroke.o Alteplase the only fibrinolytic in use for acute ischemic stroke is contraindicated for which patients? Greater than 80 yo Anticoagulation with an INR less than or equal to 1.7 Baseline National Institutes of Health (NIH) stroke scale score greater than 25 H/O both stroke and Diabetes What are the warning signs that thrombolytic therapy is causing intracerebral hemorrhage? What does intrinsic Pathway do? a. All the components necessary for the clotting process to proceed are found in the blood. a. the proteins required for such clotting to take place are part of the intrinsic pathway of blood coagulation. b. This pathway involves a series of proteins, protein cofactors, and enzymes, which interact in reactions that take place on membrane surfaces. c. These reactions are initiated by tissue injury and result in the formation of a fibrin clot d. intrinsic pathway is initiated by the activation of factor XII a. the enzyme form of factor XII (factor XIIa) catalyzes the conversion of factor XI to its enzyme form (factor XIa). b. Factor XIa catalyzes the conversion of factor IX to the activated form, factor IXa, in a reaction that requires calcium ions. c. Factor IXa assembles on the surface of membranes in complex with factor VIII; i. the factor IXa–factor VIII complex requires calcium to stabilize certain structures on these proteins associated with their membrane-binding properties d. Factor X binds to the factor IXa–factor VIII complex and is activated to factor Xa. e. Factor Xa forms a complex with factor V on membrane surfaces in a reaction that also requires calcium ions. f. Prothrombin binds to the factor Xa–factor V complex and is converted to thrombin, a potent enzyme that cleaves fibrinogen to fibrin g. The monomer fibrin molecules then link together (polymerize) to form long fibres i. additional bonding between the units of the polymer is promoted by an enzyme known as factor XIIIa, which stabilizes the newly formed clot by cross-linkages ii. the formation of a fibrin clot What is the extrinsic pathway?a. The protein on the surface of cells that is responsible for the initiation of blood clotting is known as tissue factor or tissue thromboplastin. a. Tissue factor is found in many of the cells of the body but is particularly abundant in those of the brain, lungs, and placenta. b. The pathway of blood coagulation activated by tissue factor, a protein extrinsic to blood, is known as the extrinsic pathway!!! c. Tissue factor serves as a cofactor with factor VII to facilitate the activation of factor X d. Once activated, factor X proceeds to activate prothrombin to thrombin in a reaction requiring factor V. e. The thrombin converts fibrinogen to fibrin. a. **With the exception of factor VII, all components of the extrinsic pathway are also components of the intrinsic pathway What is Disseminated Intracoagulation? Disseminated intravascular coagulation (DIC) is characterized by systemic activation of blood coagulation o which results in generation and deposition of fibrin o leading to microvascular thrombi in various organs and contributing to multiple organ dysfunction syndrome (MODS). Consumption of clotting factors and platelets in DIC can result in life-threatening hemorrhage. Derangement of the fibrinolytic system further contributes to intravascular clot formation, but in some cases, accelerated fibrinolysis may cause severe bleeding. o Hence, a patient with DIC can present with a simultaneously occurring thrombotic and bleeding problem, which obviously complicates the proper treatment. DIC is not itself a specific illness; rather, it is a complication or an effect of the progression of other illnesses. o It is always secondary to an underlying disorder and is associated with a number of clinical conditions, generally involving activation of systemic inflammation. o Such conditions include the following: (NOT A COMPLETE LIST MOST COMMON IS SEPSIS) i. Sepsis and severe infection ii. Trauma (neurotrauma) iii. Organ destruction (eg, pancreatitis) iv. Malignancy (solid and lymphoproliferative/myeloproliferative malignancies) v. Severe transfusion reactionsvi. Obstetric complications – Amniotic fluid embolism; abruptio placentae; hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome; eclampsia vii. Retained dead fetus syndrome viii. Vascular abnormalities - Kasabach-Merritt syndrome and large vascular aneurysms ix. Severe hepatic failure x. Severe toxic reactions - Envenomations, transfusion reactions, and transplant rejection xi. Heat stroke and hyperthermia 6. DIC is most commonly observed in severe sepsis and septic shock. a. Indeed, the development and severity of DIC correlate with mortality in severe sepsis. b. Although bacteremia, including both gram-positive and gram-negative organisms, is most commonly associated with DIC, other organisms (eg, viruses, fungi, and parasites) may also cause DIC. 7. Trauma, especially neurotrauma, is also frequently associated with DIC. a. DIC is more frequently observed in trauma patients with the systemic inflammatory response syndrome (SIRS). b. Evidence indicates that inflammatory cytokines play a central role in DIC in both trauma patients and septic patients. c. In fact, the systemic cytokine profiles in septic patients and trauma patients are nearly identical. 8. The symptoms of DIC are often those of the underlying inciting condition. a. In addition, symptoms of thrombosis, embolism, organ dysfunction, or bleeding may be present. 9. DIC exists in both acute and chronic forms. a. DIC can be acute or chronic. b. Acute DIC develops when sudden exposure of blood to procoagulants (eg, tissue factor [TF], or tissue thromboplastin) generates intravascular coagulation. i. Compensatory hemostatic mechanisms are quickly overwhelmed, and, as a consequence, a severe consumptive coagulopathy leading to hemorrhage develops. ii. Abnormalities of blood coagulation parameters are readily identified, and organ failure frequently results. c. In contrast, chronic DIC reflects a compensated state that develops when blood is continuously or intermittently exposed to small amounts of TF. i. Compensatory mechanisms in the liver and bone marrow are not overwhelmed, and there may be little obvious clinical or laboratory indication of the presence of DIC. ii. Chronic DIC is more frequently observed in patients with solid tumors and in those with large aortic aneurysms.Why must we have adequate iron levels be present in order for erythropoietin to work for anemia? a. Interaction of iron and erythropoietin: b. Erythropoiesis involves the close interaction of iron and erythropoietin. a. In essence, erythropoietin is the accelerator that drives erythropoiesis. b. Iron is the fuel for the production of new red blood cells. c. When the two are coupled, red cell production moves briskly and efficiently. d. If one component is absent (e.g., iron deficiency) anemia results. Food sources of Iron, B-12 and Folic acid Iron: red meat, organ meat, egg yolks, kidney beans, leafy green vegetables, and raisins; Vitamin C helps iron more readily absorb. B-12: found almost exclusively in foods derived from animals – milk, eggs, organ meats like liver, OJ, spinach, dried beans, leafy green veggies, nuts and brewer’s yeast, tofu, fortified cereal, red meat eggs and swiss cheese Folic acid: Foods high in folic acid include vegetables, fruits, and organ meats; heat destroys folic acid in foods – Liver, Organ Meats, Eggs, Cabbage, Broccoli, Brussels sprouts, leafy green veggies, nuts and yeast Labs to know: • CBC – complete blood count – RBC: 4.2-5.4F; 4.7-6.1M; WBC: 5000-10000 • elevated RBC: polcythemia vera, severe dehydration • decreased RBC: anemia, hemorrhage, kidney disease • elevated WBC: infection, inflammation • decreased WBC: immunosuppression, autoimmune disease • Hgb: 12-16,F 14-18, M • Hct: 27-47%,F 42-52%,M • platelets: 150,000-400,000 • MCV – 80-95 • elevated: macrocytic (large) RBCs, megaloblastic anemia • decreased: microcytic (small) RBCs, iron deficiency anemia • MCH – 27-31 • elevated/decreased: same as above for MCV • MCHC• D-dimer & Fibrin Split products (tell you the same thing) – less than 0.4 mcg/ml • positive result: disseminated intravascular coagulation, malignancy • negative: can rule out PE or DVT • Folic acid – • B-12 – • Schillings test – measures presence of B12 in unire after drinking radio active B12 • Reticulocyte count – • Pt/InR • Pt: 11-12.5 seconds • increased: clotting factors II, V, VII, or X, liver disease, warfarin therapy, DIC • decreased: vitamin K excess, PE, thrombophlebitis • INR: 0.8-1.1 (2-3 if on warfarin) • increased: warfarin therapy • decreased: cancer disorders • PTT – 30-40 seconds (1.5-2.5 the control value if heparin therapy is in use) • increased: vitamin K deficiency, DIC, liver disease, heparin administration • decreased: extensive cancer • Coombs test – (used for blood typing) use direct Coombs; confirms autoiummune hemolytic anemia; can be indirect or direct • Ferritin – 12-300ng/mL • Fibrinogen: 200-400mg/dL • TIBC – 250-460 • elevated: iron deficiency anemia, polycythemia anemia • decreased: malnutrition, cirrhosis, pernicious anemia • Serum Iron – 60-160,F – 80-180,M • elevated: hemochromatosis, iron excess, liver disorder, lead tox • decreased: iron deficiency anemia, chronic blood loss, inadequate diet intake of iron What lab can be ordered to monitor enoxaparin therapy? aPTT What clotting factors are Vit K dependent? Dependent clotting factors II, VII, IX, X Know basic pathophysiology, key assessment features, key diagnostics and nursing care & Treatment: Pathophysiological mechanisms of anemia: Major Categories: o Blood loss/destruction, o Nutritional, o Bone Marrow w/suppression failure Increased RBC Loss or Destruction: Blood Loss or Destruction Acute or chronic blood loss (now the difference in assessment findings and diagnostics) o Hemorrhage or Trauma o Chronic GI bleeding, menorrhagia o acute: Loss of significant amount of blood that will trigger compensatory mechanism such as vaso-contriction of peripheral blood vessels and vessels also constrict in the in the liver to increase circulating volume (remember the liver store blood just like the spleen). The heart rate will increase to maintain cardiac output. Fluid shift from the interstial spaces to the vascular space. This all will result in increased volume to compensate for acute blood loss, reducing the viscosity of the blood. However, if the hemorrhage continues theses mechanisms become less effective and Hypovolemic shock may occur. initial manifestation of hypovolemic shock-increasing tachycardia, tachypnea, skin pale, cool, clammy as vessels constrict to maintain blood flow to the brain and heart If the patient continues to lose blood hypotension, decreased LOC and oliguria develop When blood loss is acute and significant the RBC’s are normal shape and size (normocytic) Early on the RBC count and H&H may be normal. As the blood loss continues these will drop. (Iron is lost but when bleeding is stooped the Iron levels return to normal over a period of around 4 weeks) o chronic: Blood loss is slow and chronic, similar to above there is a Shift from interstitial to vascular to prevent hypovolemia. Heart murmurs may develop due to decreased viscosity of the blood. Chronic blood loss depletes iron stores and the as the Bone marrow attempt to correct this over time the blood cells become Small & Pale (microcytic and hypochromic) Increased hemolysis (hemolytic anemias)o Hereditary cell membrane disorders o Defective hemoglobin (sickle cell and thalassemia) Sickle Cell Characterized by replacement of normal hemoglobin with hemoglobin S (HbS). Therefore subject to sickle cell crisis - Increased RBC Destruction “Sickle Cell Crisis”-(vaso-occlusive crisis) o painful episodes that are the result of vascular occlusion. o Crisis can be related to infection, dehydration, trauma, 50% of cases of sickle cell crisis the cause is unknown. Autosomal recessive inheritance of two defective gene alleles for hemoglobin synthesis. o When RBC’s that contain HbS hemoglobin pass through blood vessels the deoxygenation of HbS causes the RBC’s to become rigid and deformed. Causes cells to become a sickle shape. Become rigid and clump together causing the RBC’s to become sticky & fragile. ―Sickled‖ RBC’s occlude blood vessels, especially capillaries. Vascular occlusion causes tissue ischemia and organ damage. Repeated or prolonged ischemia cause damage to tissue and organs Sickling is triggered by any condition the increases the bodies oxygen demand (fever,emotional or physical stress, high altitudes, poorly pressurized airplanes, hypoventilation, vasocontriction due to cold temperatures, acidosis). ―Sickled cells‖ can resume normal shape after re-hydration and reoxygenation. o HOWEVER, Repeated sickling episodes weaken RBC’s cell membranes and shorten the lifespan of affected RBC’s. o Early destruction of RBC’s can lead to anemia. o With repeated episodes of sickling the patient does not―bounce back‖ and when the RBC’s are being destroyed the bone marrow spaces enlarge to produce more RBC’s. 1.Vaso-occlusion- stasis of blood and clumping of sickled cells causing infarction or thrombosis 2.Splenic sequestration-pooling of blood in spleen due to sickled cells occluding drainage. Life threatening. Look for signs of hypovolemia, profound anemia, and shock. 3.Aplastic Crisis-diminished RBC production and increased destruction of RBC’s. signs include profound anemia, pallor, fatigue 4.Acute chest syndrome-pulmonary infiltrates leads to lower respiratory tract symptoms. s/s include fever, cough, chest and back pain, dyspnea, and hypoxemia.Pulmonary infection, infarction, and fat embolism may occur and can lead to pulmonary failure or death. Treatment includes: Analgesics (dilaudid,morphine) OTC or with a PCA – never PRN, IV fluid replacement, Blood tranfusions, Oxygen, Hydroxyurea Yearly flu and pneumonia vaccine, Increase hydration, Avoid taking blood pressure with external cuff. Do not raise the knee position of the bed, Elevate the head of the bed no more than 30 degrees, Keep room temperature at or above 72°, Encourage the patient to keep extremities extended to promote venous return. Bone marrow transplant Thalassemia Group of hereditary disorders associated with defective hemoglobin chain synthesis two types: o Alpha (microytic) stillborn bone deformities of face growth failure o Beta (can be fatal) Characterized by Hypochromia (abnormal decrease in the Hgb of RBC’s) and extreme microcytosis (smaller than normal RBC’s) and destruction of blood. o Fragile Hypochromic, microcytic RBC’s called ―Target Cells‖ because of their distinctive bull’s eye appearance. You will see bone marrow hyperplasia, decreased H&H, and decreased Retic count ANEMIA mild to severe, fatigue, weakness, sob, pallor, Delayed growth, facial deformities, CHF, osteoporosis, splenomegaly (increased RBC’s production due to hemolysis), Hepatomegaly & jaundice (due to hemolysis),Bronze skin coloring, Fractures of long bones, ribs, vertebrae are the result of bone marrow expansion and thinning as a result of increased hematopoiesis. NO CURE – only treatment; folic acid o diet should be low iron intake; avoid d meat, pork, poultry, seafood, raisins, beans, dark green leafy veggies, and iron fortified cereals encourage low contact sports – swimming or walking o G6DP deficiency Hereditary defect in RBC metabolism. X-linked recessive deficiency of the enzyme G6PD Hereditary condition in which RBCs break down when body is exposed to certain drugs/stress of infection G6DP also impairs the necessary compensatory increase in glucose metabolism and causes cellular damage. The defective G6DP enzyme wrongly oxidizes hemoglobin, damaging the RBC in the process. Hemolysis occurs when the patient with the damaged RBC’s is exposed to ASA, sulfonamides, or vitamin K derivatives, stressors that increase the metabolic demands of the RBC’s. exposed to a stressor that triggers G6DP anemia symptoms develop over several days. o Pallor, Jaundice, hemaglobinuria (hemoglobin in the urine). o During this acute phase, anemia and jaundice develop. Osmotic diuretics, such as mannitol (Osmitrol), may help prevent this complication most important measure is prevention – avoidance of the drugs and foods that cause hemolysis Hydration is important during an episode of hemolysis to prevent debris and hemoglobin from collecting in the kidney tubules which can lead to acute kidney injury (AKI). Anti-oxidants are good for them: berries,walnuts, pomegranate, ginger. Adequate fats & carbs Avoid: Fava beans, legumes, menthol, food coloring, sulfites, vitamin K, ascorbic ac Autoimmune hemolytic Anemiaso Abnormal immune function in which a person's immune reactive cells fail to recognize his or her own red blood cells as self cells occurs when your immune system makes antibodies that attack your red blood cells. This causes a drop in the number of red blood cells, leading to hemolytic anemia o MAY BE CAUSED BY AUTOIMMUNE DISEASES EBV, NHL, HIV, hepatitis o two main types of autoimmune hemolytic anemia: warm antibody anemia occurs with immunoglobulin G (IgG) antibody excess antibodies are most active at 98.6° F (37° C) may be triggered by drugs, chemicals, or other autoimmune problems cold antibody anemia has complement protein fixation on immunoglobulin M (IgM) occurs most at 86° F (30° C) often occurs with a Raynaud's-like response in which the arteries in the hands and feet constrict profoundly in response to cold temperatures or stress the hands and feet may be cold or bluish. o Coombs test is the confirmation of this anemia o Symptoms may include unusual weakness and fatigue with tachycardia and breathing difficulties, jaundice, dark urine and/or splenomegaly o Steroid therapy to suppress immunity is temporarily effective in most patients. Splenectomy and more intense immunosuppressive therapy with chemotherapy drugs may be used if steroid therapy fails Decreased RBC Production Nutritional or Bone Marrow Suppression/Failure Altered DNA synthesis: o B12 malabsorption or deficiency (two types) Called Pernicious Anemia when failure to absorb from GI tract vitamin B12 anemia caused by a deficiency of inadequate gastric intrinsic factor (IF) which is essential for the intestinal absorption of vitamin B12 In pernicious anemia- smooth, beefy red, sore tongue and diahrrea Tx of Pernicious Anemia: with B12 (cyanocobalamin) injections o IM; weekly at first then monthly for the rest of their life o Oral B12 preparations and nasal spray or sublingual forms of cyanocobalamin may be used to maintain vitamin levels after thepatient's deficiency has first been corrected by the traditional injection method. Inadequate consumption/Dietary deficiency inadequate dietary intake of vitamin B12. Strict vegetarians – diets lacking dairy products Vitamin B12 deficiency anemia may be mild or severe, usually develops slowly o Pallor, or slight jaundice, weakness, glossitis, cheilosis, diarrhea. correct diet – milk, eggs, liver, OJ, spinach, dried beans, leafy green veggies, nuts, and brewer’s yeast, schilling test Because B12 is important for neurological functions: paresthesias (numbness & tingling of hands & feet) (most common neuro s/s); ataxia, problems with proprioception, difficulty maintaining balance Vitamin supplements may be prescribed when anemia is severe. o Folic acid malabsorption or deficiency Folic acid is needed for DNA synthesis and RBC maturation Can also cause anemia with manifestations similar to those of vitamin B12 deficiency nervous system functions remain normal because folic acid deficiency does not affect nerve function LACK OF FOLIC ACID LEADS TO DECREASE PRODUCTION OF RBCs RBCs produced are abnormally large (macrocytic) Common causes of folic acid deficiency poor nutrition, malabsorption, and drugs Poor nutrition-a diet lacking green leafy vegetables, liver, yeast, citrus fruits, dried beans, and nuts, is the most common cause Often seen in alcoholics & drug addicts, older adults, patients receiving TPN. ***Also be aware that increased folic acid levels can also cause anemia…. So pregnant women taking folic acid for to prevent neural tube defects of the infant are at risk for anemias due to too much folic acid. Malabsorption of folic acid due to coexisting B12 deficiency (including pernicious anemia) Malabsorption syndromes like Crohn’s disease, Celiac Sprue Drugs that inhibit folic acid metabolism o methotrexate, anticonvulsants, some chemotherapy drugs & oral contraceptives replace dietary folic acid and treat the cause is treatment Altered Hemoglobin Synthesis o Iron Deficiency common anemia worldwide, especially among women of child bearing age, older adults, and people with poor diets problem is a decreased iron supply for the developing RBC Any adult with iron deficiency should be evaluated for abnormal bleeding, especially from the GI tract CAUSES: Nutritional iron deficiency o Inadequate iron intake caused by: Iron-deficient diet -example: vegetarians Chronic alcoholism protein deficient diet. Often seen with Pica (consumption or craving for a non food item) lead poisoning Internal blood loss o chronic o occult (hidden) blood loss peptic ulcers, GI inflammation, hemorrhoids, cancer Impaired absorption o chronic diarrhea o partial or total gastrectomy Increased body demands o Rapid metabolic (anabolic) o Pregnancy & lactation o Adolescence o Infection LABS adults usually have between 2 to 6 g of iron depending on size, amount of Hgb in cells o serum iron level: look at lab values from early o ferritin: <10ng/mL (NORMAL RANGE IS 12-300ng/mL) this is the most accurate test to diagnose iron deficiency anemia!!! RBC, Hgb, MCH, MCV, MCHC are all LOW with iron deficiency anemia!!! o as well as serum ferritin and serum iron TIBC and RDW are elevated!!! signs/symptoms: If have mild symptoms of anemia, including weakness and pallor o make sure your looking at skin and palmar creases Other manifestations include fatigue, reduced exercise tolerance. Chronic Iron deficiency Anemia- brittle spoon shaped nails, cheilosis (cracks in corners of mouth) smooth sore tongue, & Pica’s (eating ice, dirt, clay ect..) can give iron parenterally (in severe cases) oral iron intake from supplements like ferrous sulfate should be taken between meals for better absorption and to reduce GI distress stools may be black or green BEST ABSORBED ON AN EMPTY STOMACH DRINK WITH A STRAW (stains teeth) take with ascorbic acid (vitamin C) to increase absorption Tx: replace Iron; Expect results in 2-4 wks Bone Marrow Supression/Failure: o Aplastic Anemia (stem cell dysfunction) TYPES Faconi’s- defects in DNA repair Acquired Idiopathic- cause unknown stem cell damage after Exposure to o myelotoxic agents: Radiation, Benzene, Chloramphenicol, Alkylating agents, Antimetabolites, Sulfonamides, Insecticides Viral infection cause: o Epstein-Barr virus-mononucleosis, Hepatitis C, HIV Aplastic anemia is a deficiency of circulating red blood cells (RBCs), WBC and platelets (pancytopenia) because of failure of the bone marrow to produce these cells although typically occurs alone can be seen with leukopenia (reduction in WBC), thrombocytopenia (a reduction in platelets), and a condition known as pancytopenia complete blood count (CBC) shows severe macrocytic anemia, leukopenia, and thrombocytopenia. disease onset may be slow or rapid most common type of disease is caused by exposure to toxic agents, drugs ionizing radiation, or infection signs/symptoms patient has manifestations depending on the severity of pancytopenia Faitigue,pallor, weakness, exertional dyspnea, headache tachycardia & heart failure Platelet deficiency leads to bleeding problems, bleeding gums, excessive bruising, nosebleeds maybe initial symptoms A defiency in WBC’s increases the risk for infection, causing manifestations like sore throat and fever. Hematopoietic stem cell transplantation with donor cells is the most successful method of treatment for aplastic anemia that does not respond to other therapies patients who are unable to undergo such treatment or lack a suitable donor, immunosuppressive therapy remains the treatment of choice. Platelets or Clotting factors disorders – ITPo Idiopathic Thrombopenic Purpura o Characterized by autoimmune destruction of platelets. Thrombocytopenia o usually follows a viral infection (chicken pox, rubella or measles) o High risk for spontaneous bleeding if PLT <20,000/ mm3 o s/s petecchia, (pin point hemorrhages, on skin and mucous membranes) purpura (purple discolored areas) most commonly found in mucous membranes anterior thorax and neck Decreased platelet count, platelet antibodies, prolonged bleeding time, Bone marrow will show decreased platelet activity and increased megakaryocytes. o Treatment: Platelet transfusion if bleeding, Steroids and immunoglobulins to suppress immune response, Immunosuppressive therapies also visicristine & cyclophosphamide. Platelet growth factor OPRELVEKIN. Spleenectomy if medications are not effective. o Put patient on bleeding precautions; avoid aspirin (other drugs affecting coagulation) TTP o Thrombotic Thrombocytopenic Purpura o Autoimmune Disease where Platelets clump together abnormally in the capillaries and leave very few circulating platelets and inappropriate clumps of platelets elsewhere in the circulation o TX: FFP (fresh frozen plasma), Plasma exchange, immunosuppressants, ASPIRIN Hemophilia A & B o Hemophilia is a hereditary bleeding disorder with two forms resulting from different clotting factor deficiencies o Hemophilia A (classic hemophilia) is a deficiency of factor VIII and accounts for 80% of cases of hemophilia affects mostly males, none of whose sons will have the gene for hemophilia and all of whose daughters will be carriers A: managed by either regularly scheduled infusions of synthetic factor VIII or the infusion of this substance only when injury or bleeding occurs o Hemophilia B (Christmas disease) is a deficiency of factor IX and accounts for 20% of cases. o Von Willebrands – did not talk about much in class* – it is one of the common disorders that result from defects at the clotting factor level along with hemophilias A and B!! o Most clotting factor disorders are genetic problems of one clotting factor. A damaged liver also leads to a clotting disorder by reducing the amount of clotting factors produced.o Hemophilia is an X-linked recessive trait meaning women are carriers (daughters are carriers and if passes to son they have hemophilia) o patient with hemophilia show a prolonged activated partial thromboplastin time (aPTT), a normal bleeding time, and a normal prothrombin time (PT). o Signs and symptoms for both A and B are identical the patient has abnormal bleeding in response to any trauma because of a deficiency of the specific clotting factor Hemophiliacs form platelet plugs at the bleeding site, but the clotting factor deficiency impairs the formation of stable fibrin clots. This allows excessive bleeding, which may be mild, moderate, or severe, depending on the degree of factor deficiency. Excessive bleeding from minor cuts, bruises, or abrasions (from abnormal platelet function) Joint and muscle hemorrhages that lead to disabling long-term problems and may require joint replacement The most common problem that occurs with hemophilia is degenerating joint function as a result of chronic bleeding into the joints, especially the hip and knee. HIT o heparin induced thrombocytopenia a serious immunity-mediated clotting disorder with an unexplained drop in platelet count after heparin treatment. o occurrence is increasing because of the increased use of heparin o HIT is an immune-mediated drug reaction that is caused by heparin-dependent plateletactivating immunoglobulin G (IgG) antibodies in which heparin binds with platelet factor 4 (PF4) drug binding leads to the development of a highly reactive immune complex that activates the platelets. Once activated, platelets release procoagulants and PF4, which neutralizes heparin and increases thrombin generation from prothrombin o risk factors duration of heparin longer than 1 week exposure to unfractionated heparin post-surgical trhomboprophylaxis being female o LOW platelet count but not symptomatic o S/S: venous thromboembolism (VTE) such as deep vein thrombosis and pulmonary embolism thrombocytopenia after heparin exposure is THE HALLMARK SIGN of HIT "systemic reaction") may occur when the infusion is started. These include fever, chills, high blood pressure, a fast heart rate, shortness of breath, and chest pain. This happens in about a quarter of people with HIT most common symptom of HIT is enlargement or extension of a previously diagnosed blood clot, or the development of a new blood clot elsewhere in the body may take the form of clots in either arteries or veins o arterial thrombosis: stroke, MI, acute leg ischemia o venous thrombosis: DVT in leg/arm, PE o tx: includes anticoagulant therapy use a direct thrombin inhibitor such as argatroban or angiomax do not use warfarin – can cause warfarin necrosis an alternative anticoag is used and it cant be warfarin until platelet count is at a certain range do not give platelets either Overproduction of RBC’s – Polycythemia vera 2 types: o Cancer o Excessive erythropoiesis as a physiological response to hypoxia (prolonged exposure to high altitudes, pulmonary disease, hypoventilation, smoking) number of red blood cells (RBCs) in the blood is greater than normal o blood of a patient with polycythemia is hyperviscous (thicker than normal blood) PV is a cancer of the RBCs with three major hallmarks: o massive production of RBCs, excessive leukocyte production, and excessive production of platelets o Many of these of patients show a mutation of the JAK2 kinase gene in the affected cells o Extreme hypercellularity (cell excess) of the peripheral blood occurs in people with PV. Even though the number of RBCs is greatly increased, o their oxygen-carrying capacity is impaired o patients have poor gas exchange with severe hypoxia. Bleeding problems are common because of platelet impairment. LABS: o Hgb levels: sustained increase to 18g/dL o RBC count of 6 million/mm3 o Hct of 55% or greater S/S o Plethoric (dark, facial appearance from the blood is so oxygenated) facial skin and mucous membranes o Intense itching caused by dilated blood vessels, and poor perfusion is common o thick blood moves more slowly and places increased demands on the heart resulting in hypertension o Breathing difficulty when lying down o Dizziness o Excessive bleeding o Fullness in the left upper abdomen (due to enlarged spleen) o Headache o Itchiness, especially after a warm bath o Red coloring, especially of the face o Shortness of breatho Symptoms of phlebitis TREATMENT: repeated phlebotomy with apheresis (2 to 5 times per week), the patient may live 10 to 15 years or longer o Apheresis is the withdrawal of whole blood and removal of some of the patient's blood component, in this case RBCs. o The plasma is then reinfused back into the patient. o Drink at least 3 liters of liquids each day. o Avoid tight or constrictive clothing, especially garters and girdles. o Wear gloves when outdoors in temperatures lower than 50° F (10° C). Emergency Preparedness: Types of disasters internal any event inside a health care facility or campus that could endanger the SAFETY of patients or staff fire, explosion, loss of critical utilities (e.g., electricity, water, and communications capabilities), and violence event creates a need for evacuation or relocation. It often requires extra personnel and the activation of the facility's emergency preparedness and response plan most important outcome for any internal disaster is to maintain patient, staff, and visitor safety. external any event outside the health care facility or campus, somewhere in the community, which requires the activation of the facility's emergency management plan can be either natural, such as a hurricane, earthquake or tornado or technologic, such as an act of terrorism with explosive devices or a malfunction of a nuclear reactor with radiation exposure. The number of facility staff and resources may not be adequate for the incoming emergency department (ED) patients Both internal and external disasters can result in many casualties, including death. ** Multi-casualty and mass casualty (disaster) events are not the same main difference between the two is based on the scope and scale of the incident, considering the number and severity of victims or casualties involved Both require specific response plans to activate necessary resources a multi-casualty event can be managed by a hospital using local resources a mass casualty event overwhelms local medical capabilities and may require the COLLABORATION of multiple agencies and health care facilities Nurse role in a fire within a medical facility – remember RACE (rescue, alarm, confine, extinguish) Remove any patient or staff from immediate danger of the fire or smoke. Discontinue oxygen for all patients who can breathe without it. For patients on life support, maintain their respiratory status manually until removed from the fire area. Direct ambulatory patients to walk to a safe location. If possible, ask ambulatory patients to help push wheelchair patients out of danger. Move bedridden patients from the fire area in bed, by stretcher, or in a wheelchair; if needed, have one or two staff members move patients on blankets or carry them. After everyone is out of danger, seek to contain the fire by closing doors and windows and using an ABC extinguisher (can put out any type of fire), if possible. Do not risk injury to you or staff members while moving patients or attempting to extinguish the fire. Mass casualty triage: what are the meanings A key process in any multi-casualty or mass casualty response is effective triage to rapidly sort ill or injured patients into priority categories based on their acuity and survival potential. Most mass casualty response teams both in the field (at the disaster site) and in the hospital setting use a disaster triage tag system that categorizes triage priority by color and number: red Emergent (class I) patients airway obstruction or shock, and require immediate attention yellow Patients who can wait a short time for care (class II) major injuries, such as open fractures with a distal pulse and large wounds that need treatment within 30 minutes to 2 hours green Nonurgent or ―walking wounded‖ (class III) patient minor injuries that can be managed in a delayed fashion, generally more than 2 hours closed fractures, sprains, strains, abrasions, and contusions black tag Patients who are expected to die or are dead are issued a black tag massive head trauma, extensive full-thickness body burns, and high cervical spinal cord injury requiring mechanical ventilation resources must be dedicated to saving the most lives rather than expending valuable resources to save one life at the possible expense of many others What occurs during event resolution and debriefing When the last major casualties have been treated and no more are expected to arrive in numbers that could overwhelm the health care system the incident commander considers ―standing down‖ or deactivating the emergency response plan However, although the casualties may have left the ED, other areas in the hospital may still be under stress and need the support of the supplemental resources provided by emergency plan activation. Before terminating the response, it is essential to ensure that the needs of the other hospital departments have been met and all are in agreement to resume normal operations. Environmental related injuries 1. Heat related illness a. Who is at risk? i. Older adults- Older adults have less body fluid volume and can easily become dehydrated when exposed to excessive heat and humidity. 1. Wearing heavy clothing, inadequate acclimatization to hot weather, and social disadvantage (e.g., poor housing, lack of air-conditioning) ii. People with mental health conditions iii. People who work outside iv. Homeless people v. illicit drug users (especially cocaine users) vi. Outdoor athletesvii. members of the military who are stationed in countries with hot climates viii. Pre-existing health status problem especially obesity, heart disease, fever, infection b. Prevention i. Avoid alcohol and caffeine ii. Prevent overexposure to the sun; use a sunscreen with an SPF of at least 30 with UVA and UVB protection iii. Wear clothing suited to the environment. Lightweight, light-colored, and loose-fitting clothing is best iv. cool baths or showers to help reduce body temperature c. Heat exhaustion i. s/s 1. Usually have flu-like symptoms with headache, weakness, nausea, and/or vomiting. 2. Body temperature is not significantly elevated in this condition. 3. The patient may continue to perspire despite dehydration a. (YOU WILL HAVE HYPONATREMIA CAUSED BY EXCESSIVE SODIUM LOST IN PERSPIRATION) 4. assess for orthostatic hypotension and tachycardia a. especially the older adult who is predisposed to rapid dehydration. b. Older adults who are already dehydrated often experience acute confusion and are at risk for falls. ii. treatment 1. immediately stop physical activity; move him or her to a cool place, and use cooling measures a. cooling measures include: i. placing cold packs on the neck, chest, abdomen, and groin; ii. soaking the person in cool water; iii. or fanning him or her while spraying water on the skin. 2. Remove any constrictive clothing!! 3. Provide an oral re-hydrating solution such as a sports drink or an oral rehydration therapy solution. a. Mistakenly drinking plain water can worsen the sodium deficit!!! (diluting the sodium even further causing to be more hyponatremic)b. do not give salt tabs!! can cause stomach irritation, N/V 4. If these signs and symptoms persist, call an ambulance to transport the patient to the hospital. 5. In clinical setting treatment: a. monitor vital signs. b. Rehydrate the patient with IV 0.9% saline solution if nausea or vomiting persists. c. Draw blood for serum electrolyte analysis. d. Hospital admission is indicated only for patients who have... i. other health problems that are worsened by the heat-related illness ii. or for those with severe dehydration. d. Heat stroke i. types 1. Heat stroke is a true medical emergency in which body temperature may exceed 104° F (40° C). a. The victim's THERMOREGULATION mechanisms fail and do not adjust to the high body temp. b. If the condition is not treated or the patient does not respond to treatment, organ dysfunction and death can result. 2. two major types of heat stroke are exertional and classic a. Exertional heat stroke i. has a sudden onset ii. is often the result of strenuous physical activity in hot, humid conditions. iii. Not being used to hot weather and wearing clothing too heavy for the environment are common contributing factors. b. Classic heat stroke i. also referred to as non-exertional heat stroke ii. occurs over a period of time as a result of chronic exposure to a hot, humid environment 1. such as a home without air-conditioning in the high heat of the summer. ii. s/s1. elevated body temperature (above 104° F [40° C]) 2. skin is hot and dry, the presence of sweating does not rule out heat stroke a. PATIENTS WITH HEAT STROKE MAY CONTINUE TO PERSPIRE 3. Mental status changes occur as a result of thermal injury to the brain a. confusion, bizarre behavior, seizures, or even coma 4. hypotension, tachycardia, and tachypnea 5. Recent research – cardiac troponin I (cTnI) is frequently elevated during nonexertional heat-related illnesses. a. A severe increase (>1.5 ng/mL) indicates severe myocardial damage 6. Complications of THERMOREGULATION failure seen w/heat stroke: a. Multiple organ dysfunction syndrome (MODS), b. renal impairment, c. electrolyte and acid-base disturbances, d. coagulopathy (abnormal clotting), e. pulmonary edema and cerebral edema iii. treatment 1. in the field a. Ensure a patent airway. b. Remove the patient from the hot environment (into air-conditioning or into the shade). c. Remove the patient's clothing. d. Pour or spray cold water on the patient's body and scalp. e. Fan the patient (not only the person providing care, but all surrounding people should fan the patient with newspapers or whatever is available). f. If ice is available, place ice in cloth or bags and position the packs on the patient's scalp, in the groin area, behind the neck, and in the armpits. g. Contact emergency medical services to transport the patient to the emergency department. 2. at the hospital – remember ABC a. Give oxygen by mask or nasal cannula; be prepared for endotracheal intubationb. Start at least one IV with a large-bore needle or cannula. c. Administer normal saline (0.9% sodium chloride) as prescribed, using cooled solutions if available. d. Use a cooling blanket. e. Do not give aspirin or any other antipyretics. f. Insert a rectal probe to measure core body temperature continuously, or use a rectal thermometer and assess temperature every 15 minutes. g. Insert an indwelling urinary drainage catheter. i. Measure urine output and specific gravity to determine fluid needs. ii. Obtain UA h. Monitor vital signs frequently as clinically indicated. i. Obtain baseline laboratory tests as quickly as possible: i. serum electrolytes, cardiac enzymes, liver enzymes, and complete blood count (CBC). j. Assess arterial blood gases. k. Administer muscle relaxants (benzodiazepines) if the patient begins to shiver. i. Give parenterally – drugs include diazepam (valium) or lorazepam (ativan) l. Stop cooling interventions when core body temperature is reduced to 102° F (39° C) 2. Snake bites a. venom causes local and systemic toxic effects. i. The enzymes in venom break down human tissue proteins, alter membrane integrity, and impair blood clotting b. Pit Viper bites i. pit vipers include: 1. rattlesnakes, copperheads, and cottonmouths ii. s/s 1. pit viper envenomation can lead to a. impaired TISSUE INTEGRITY from local tissue necrosis and massive tissue swelling, b. intravascular fluid shifts and hypovolemic shock,c. pulmonary edema, d. renal failure, e. hemorrhagic complications from disseminated intravascular coagulation (DIC), f. death 2. Severe PAIN, swelling, and redness or ecchymosis (bruising) in the area around the bite are common. a. Hours later, vesicles or hemorrhagic bullae may form. 3. Systemic responses to venom must be distinguished from the effects of anxiety and panic related to being bitten by a snake. a. Common reports by the victim include a minty, rubbery, or metallic taste in the mouth b. tingling or paresthesias of the scalp, face, and lips. c. Other effects include muscle fasciculations (twitching) and weakness, nausea, vomiting, hypotension, seizures, and coagulopathy (clotting abnormalities) or DIC iii. treatment 1. in the field a. first priority is to move the person to a safe area away from the snake and encourage rest to decrease venom circulation b. remove jewelry and constricting clothing before swelling worsens c. Call for immediate emergency assistance. Do not attempt to capture or kill the snake, but do take digital photographs to identify at hospital d. immobilizing the affected extremity in a position of function with a splint may help limit the spread of the venom i. Maintain the extremity at the level of the heart. ii. Keep the person warm, and provide calm reassurance. iii. Do not offer any alcohol because it can cause the venom to spread through vasodilation iv. Do not incise or suck the wound, apply ice to it, or use a tourniquet 1. these actions are ineffective and can worsen the patient's outcome 2. hospital care a. Supportive care includesi. supplemental oxygen, ii. two large-bore IV lines, iii. and infusion of crystalloid fluids 1. such as normal saline solution or Ringer's lactate solution b. Apply continuous cardiac and blood pressure monitoring equipment to quickly detect clinical deterioration c. Provide tetanus prophylaxis and wound care as part of the collaborative plan of care. – can also give pain meds such as opioids d. obtain labs: coagulation profile, complete blood count (CBC), creatine kinase (CK), type and crossmatch for possible blood transfusion, and urinalysis 3. Cro Fab a. ***Not all snakebite victims need antivenom administration i. Contact the regional poison control center so that toxicologists can provide specific advice for antivenom dosing and medical management b. Crotalidae Polyvalent Immune Fab i. derived from sheep (ovine) 1. this drug consists of specific antibody fragments of immunoglobulin G (IgG) that bind and neutralize toxins in pit viper venom to counteract its effects on the body c. unlike the older antivenoms that were derived from horse serum, serum sickness rarely occurs after IV CroFab administration. i. Serum sickness is a type III hypersensitivity reaction that develops within 3 to 21 days 1. first as a skin rash with progression to fever, joint PAIN, and pruritus (itching). d. Drug effects: i. Although mild to moderate allergic reactions such as pruritus and urticaria (hives) can occur, anaphylaxis is rare. ii. Allergry to pineapple or papaya: 1. CroFab is contraindicated unless the benefits are believed to outweigh the risks.iii. Give CroFab cautiously to patients who have: previous allergy, bromelain allergy (pineapple-derived enzyme) or sheep protein, pregnancy, prior crofab therapy, sensitivity to mercury products e. CroFab should be given with the optimal timing within 6 hours of the bite f. The recommended initial IV dose is 4 to 6 vials infused over 60 minutes. i. If symptoms are not effectively controlled with the first dose, an additional 4 to 6 vials are recommended. ii. Once the symptoms are under control, 2 more vials of CroFab are administered every 6 hours for a total of 18 hours of administration c. Coral Snakes i. s/s 1. result of its neurotoxic properties a. physiologic effect is to block neurotransmission causing the following: i. weakness, ii. cranial nerve deficits (ptosis, diplopia, swallowing difficulty), iii. an altered level of consciousness, iv. and, ultimately, respiratory paralysis b. venom is spread via the lymphatic system, but swelling, if present, is typically mild – usually mild and transient pain c. toxic effects may be delayed up to 13 hours after a bite but then produce rapid clinical deterioration i. Early signs and symptoms include nausea, vomiting, headache, pallor, and abdominal pain. ii. Assess for neurologic manifestations, such as paresthesias (painful tingling), numbness, muscle fasciculations, and mental status changes, as well as cranial nerve and peripheral nerve deficits. iii. Total flaccid paralysis may occur later, and the patient may have difficulty speaking, swallowing, and breathing. iv. Clotting disorders do not occur. ii. treatment 1. in the fielda. identify the snake as a coral snake – if can not identify treat as if it is venomous snake b. field tx to limit the spread of venom includes the use of pressure immobilization techniques i. affected extremity is encircled snugly with an elastic bandage or roller gauze dressing to impede lymphatic flow; it is then splinted. ii. Leave this on even if being transported to medical facility 2. hospital care a. patients who have had an actual or potential coral snake envenomation will have continuous cardiac, blood pressure, and pulse oximetry monitoring and are admitted to a critical care unit b. Prepare to provide aggressive airway management via endotracheal intubation if respiratory insufficiency or severe neurologic impairment occurs c. patient can survive a coral snake bite without antivenom i. but may require prolonged mechanical ventilation; ii. the effects of severe bites can persist for many days d. The most significant risk to the victim is airway compromise and respiratory failure. i. ensure that the patient's IV lines are patent and that resuscitation equipment is immediately available. 3. Arthropod Bites a. Brown recluse i. loxoscelism 1. since most do not see spider that bit them, only evidence may be impaired TISSUE INTEGRITY from a skin lesion or a necrotic wound 2. or, less often, systemic effects from the injected toxin, commonly referred to as loxoscelism. a. systemic toxicity to brown recluse spider bites b. These can include a rash, fever, chills, nausea, vomiting, malaise, and joint PAIN. c. In the worst cases, hemolytic reactions, thrombocytopenia, renal failure, pulmonary edema, cardiovascular collapse, and death can occur. ii. s/s 1. bite may be described as painless or stinging to sharp and painfula. Some victims are unaware that they were bitten until intense local aching and pruritus develop over minutes to hours 2. TISSUE INTEGRITY a. appearing as a bleb or vesicle surrounded by edema and erythema, b. which may expand over the course of hours as the toxin spreads to surrounding tissues c. center of the bite becomes bluish purple d. over the next 1 to 3 days the central part of the wound becomes dark and necrotic e. Eschar (a necrotic, leathery covering over the wound) eventually forms i. combination of tissue changes known as “red, white, and blue sign” iii. treatment 1. in the field a. first aid – apply cold compresses over the site intermittently until there is no further progression of the wound i. Cold helps decrease the enzyme activity of the venom and may limit tissue swelling and necrosis ii. Do not use heat because it increases the enzyme activity and potentially worsens the wound b. elevation of the affected extremity, local wound care, and rest. 2. hospital care a. Supportive care and ongoing monitoring for complications meet the needs of most patients with a brown recluse spider bite. b. For patients with wounds that appear infected: i. topical antiseptic and sterile dressings are necessary. ii. Wound cultures and antibiotics may also be indicated. iii. Tetanus prophylaxis is recommended. c. A surgeon evaluates patients whose wounds require interventions beyond conservative management i. Débridement (removal of necrotic tissue) and skin grafting may be required1. promotes TISSUE INTEGRITY and healing in severe wounds. d. If loxoscelism s/s show: i. aggressive hydration, blood transfusions, hemodialysis, and supportive therapies b. Black widow c. Lactrodectism i. Black widow spider venom produces a syndrome known as latrodectism, in which the venom causes neurotransmitter release from nerve terminals. ii. s/s 1. Severe abdominal PAIN, muscle rigidity and spasm, hypertension, and nausea and vomiting are common 2. Muscle spasms involve the large muscles of the abdomen, back, and limbs. 3. facial edema, ptosis (eyelid drooping), diaphoresis, weakness, increased salivation, respiratory difficulty from excessive secretions, fasciculations (twitching), and paresthesias (painful tingling or numbness). iii. treatment 1. In the field a. priority intervention – apply an ice pack because cold application decreases the action of the neurotoxin b. Monitor the person for evidence of systemic toxicity i. If this problem occurs, support the patient's airway, breathing, and circulation. 2. hospital care a. closely monitor vital signs, with special attention to blood pressure and respiratory function. b. Supportive therapy i. opioid pain medication and muscle relaxants such as diazepam (Valium) or other benzodiazepines. ii. Provide tetanus prophylaxis as needed. iii. Observe the patient for seizures related to a rapidly rising blood pressure. iv. For some patients, antihypertensive agents are needed. c. Less often, i. pulmonary edema, uncontrollable hypertension, seizures, respiratory arrest, and shock occur. ii. These patients require critical care management.iii. Antivenom is available for black widow spider bites. 1. Although it can cause anaphylaxis and serum sickness, antivenom is considered effective in treating severe reactions. 2. The drug is also given to pregnant women because they may have uterine contractions from a black widow spider bite that can lead to a premature delivery. 4. Bee and wasp bites a. s/s i. first has a local reaction of immediate PAIN and a wheal-and-flare skin reaction. ii. For some people, swelling can be extensive and involve an entire limb or body area. iii. Systemic effects can then develop based on the venom load and the person's sensitivity to the venom. 1. These effects may include generalized edema, nausea, vomiting, and diarrhea and are reactions to the toxic effects of the venom itself, not necessarily an allergic reaction. 2. Other toxic venom effects include destruction of red and white blood cells and platelets, damage to the blood vessel walls, acute kidney injury, renal failure, liver injury, and cardiac complications; multi-system organ failure can develop iv. If the patient has an allergy to the venom, 1. urticaria (hives), pruritus (itching), and swelling of the lips and tongue may occur. 2. An allergic response can rapidly progress to an anaphylactic reaction in highly sensitive patients. 3. Anaphylaxis is a life-threatening allergic response and is evidenced by respiratory distress with bronchospasm and laryngeal edema, hypotension, deterioration in mental status, and cardiac dysrhythmias. b. Treatments i. Basic emergency care for bee and wasp stings includes quick removal of the stinger (if present) and application of an ice pack ii. If the patient has a severe allergic reaction with wheezing, facial swelling, and respiratory distress, epinephrine must be given immediately 1. allergy – hospital admission a. patients who sustain serious reactions to bee or wasp stings need oxygen administration and continuous cardiac and blood pressure monitoring. b. Establish an IV infusion with normal saline solution to support blood pressure.c. Advanced life support drugs and resuscitation equipment should be made immediately available. d. If epinephrine IM fails to relieve the life-threatening reaction, a different epinephrine formulation may be requested as a very slow IV bolus. 5. lightening injuries a. assessment – S/S i. Both the cardiopulmonary and the central nervous systems are profoundly affected by lightning injuries. ii. People who survive the immediate lightning strike may be treated in a less emergent fashion. 1. these victims can have serious myocardial injury, which may be manifested by ECG and myocardial perfusion abnormalities, such as angina and dysrhythmias. 2. The initial appearance of mottled skin and decreased to absent peripheral pulses usually arises from arterial vasospasm and typically resolves spontaneously in several hours. iii. CNS findings: 1. classic finding is an immediate but temporary paralysis that affects the lower limbs to a greater extent than the upper limbs. b. treatment i. in the field 1. initial care includes spinal immobilization with priority attention to stabilization of airway, breathing, and circulation through standard basic and advanced life support measures. 2. CPR is performed immediately when a person is in cardiac arrest. 3. If cardiopulmonary or CNS injury is present, skin burns are not an initial priority! a. However, if time and resources permit, a sterile dressing may be applied to cover the sites. 4. Victims of lightning strike are not electrically charged; the rescuer is in no danger from physical contact. ii. hospital care 1. Once in the acute care hospital setting, a. the focus of care is advanced life support management, including cardiac monitoring to detect cardiac dysrhythmias and a 12-lead ECG.2. The patient may require mechanical ventilation until spontaneous breathing returns. 3. A computed tomography (CT) scan of the head may be performed to identify intracranial hemorrhage. 4. A creatine kinase (CK) measurement may be requested to detect skeletal muscle damage resulting from the lightning strike. 5. In severe cases, rhabdomyolysis (circulation of by-products of skeletal muscle destruction) can lead to renal failure. 6. Burn wounds are assessed and treated according to standard burn care protocols. a. Tetanus prophylaxis is necessary for burns or any break in skin integrity. b. Some institutions transfer these victims to a burn center for follow-up management. 6. Cold related injuries a. Hypothermia i. s/s 1. core body temperature below 95° F (35° C) 2. three categories by severity: a. mild (90° to 95° F [32° to 35° C]); b. moderate (82.4° to 90° F [28° to 32° C]); c. severe (below 82.4° F [28° C]). ii. treatment 1. Treatment decisions are based on the severity of hypothermia. 2. in the field a. mild hypothermia i. the person needs to be sheltered from the cold environment 1. have all wet clothing removed, and undergo passive or active external rewarming. ii. Passive methods involve applying warm clothing or blankets. iii. Active methods incorporate heating blankets, warm packs, and convective air heaters or warmers to speed rewarming. 1. If a heating blanket is used, monitor the patient's skin at least every 15 to 30 minutes to reduce the risk for burn injury. b. In the case of mild, uncomplicated hypothermia as the only health problem,i. having the victim drink warm high-carbohydrate liquids that do not contain alcohol or caffeine can aid in rewarming. 1. Alcohol is a peripheral vasodilator; both alcohol and caffeine are diuretics. 2. These effects can potentially worsen dehydration and hypothermia. ii. Treatment of moderate hypothermia may involve both active external and core (internal) rewarming methods. 1. Applying external heat with heating blankets can promote core temperature ―after-drop‖ by producing peripheral vasodilation. 2. ―After-drop‖ is the continued decrease in core body temperature after the victim is removed from the cold environment; it is caused by the return of cold blood from the periphery to the central circulation. a. Therefore the patient's trunk should be actively rewarmed before the extremities. 3. Core rewarming methods for moderate hypothermia include administration of warm IV fluids, heated oxygen or inspired gas to prevent further heat loss via the respiratory tract, and heated peritoneal, pleural, gastric, or bladder lavage. c. Patients who are severely hypothermic i. high risk for cardiac arrest. ii. Avoid using active external rewarming with heating devices because it is dangerous and contraindicated in this population due to rapid vasodilation. iii. The treatment of choice for severe hypothermia is to use extracorporeal rewarming methods 1. such as cardiopulmonary bypass or hemodialysis 3. hospital care a. Protect patients from further heat loss and handle them gently to prevent ventricular fibrillation. b. Positioning the patient in the supine position prevents orthostatic changes in blood pressure from cardiovascular instability. c. Follow standard resuscitation efforts with special attention to maintenance of airway, breathing, and circulationd. Administer drugs with caution and/or spaced at longer intervals because metabolism is unpredictable in hypothermic conditions. i. Remember that drugs can accumulate without obvious therapeutic effect while the patient is cold but may become active and potentially lead to drug toxicity as effective rewarming is underway ii. Consider withholding IV drugs, except vasopressors, until the core temperature is above 86° F (30° C) e. Initiate CPR for patients without spontaneous circulation. f. For a hypothermic patient in ventricular fibrillation or pulseless ventricular tachycardia i. one defibrillation attempt is appropriate. ii. Be aware that defibrillation attempts may be ineffective until the core temperature is above 86° F (30° C). b. Frostbite i. Degrees of frostbite characteristics – s/s 1. First-degree frostbite a. involves hyperemia (increased blood flow) of the involved area and edema formation. 2. In second-degree frostbite a. large fluid-filled blisters develop with partial-thickness skin necrosis. 3. Third-degree frostbite a. appears as small blisters that contain dark fluid and an affected body part that is cool, numb, blue, or red and does not blanch. b. Full-thickness and subcutaneous tissue necrosis occurs and requires débridement. 4. In fourth-degree frostbite a. the most severe form, b. there are no blisters or edema; c. the part is numb, cold, and bloodless. d. The full-thickness necrosis extends into the muscle and bone. e. At this stage, gangrene develops, which may require amputation of the affected part. ii. treatment 1. in the field a. Recognition of frostbite is essential to early, effective intervention and prevention of further tissue damage. b. Asking a partner to frequently observe for early signs of frostbite such as a white, waxy appearance to exposed skin, especially on the nose, cheeks, and ears, is an effective strategy to identify the problem before it worsens.c. In persons with dark skin, skin becomes paler, waxy, and somewhat gray. In this case, the best remedy is to have the person seek shelter from the wind and cold and to attend to the affected body part. d. Superficial frostbite is easily managed using body heat to warm the affected area. i. Teach patients to place their warm hands over the affected areas on their face or to place cold hands under the arms. e. Do not apply dry heat or massage the frostbitten areas as part of the warming process. i. These actions can produce further tissue injury 2. hospital care a. Patients with more severe and deeper forms of frostbite need aggressive management. b. For all degrees of partial-thickness to full-thickness frostbite, i. rapid rewarming in a water bath at a temperature range of 104° to 108° F (40° to 42° C) is indicated to thaw the frozen part. ii. Because patients experience severe PAIN during the rewarming process 1. this intervention is best accomplished in a medical facility; however, it may be done in another setting if no other options exist for prompt transport or rescue. iii. Administer analgesics, especially IV opiates, and IV rehydration. c. Apply only loose, nonadherent sterile dressings to the damaged areas. i. Avoid compression of the injured tissues. ii. Both topical and systemic antibiotics may be used. iii. Once a patient's frozen part has thawed, do not allow it to refreeze, which worsens the injury. iv. Antiprostaglandin therapy with ibuprofen may be used because it may decrease tissue damage for some patients 7. Altitude Related Illness in the field and hospital care a. 3 most common clinical conditions that are high altitude illnesses i. Mountain illness 1. AMS include reports ofa. throbbing headache, anorexia, nausea, and vomiting. b. Feeling chilled, irritable, and apathetic is also associated with AMS. c. The syndrome produces effects similar to an alcohol-induced hangover ii. HACE 1. high altitude cerebral edema 2. If AMS progresses to high altitude cerebral edema (HACE), a. the patient cannot perform ADLs and has extreme apathy. b. A key sign of HACE is the development of ataxia (defective muscular coordination). c. The patient also has a change in mental status with confusion and impaired judgment. d. Cranial nerve dysfunction and seizures may occur. e. If untreated, a further decline in the patient's level of consciousness results. f. Stupor, coma, and death can result from brain swelling and the subsequent damage caused by increased intracranial pressure over the course of 1 to 3 days. iii. HAPE 1. high altitude pulmonary edema 2. High altitude pulmonary edema (HAPE) often appears in conjunction with HACE but may occur during the progression of AMS within the first 2 to 4 days of a rapid ascent to high altitude, commonly on the second night. 3. It is the most common cause of death associated with high altitude. 4. Patients notice poor exercise tolerance and a prolonged recovery time after exertion. 5. Fatigue and weakness, as well as other signs and symptoms of AMS, are present. 6. Important clinical indicators of HAPE include a. a persistent dry cough and cyanosis of the lips and nail beds. b. Tachycardia and tachypnea occur at rest. c. Crackles may be auscultated in one or both lungs. d. Pink, frothy sputum is a late sign of HAPE. 7. A chest x-ray demonstrates pulmonary infiltrates and pulmonary edema.8. Arterial blood gas analysis shows respiratory alkalosis and hypoxemia (decreased oxygen). b. The most important intervention to manage serious altitude-related illnesses is descent to a lower altitude!!! c. Patients must be monitored carefully for any evidence of symptom progression. d. With mild AMS, i. the victim should be allowed to rest and acclimate at the current altitude. ii. The person is instructed not to ascend to a higher altitude, especially for sleep, until symptoms lessen. iii. If symptoms persist or worsen, he or she should be moved to a lower altitude as soon as possible. 1. Even a descent of about 1600 feet may improve the patient's condition and reverse altitude-related pathologic effects. iv. Oxygen should also be administered if available to effectively treat symptoms of AMS. e. For the treatment of HACE, i. early recognition of ataxia or a change in level of consciousness should prompt a rapid descent by rescuers or companions to a lower altitude. ii. While undergoing descent, the patient can be given supplemental oxygen and dexamethasone. iii. If mental status is severely impaired and the patient's airway is at risk, all drugs should be given parenterally. iv. Ultimately, the patient with HACE must be admitted to the hospital. Critical care management may be necessary. f. Like HACE, early recognition of HAPE is essential to improve the patient's chance for survival. i. Phosphodiesterase inhibitors such as tadalafil (Cialis) and sildenafil (Viagra) may be used to prevent HAPE because of their pulmonary vasodilatory effects. ii. When it occurs, HAPE is a serious condition that requires quick evacuation to a lower altitude, oxygen administration, and bedrest to save the patient's life. iii. If descent must be delayed because of weather conditions or other factors, oxygen administration is essential as soon as possible. iv. Keep the patient warm at all times. v. Drugs are not substitutes for descent and oxygen. 1. However, the treatment of HAPE may include the calcium channel blocker nifedipine (Procardia, Adalat PA , Apo-Nifed ) to decrease pulmonary vascular resistance.vi. Hospital admission is required. vii. In uncomplicated cases of HAPE, recovery occurs quickly but effects such as weakness and fatigue may persist for 2 weeks. 8. Drowning a. Difference b/t wet and dry drowning i. wet 1. the person has inhaled water which interferes with respiration and causes the circulatory system to collapse 2. Both fresh and salt water cause surfactant to wash out of the lungs, causing surface tension within the alveoli, increasing the size of the alveoli and causing bradycardia. 3. In both cases it causes pulmonary edema which can lead to secondary edema ii. dry 1. Dry drowning occurs when a person inhales water through the nose of mouth causing airway and difficulty breathing a. the airway closes up due to spasms caused by the presence of water. 2. It is called DRY because water does not enter the lungs 3. (because of the spasm of the vocal cords) 4. Death occurs when the vocal cords do not relax which prevents air from entering the lungs 5. It is most common in kids 6. It normally occurs less than an hour after inhaling the water b. Treatment i. in the field 1. Immediate emergency care focuses on a safe rescue of the victim. 2. Once rescuers gain access to the victim, the priority is safe removal from the water. 3. Spine stabilization with a board or flotation device should be considered only for those victims who are at high risk for spine trauma (e.g., history of diving, use of a water slide, signs of injury or alcohol intoxication) 4. Time is of the essence; efforts directed toward a rapid rescue have the most potential benefit. 5. Initiate airway clearance and ventilatory support measures, including delivering rescue breaths while the patient is still in the water, as soon as possible. 6. If hypothermia is a concern, handle the victim gently to prevent ventricular fibrillation. ii. hospital care 1. Do not attempt to get the water out of the victim's lungs; deliver abdominal or chest thrusts only if airway obstruction is suspected. 2. Once the person is safely removed from the water, airway and cardiopulmonary support interventions begin, including oxygen administration, endotracheal intubation, CPR, and defibrillation, if necessary.3. In the clinical setting, gastric decompression with a nasogastric or orogastric tube is needed to prevent aspiration of gastric contents and improve ventilatory function. 4. After a period of artificial ventilation by mask, the victim typically has a distended abdomen, which impairs movement of the diaphragm and decreases lung ventilation. 5. Patients who experience drowning require complex care to support their major body systems. 6. The full spectrum of critical care technology may be needed to manage the pathophysiologic complications of drowning, including pulmonary edema, infection, acute respiratory distress syndrome (ARDS), and CNS impairment. 9. Carbon monoxide poisoning. How does it occur? a. Definition i. a colorless, odorless, tasteless gas released in the process of combustion. Inhalation injury is a risk for carbon monoxide poisoning b. s/s i. dull headache ii. Weakness iii. Nausea vomiting iv. Confusion v. Dizziness vi. difficulty breathing c. basic treatment i. remove patient from source ii. NRB mask 15LPM and elevate HOB iii. Hyperbaric oxygen therapy iv. Normal Saline to restore volume d. Methelyne blue i. used to treat methemoglobinemia 1. The presence in the blood of methemoglobin a form of hemoglobin that is useless for carrying oxygen and delivering it to tissues throughout the human body. 10. Burns- classification, parkland formula, rule of nine, fluid resuscitation a. Burns are complex injuries with loss of TISSUE INTEGRITY that cause patients to develop many physiologic, metabolic, and psychological changes. i. Burns can either be 1. chemical burns 2. thermal burns 3. electrical burns4. radiation burns b. Parkland formula and rule of nine (look at work sheet given) c. fluid resuscitation: lactated ringers or normal saline (isotonic solutions) i. refer to parkland formula to determine how much to give Shock: Types, symptoms, causes and treatments Hypovolemic – 2 types Cardiogenic Obstructive Distributive: Neurogenic Anaphylaxis Septic What do these shock conditions look like on assessment. Central venous pressure, SVR, Fever, tachycardia, bradycardia, skin, peripheral pulses ect……. Mental Health Concepts Specific Medications for Exam – Mental Health Primary side effects of SSRIs ◦ Paroxetine, sertraline, duloxetine, desvenlafaxine, fluoxetine ◦ this drug allows more serotonin to stay at the junction of the neurons; takes up to 4 weeks to produce therapeutic medication levels ◦ EARLY adverse effects: ▪ nausea, diaphoresis, tremor, fatigue, drowsiness ◦ LATE adverse effects: ▪ after 5-6wks: sexual dysfunction (impotence, absent or delayed orgasm/ejaculation, decreased libido), weight gain, HA ◦ weight changes, GI bleeding (report dark stools/coffee emesis), hyponatremia, bruxism (grinding/clenching of teeth) ◦ Serotonin Syndrome – can begin 2-72hrs after tx; CAN BE LETHAL ▪ confusion, agitation, delirium, seizures – status epilepticus, tachycardia (leading to cardiovascular shock), labile BP, diaphoresis, fever, N/V/D, coma leading to apnea ▪ REPORT IMMEDIATELY Serious adverse effect of lithium ◦ Lithium is a mood stabilizer – used for Bipolar Disorders ◦ produces neurochemical changes in the brain, including serotonin receptor blockade ◦ can cause goiter and hypothyroidism ▪ with long-term treatment ▪ obtain baseline T3, T4, TSH levels prior and then annually ▪ watch for cold, dry skin, decreased heart rate, weight gain ▪ give levothyroxine ◦ SERIOUS ADVERSE EFFECTS: ▪ Kidney Toxicity: monitor I&O, adjust dosage, and keep doseat lowest level, monitor BUN/creatinine periodically ▪ Bradysrhythmias, hypotension, and electrolyte imbalances: maintain adequate fluid and sodium intake ▪ Lithium toxicity: Early indications: ◦ lithium level – less than 1.5 mEq/L, ◦ manifestations – D/N/V, polyuria, muscle weakness, fine hand tremors, slurred speech, lethargy ◦ withhold medication and notify HCP, administer new dose based on serum lithium and Na levels Advanced Indications: ◦ lithium level – 1.5-2.0 mEq/L, ◦ manifestations – mental confusion, sedation, poor coordination, coarse tremors, ongoing N/V/D ◦ withhold and notify, administer new dose based on serum levels, excretion may need to be promoted Severe toxicity:◦ lithium level – 2.0-2.5 mEq/L ◦ manifestations – extreme polyuria (dilute urine), tinnitus, giddiness, jerking movements, blurred vision, ataxia, seizures, severe hypotension and stupor leading to coma, death (from possible resp. complications) ◦ administer emetic to alert clients or gastric lavage, urea, mannitol, or aminophylline may be prescribed to increase the rate of excretion lithium levels > 2.5 ◦ rapid progression of manifestations leading to coma and death ◦ hemodialysis can be warranted S/S of extrapyramidal effects ◦ tremor, slurred speech, akathesia (feeling off inner restlessness and inability to stay still), dystonia (person’s muscles contract uncontrollably), anxiety, distress, paranoia, and bradyphrenia (slowed thinking) S/S of tardive dyskinesia ◦ characterized by: involuntary and abnormal movements of the jaw, lips, and tongue ◦ symptoms: facial grimacing, sticking out the tongue, sucking or fish-like movements of the mouth MAOIs – what happens if patient eats foods with tyramine ◦ monoamine oxidase inhibitors ◦ phenelzine (prototype medications) ◦ blocks MAO in the brain – increasing the amount of norepinephrine, dopamine, and serotonin available for transmission of impulses – an increased amount of these neurotransmitters at nerve endings intensifies responses and relieves depression ◦ HYPERTENSIVE CRISIS ▪ this happens from INTAKE OF DIETARY TYRAMINE as well as being on MAOIs: classified as severe HTN as a result of intensive vasoconstriction and stimulation of the heart ▪ manifestations include: HA, N/V, Increased HR/BP, diaphoresis, change in LOC ▪ RN actions: administer phentolamine IV (rapid acting alpha adrenergic blocker or nifedipine provide continuous cardiac monitoring and respiratory support teaching: Zoloft also known as Sertraline◦ a type of selective serotonin reuptake inhibitors – antidepressants ◦ TEACHING: ▪ report suicidal thoughts and behaviors (especially at the START OF THERAPY) ▪ teach that it can take up to 4 weeks to achieve therapeutic effects ▪ take medication on a daily basis to establish theraputic plasma levels ▪ may be taken with food ▪ sleep disturbances are minimized by taking the medication in the morning ▪ avoid concurrent use with lithium and TCAs ▪ concurrent use with MAOIs, TCAs, St. John’s wort can increase risk of serotonin syndrome ▪ wear sunscreen – photosensitivity taking antidepressant that causes anticholinergic side effects, what can the patient be at risk for? ◦ Drugs that cause anticholinergic side effects are drugs that are antidepressants – example would be amitriptyline – Elavil ◦ side effects of Elavil: dry mouth, constipation, dry eyes, blurred vision, urinary retention, hypotension, confusion, headache ◦ patient can be at risk for: pneumonia or dementia Klonopin – patient refuses to take – watch for what? ◦ Abrupt disruption or withdrawal: patient is AT RISK FOR status epilepticus, tremors, N/V, abdominal and muscle cramps ◦ place on seizure precautions!! Zyprexa – watch for what with the 1st dose? ◦ A type of antipsychotics/mood stabilizers ◦ observe for S/S of post-injection delirium/sedation syndrome ▪ dizziness, confusion, disorientation, slurred speech, altered gait, difficulty ambulating, weakness, agitation, extrapyramidal symptoms, hypertension, convulsion, reduced level of consciousness ranging from mild sedation to coma – for at least 3hrs after injection ▪ Monitor BP (sitting, standing, lying), ECG, pulse, and respiratory rate before and frequently during dose adjustment.▪ Assess mental status (orientation, mood, behavior) before and periodically during therapy. Patient taking Haldol and Depakote – why give them together? ◦ Okay so I do not know this one specifically, but I do know this…Haldol as an adverse effect and it gives seizures and Depakote is an anticonvulsant (used for seizures) and that is the only correlation I had with the two drugs. Another thing is they both decrease manic states but I feel like the seizure one made more sense. – please correct me if I am wrong! ▪ HALDOL MOA/Therapeutic effects: Alters the effects of dopamine in the CNS; Also has anticholinergic and alphaadrenergic blocking activity. Diminished signs and symptoms of psychoses (schizophrenia, manic states, druginduced psychoses); Also useful in managing aggressive or agitated patients. ▪ DEPAKOTE MOA/Therapeutic effects: Increase levels of GABA, an inhibitory neurotransmitter in the CNS. Suppression of seizure activity, Decreased manic episodes, Decreased frequency of migraine headaches Clozaril – teaching priority to report to HCP ◦ neuroleptic malignant syndrome ▪ Instruct patient to notify health care professional promptly if the following occur: unexplained fatigue, dyspnea, tachypnea, chest pain, palpitations, sore throat, fever, lethargy, weakness, malaise, or flu-like symptoms occur. ◦ Respiratory status: ▪ DVT, acute dyspnea, chest pain, or other resp. S/S occur – consider pulmonary embolism! Naltrexone (Re Via) used for what? ◦ Management of opioid and alcohol dependence ◦ Competitively blocks the effects of opioids, including CNS and respiratory depression, without producing any agonist (opioid-like) effects – Mechanism in managing alcohol dependence may involve the endogenous opioid system Important labs when starting Tegretol ◦ also known as carbamazepine ◦ Decreases synaptic transmission in the CNS by affecting sodium channels in neurons▪ Monitor ECG and serum electrolytes before and periodically during therapy. May cause hyponatremia. ◦ Monitor CBC: including platelet count, reticulocyte count, and serum iron ▪ at baseline, weekly during the first 2 mo, and yearly thereafter ▪ for evidence of potentially fatal blood cell abnormalities. Discontinue therapy if bone marrow depression occurs. ◦ Perform liver function tests, urinalysis, electrolytes, serum creatinine, and BUN ▪ at baseline and routinely performed ▪ May cause ↑ AST, ALT, serum alkaline phosphatase, bilirubin, BUN, urine protein, and urine glucose levels ◦ Toxicity Overdose: ▪ Serum blood levels should be routinely monitored during therapy ▪ Therapeutic levels range from 4–12 mcg/mL. Matching (term with definition or description) Buspar: ◦ buspirone ◦ Management of anxiety ◦ Binds to serotonin and dopamine receptors in the brain; increases norepinephrine metabolism in the brain. Tyramine: ◦ Tyramine is an amino acid that helps regulate BP; occurs naturally in the body and is found in certain foods ▪ aged cheese (blue, parmesan, cheddar), smoked or processed meats (salami, summer sausage), caviar, chicken/beef liver, red wines and raisins (avoid these foods if taking MAOIs) ◦ *MOAIs block monoamine oxidase, which is an enzyme that breaks down excess tyramine in body – so if you take MAOIs you will have increase tyramine Psychosis: ◦ a severe mental disorder in which thought and emotions are so impaired that contact is lost with external reality Mania: ◦ a state of abnormally elevated arousal, affect, and energy level, or "a state of heightened overall activation with enhanced affective expression together with lability of affect." ◦ Extremely elevated and excitable mood usually associated with bipolar disorder. Valium: ◦ drug name: diazepam ◦ CLASS: anti-anxiety agents, skeletal muscle relaxants, sedative/hypnotics; benzodiazepines ◦ MOA: ▪ Depresses the CNS, probably by potentiating GABA, an inhibitory neurotransmitter ▪ Produces skeletal muscle relaxation by inhibiting spinal polysynaptic afferent pathways Elavil: ◦ drug name: amitriptyline ◦ CLASS: antidepressants; tricyclic antidepressants ◦ MOA: ▪ Potentiates the effect of serotonin and norepinephrine in the CNS ▪ Has significant anticholinergic properties. Risperdal: ◦ drug: risperidone ◦ CLASS: antipsychotics, mood stabilizers; benzisoxazoles ◦ MOA: ▪ May act by antagonizing dopamine and serotonin in the CNS ▪ Decreased symptoms of psychoses, bipolar mania, or autism Anxiety: ◦ Intense, excessive, and persistent worry and fear about everyday situations ◦ Fast heart rate, rapid breathing, sweating, and feeling tired may occur. Depression:◦ mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life. Bipolar affective disorder: ◦ disorder associated with episodes of mood swings ranging from depressive lows to manic highs Extrapyramidal: ◦ relating to or denoting nerves concerned with motor activity that descend from the cortex to the spine and are not part of the pyramidal system. Few Other Notes to Review Serious side effects of lithium ◦ look up top under ―lithium‖ ◦ depends on lithium levels Intervention for schizo staring at wall ◦ may be experiencing visual hallucinations ◦ ask what is wrong; do not go along with their hallucinations though and do not argue with their hallucinations ◦ kinda look at the auditory interventions below because it some what plays off of that too ◦ provide milieu therapy: a structured, safe environment Teaching behavior – modification with eating disorders ◦ diet teachings and interventions ▪ provide a diet high in fiber to prevent constipation ▪ diet low in sodium to prevent fluid retention ▪ imit high fat and gassy foods during start of treatment ▪ small, frequent meals ▪ structured and inflexible eating schedule ▪ consider clients preferences ▪ avoid caffeine ◦ promote and reinforce teaching about cognitive-behavioral therapies ▪ cognitive re-framing ▪ relaxation techniques ▪ journal writing▪ systematic desensitization exercises Nursing intervention for antisocial personality outbursts ◦ Antisocial: Cluster B ▪ characterized by disregard for others with exploitation, lack of empathy, repeated unlawful actions, deceit, and failure to accept personal responsibility have a sense of entitlement, manipulative, impulsive, and seductive non-adherence to traditional morals and values; verbally charming and engaging ◦ Self assessment is vital for nurses caring for clients who have personality disorders and should be performed prior to care: ▪ self-assessment is the process of looking at oneself in order to assess aspects that are important to one's identity. It is one of the motives that drive self-evaluation, along with self-verification and selfenhancement. ▪ clients who have personality disorders can evoke intense emotions in the nurse ◦ communication strategies: ▪ limit-setting and consistency are essential with clients who are manipulative, especially those who have antisocial personality disorders ▪ have a firm, yet supportive approach and consistent care Violence from paranoid patient on unit – intervention ◦ How to de-escalate an aggressive client ▪ 1st ensure safety of the patient, staff, and others in the area ▪ Respect personal space, ▪ do not be provocative, ▪ be concise – keep messages clear and simple, ▪ identify wants and feelings, ▪ listen closely to what the person is saying, ▪ set clear limits, offer choices and optimism S/S of panic (anxiety)◦ panic disorder: client experiences recurrent panic attacks ◦ S/S usually last 15-30 minutes – four or more of the following are present: ▪ palpitations ▪ SOB ▪ choking or smothering sensation ▪ chest pain ▪ nausea ▪ feels of depersonalization ▪ fear of dying or insanity ▪ chills or hot flasshes EPS S/S ◦ extrapyramidal symptoms ▪ dystonia (continuous spasms and muscle contractions), ▪ akathisia (may manifest as motor restlessness), ▪ parkinsonism (characteristic symptoms such as rigidity), ▪ bradykinesia (slowness of movement), ▪ tremor, ▪ and tardive dyskinesia (irregular, jerky movements). ◦ **tardive dyskinesias simply mean late onset of the same EPS movement side effects Why does tooth enamel deteriorate with bulimia ◦ with bulimia, clients typically eat large quantities of food over short periods of time usually followed by behaviors like self-induced vomiting (also known as purging) ◦ when vomiting – you rid of acid from the stomach ◦ frequent self induced vomiting can wear away tooth enamel (the acid wears it away!!) ▪ This may leave a hole or a cavity Intervention for paranoid patient with bizarre behaviors◦ monitor client for paranoid delusions – which can increase the risk for violence against others ◦ promote therapeutic communication to lower anxiety, decrease defensive patterns, and encourage participation in the milieu ◦ milieu: a therapy used for clients who have a psychotic disorder ▪ provides a structured, safe environment (milieu) for the client in order to decrease anxiety and to distract the client from constant thinking about hallucinations Nursing response to schizo patient hearing voices ◦ when a patient hears voices it is known as hallucinations that are auditory: ▪ hearing voices or sounds ▪ if it is a command: the voice instructs the client to perform an action, such as to hurt self or even others ◦ the RN should NOT argue or agree with the client’s views of the situation, they can offer a comment like this: ▪ ―I do not hear anything, but you seem to be feeling frightened‖ ◦ if the client is experiencing command hallucinations ▪ provide for safety due to increase risk for harm to self or others ◦ know what triggers auditory hallucinations ▪ some clients are triggered by loud noises ◦ some symptom management techniques for auditory hallucinations: ▪ music to distract from ―voices‖ ▪ interaction with an auditory hallucination by telling it to stop or go away Differentiate between positive and negative symptoms of schizo ◦ POSITIVE: manifestation of things that are not normally present ▪ hallucinations ▪ delusions ▪ alterations in speech ▪ bizarre behavior such as walking backwards constantly◦ NEGATIVE: absence of things that are normally present. These manifestations are more difficult to treat successfully than positive symptoms ▪ affect: usually blunted (narrow range of expression) or flat (facial expression never changes) ▪ alogia: poverty of thought or speech. The client might sit with a visitor but only mumble or respond vaguely to questions ▪ anergia: lack of energy ▪ anhedonia: lack of pleasure or joy; client is indifferent to thinks that often make others happy ▪ avolition: lack of motivation in activities and hygiene Manic intervention to help increase nutrition ◦ Patients who are bipolar will have manic episodes and one manic characteristic finding is ▪ a neglect of ADLs, including nutrition and hydration ◦ monitor sleep, fluid intake, and nutrition ▪ provide nutritious but portable foods – because the client might not be able to sit down to eat AIMS used to assess what ◦ abnormal involuntary movement scale ◦ USE AIMS TEST TO SCREEN FOR EPSs ▪ pseudoparkinsonism, acute dystonia, akathisia, and tardive dyskinesia Position for ECT ◦ electroconvulsive therapy uses electrical current to induce brief seizure activity while the client is anesthetized ▪ PLACE IN SIDE LYING POSITION – DUE TO PATIENT BEING AT RISK FOR SEIZURES AFTER PROCEDURE Interventions/priorities for suicide patient ◦ IMPLEMENT SAFETY PRECAUTIONS OR ONE-TO- ONE OBSERVATION AS NEEDED ◦ if patient does have one-to-one observation and you are the RN in charge and had to step out; YOU MUST ALWAYS MAKE SURE SOMEONE IS IN THERE, patient must NEVER be alone Med used to treat opioid withdraw ◦ Narcan is for toxicity ◦ Naltrexone (Re Via) – which is used as part of Tx for drug dependence (opioids) Major influence in development of anorexia nervosa ◦ occupational choices that encourage thinness ▪ (fashion modeling) ◦ picky eaters history ◦ participation in athletics ▪ (bicycling or runners – lean body build is ideal for this sport) ◦ family genetics: ▪ history of eating disorders ◦ environmental factors: ▪ society views of the perfect body ◦ temperamental: ▪ anxiety in childhood ◦ psychological influences: ▪ depression, distorted body image, physical abuse history ◦ Interpersonal relationships: ▪ influenced by others around them ◦ biological: ▪ hypothalamic, hormonal, neurotransmitter, or biochemical imbalance – with disturbances of the serotonin neurotransmitter pathways seeming to be implicated DRUGS – LOOK AT ALL TICKET TO TEST DRUGS MADE FOR EACH TEST AND COMPARE TO LIST BELOW. REPRODUCTIVE AND GENITOURINARY SYSTEMS Female reproductive drugs Estrogen and progesterone hormones 1. Drug therapy for contraception and premenstrual syndrome (PMS) Oral contraceptives – ethinyl estradiol and drospirenone (Yasmin) 2. Drug therapy for menopauseEstrogen HRT Oral – conjugated equine estrogen (Premarin) Transdermal – estradiol (Estraderm) Intravaginal – estradiol (Vagifem, Estrace Vaginal Cream) Estrogen and progesterone HRT Oral – conjugated estrogen and medroxyprogesterone acetate (Prempro) Transdermal – estradiol and norethindrone acetate transdermal system (CombiPatch) 3.Drug therapy for endometrial hyperplasia and endometriosis GnRH agonist – leuprolide (Lupron, Lupron Depot) Progesterone – medroxyprogesterone acetate (Provera) Ovulation-related hormones 4. Drug therapy for infertility LH and FSH stimulant – clomiphene (Clomid) Ovulation stimulant – hCG (Pregnyl) Hyperprolactinemia inhibitor – cabergoline Male reproductive drugs 5. Drug therapy for replacement of androgens Testosterone – testosterone (Androderm, Delatestryl) 6. Drug therapy for benign prostatic hypertrophy and outflow disorders 5-alpha reductase inhibitor – finasteride (Propecia, Proscar) Alpha-adrenergic receptor antagonists – tamsulosin (Flomax) 7. Drug therapy for erectile dysfunction Phosphodiesterase inhibitors PDE5 inhibitor – sildenafil (Viagra) Specific antibiotics/antifungals for STIs/vaccine STI Syphilis- Penicillin G HPV – Gardasil (recombinant human papilloma vaccine) Podofilox (Condylox) Chlamydia- Azithromycin(Zithromax) Doxycycline (Vibramycin)Gonohrea- Ceftriaxone (Rocephin) Specific Cancer Drugs Chemotherapy for cancer Breast CancerAnthracyclines:doxorubicin (Adriamycin) Taxanes:paclitaxel (Taxol) 5-fluorouracil (5-FU) Cyclophosphamide (Cytoxan) Carboplatin (Paraplatin) Most often, combinations of 2 or 3 of these drugs are use Prostate Cancer-Docetaxel (Taxotere) Hormone Therapy for cancer Breast cancer: Tamoxifen Prostate: Leuprolide (Lupron, Eligard) Bicalutamide (Casodex) Ketoconazole (Nizoral) Estrogen (female) hormon Vaccine for Prostate cancer : Sipuleucel-T (Provenge) is a cancer vaccine. Unlike traditional vaccines, which boost the body’s immune system to help prevent infections, this vaccine boosts the immune system to help it attack prostate cancer cells. The vaccine is used to treat advanced prostate cancer that's no longer responding to hormone therapy but is causing few or no symptoms. This vaccine is made specifically for each man. To make it, white blood cells (cells of the immune system) are removed from your blood over a few hours while you are hooked up to a special machine. The cells are then sent to a lab, where they are exposed to a protein from prostate cancer cells called prostatic acid phosphatase (PAP). The cells are then sent back to the doctor’s office or hospital, where they are given back to you by infusion into a vein (IV). This process is repeated 2 more times, 2 weeks apart, so that you get 3 doses of cells. The cells help your other immune system cells attack the prostate cancer. The vaccine hasn’t been shown to stop prostate cancer from growing, but it seems to help men live an average of several months longer. As with hormone therapy and chemotherapy, this type of treatment has not been shown to cure prostate cancer. Studies are now being done to see if this vaccine can help men with less advanced prostate cancer. Possible side effects of vaccine treatment Side effects from the vaccine tend to be milder than those from hormone therapy or chemotherapy. Common side effects can include fever, chills, fatigue, back and joint pain, nausea, and headache. These most often start during the cell infusions and last no more than a couple of days. A few men may have more severe symptoms, including problems breathing and high blood pressure, which usually get better after treatment ATINEOPLASTIC -CANCER DRUGS Cytotoxic drugs: 11. Anti-metabolites Folic acid analog – methotrexate (MTX) (Rheumatrix) Pyrimidine analog – cytarabine (Cytosar-U, DepoCyt)Purine analogs – mercaptopurine (Purinethol) 12. Alkylating Agents Nitrogen mustards – cyclophosphamide (Cytoxan) Nitrosoureas – carmustine (BiCNU) 13. Platinum compounds cisplatin (Platinol) 14. Antitumor antibiotics Anthracyclines –doxorubicin (Adriamycin, Doxil) 15. Antimitotics Vinca alkaloid – vincristine (Oncovin) Taxanes – paclitaxel (Taxol, Abraxane) 16. Topoisomerase inhibitors topotecan (Hycamtin) Hormonal agents : Gonadotropin-releasing hormone agonists – leuprolide (Lupron, Lupron Depot) Androgen receptor blockers – flutamide Estrogen receptor blockers – tamoxifen (Soltamox) Aromatase inhibitors – anastrozole (Arimidex) Monoclonal antibody: trastuzumab (Herceptin) Rituximab (Rituxin) Biologic response modifiers: Interferon – interferon alfa-2a (Roferon-A) interferon alfa-2b (Intron A) Targeted antineoplastic drugs BCR-ABL tyrosine kinase inhibitor – imatinib (Gleevec) Rheumatoid: DMARDS ; Etanercept (Enbrel) Adalimumab humiraInfliximab (Remicade) Rituximab (Rituxin) Azothioprine (Imuran) Hydroxychloroquinine – Plaquenil Cyclophosphamide (Cytoxin) Other drugs used for RA: Folic acid analog – methotrexate (MTX) (Rheumatrix) Prednisone (deltasone) Nsaids Anaphylaxis Epinephrine Diphenylhydramine (Benadryl) Histamine Blocker SLE Drugs: Hydroxychloroquinine – Plaquenil Prednisone (deltasone) Azothioprine (Imuran) Folic acid analog – methotrexate (MTX) (Rheumatrix) Immunosuppressants (Transplant Drug) Cyclosporine (Sandimmune) ANTI-VIRAL DRUGS FOR HIV – look at drug cards Eye drops Prostaglandin agonists Lantanoprost (Xalatan) Bimatoprost (Lumigan) Travaprost (Travatan) Beta-Adrenergic Blockers Betaxolol hydrochloride (Betoptic) Timolol (Timoptic, Istalol,Betimol) Andrenergic agonistBrimonidine tartrate (Alphagan P) Cholinergic Drugs (miotics) Echothiophate (phospholine iodide) Pilocarpine (Isopto Carpine) Carbonic Anhydrase Inhibitors Dorzolamide (Trusopt) Mydriatics (Sympathomimetics) ―—onidine‖ Cycloplegics Atropine Elimination – drug cards Drug List For Renal (11 total) Alucap (aluminum hydroxide) is a phosphate binder which contains aluminum. It is very effective at binding phosphate, but if taken over a long period of time, aluminum can build up in the body, possibly causing memory problems. Your doctor will measure your aluminum levels if you take Alucaps. Side effects of Alucaps include constipation. Alucaps should be swallowed whole 10-15 minutes before meals. Phosex (calcium acetate) is another phosphate binder which contains calcium. It should be swallowed whole and taken 10-15 minutes before meals. Renagel (sevelamer) is a phosphate binder which doesn’t contain calcium or aluminum. The tablets should be swallowed whole with meals. Medicines for electrolyte imbalances Kayexelate Potassium chloride Magnesium Sulfate Diuretics: WHEN YOU MAKE YOUR DRUG CARDS DO BY CLASS 1.Loop diuretics: Furosemide (Lasix) Bumex Demadex 2.Thiazide and thiazide like diuretics: Hydrochlorothiazide (Hydrodiuril) Diuril3.Osmotic Diuretics: Mannitol 4.Carbonic Anhydrase Inhibitors: Diamox 5.Potassium Sparing diuretics: Aldactone Inspra Note that…..ACE inhibitors and ARBs. These may be used if you have protein in your urine (proteinuria) or have heart failure. Regular blood tests are required to make sure that these medicines don't raise potassium levels (hyperkalemia) or make kidney function worse. Drug therapy for hypertension RAAS Suppressants ■ ACE inhibitors – captopril (Capoten) ■ ARBs – losartan (Cozaar) ■ Aldosterone antagonists – eplerenone (Inspra) ■ Direct renin inhibitors – aliskiren (Tekturna) Calcium channel blockers – nifedipine (Adalat, Procardia) Sympatholytics ■ Alpha1 adrenergic blockers – doxazosin (Cardura) ■ Beta adrenergic blockers – atenolol (Tenormin), metoprolol (Lopressor) ■ Adrenergic neuron blockers – reserpine ■ Centrally acting alpha2 agonists – clonidine (Catapres) ■ Alpha/beta blockers – carvedilol (Coreg) Direct acting vasodilators – hydralazine ● Drug therapy for heart failure Diuretics ■ Thiazide diuretics – hydrochlorothiazide (HydroDIURIL) ■ Loop diuretics – furosemide (Lasix) ■ Potassium-sparing diuretics – spironolactone (Aldactone) Cardiac glycosides – digoxin (Lanoxin)Sympathomimetics – dobutamine Phosphodiesterase inhibitors – milrinone (Primacor) Drug therapy for coronary heart disease Antilipidemic ◦ HMG-CoA reductase inhibitors (statins) – atorvastatin (Lipitor), simvastatin(Zocor) ◦ Fibrates – gemfibrozil (Lopid) Fenofibrate (Zocor) ◦ Niacin (Vitamin B3) ◦ Bile Acid Sequestrant- Questran (Cholestyramine) Antianginals ◦ Nitrates – nitroglycerin (Nitrostat, Nitro-Dur), isosorbide (Isordil) Drug therapy for cardiac dysrhythmias Class I/sodium channel blockers ◦ Class IA – quinidine, procainamide ◦ Class IB – lidocaine (Xylocaine) ◦ Class IC – flecainide (Tambocor) Class II/beta adrenergic blockers – propranolol (Inderal) Class III/potassium channel blockers – amiodarone (Cordarone) Class IV/calcium channel blockers – verapamil (Calan) Acute coronary Syndrome Oxygen Aspirin Nitroglycerin- Prototype Anti-angina nitrate Morphine Integrellin- Prototype Glycoprotein IIb/IIIa antagonist Streptokinase-Prototype Fibrinolytic Heparin Ventricular Fibrillation or Ventricular tachycardia Epinephrine- Prototype sympathomimetic beta agonist Amiodarone-prototype Class 3 anti-dysrhythmic drugLidocaine class 1B antidysrythmic Sodium channel blocker Magnesium-prototype electrolyte replacement DRUGS FOR BRADY-DYSRHYTHMIA Atropine- Prototype positive chronotropic Epinephrine- Prototype sympathomimetic beta agonist Dopamine DRUGS FOR TACHYCARDIAS Adenosine- Prototype negative Chronotropic Diltiazem- Prototype Class 4 anti dysrhythmic Calcium channel blocker Lopressor- Prototype Class 2 anti dysrhythmic beta blocker Digoxin- Prototype positive inotrope Amiodarone- prototype Class 3 anti-dysrhythmic drug Potassium Channel blocker Verapamil Magnesium- prototype electrolyte replacement DRUGS FOR ASYSTOLE/PEA Epinephrine- Prototype sympathomimetic beta agonist VASOCONSTRICTORS Vassopressin Phenylephrine- Prototype Vasoconstrictor ANTILIPIDEMICS HMG-CoA reductase inhibitors (statins) ◦ atorvastatin (Lipitor), simvastatin(Zocor) Fibrates ◦ gemfibrozil (Lopid) Fenofibrate (Tricor) Niacin (Vitamin B3) Bile Acid Sequestrant ◦ Questran (Cholestyramine) ANTI DYSRHYTHMICS Moricizine Class I fast channel sodium blocker Quinidine- Prototype Class IA antidysrhythmic Sodium channel blocker Lidocaine class 1B antidysrythmic Sodium channel blockerFecanide class 1C sodium channel blocker Lopressor- Prototype Class 2 anti dysrhythmic beta blocker Amiodarone-prototype Class 3 anti-dysrhythmic drug Potassium Channel blocker Diltiazem-Prototype Class 4 anti dysrhythmic Calcium channel blocker Drugs for Exam DVT/PE/CVA – exam 8 drugs; look at drug cards Anticoagulants Factor Xa and thrombin inhibitors Heparin Fondaparinux-Arixtra Dalteparin (Fragmin) enoxaparin (Lovenox) Low molecular weight heparin Vitamin K inhibitor – warfarin (Coumadin) Thrombin Inhibitor-Dabigatran (Pradaxa) Factor Xa Inhibitor-Apixaban (Eliquis) Factor Xa Inhibitor- Rivaroxaban (Xarelto) Antiplatelets-Drugs that Prevent platelet adhesion ■ Salicylics – aspirin (Ecotrin) ■ ADP Inhibitors – clopidogrel (Plavix) Drugs that break down, or lyse, preformed clots Older drugs streptokinase and urokinase Current drugs alteplase (Activase, Cathflo Activase,tPA) reteplase (Retavase) tenecteplase (TNKase) Antidotes Aminocaproic acid (Amicar) Vitamin K (AquaMEPHYTON) Protamine Sulfate Micellaneous drugs for CVA Nifedipine (Nimotop) Labateolol (Normodyne) Prednisone Mannitol Antilipidemics: HMG-CoA reductase inhibitors (statins) – atorvastatin (Lipitor) simvastatin Fibrates – gemfibrozil (Lopid) Fenofibrate (Zocor) Niacin (Vitamin B3) Bile Acid Sequestrant- Questran (Cholestyramine) Drugs for Medical Emergencies – did not make drug cards for but you should already know these drugs (easy drugs, look up if not sure) Dopamine (Inotropin) o used to improve BP, cardiac output, urine output in treatment of shock o also increases renal perfusion with small doses by producing renal vasodilation Sodium Nitroprusside (Nipride) o a vasodilator and antihypertensive; o used for hypertensive crises and cardiac pump failure or cardiogenic shock o Produces peripheral vasodilation by a direct action on venous and arteriolar smooth muscle Phenylephrine o vasopressors, adrenergics & alpha adrenergic agonists. o Management of hypotension associated with shock that may persist after adequate fluid replacement; o Management of hypotension associated with anesthesia. o Constricts blood vessels by stimulating alpha-adrenergic receptors. Epinephrine o antiasthamtic, bronchodilators, vasopressors o adrenergics o Used for severe allergic reactions Norepinephrine (Levophed) o vasopressors o Produces vasoconstriction and myocardial stimulation, which may be required after adequate fluid replacement in the treatment of severe hypotension and shock. Neosynephrine Dobutamine (Dobutrex) o inotropics, adrenergics o Increased cardiac output without significantly increased heart rate. o Short-term (<48 hr) management of heart failure Milrinone (Primacor) o inotropics; o Short-term treatment of HF unresponsive to conventional therapy with digoxin, diuretics, and vasodilators.o Increased cardiac output (inotropic effect). o Increases myocardial contractility. o Decreases preload and afterload by a direct dilating effect on vascular smooth muscle. CroFab (crotalidae polyvalent immune fab-(ovine) o used for snake bites (pit viper ones) Methylene Blue o used for carbon monoxide poisoning Mental Health Concept – look at drug cards aripiprazole/abilify diazapam/valium venlafaxine/effexor Lorazapam/ativan escatalopram/zoloft trazadone/desyrel clonazepam/klonopin citolopram/celexa duloxetine/cymbalta buprenorphine/ naloxone (suboxone) Memantine/Namenda Quetiapine/seraquel Alprazolam/Xanex Olanzapine/Zyprexa Growth and Development Concept Amphetamines – Adderall Methylphenidate-Ritalin [Show More]
Last updated: 1 year ago
Preview 1 out of 180 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 16, 2021
Number of pages
180
Written in
Additional information
This document has been written for:
Uploaded
May 16, 2021
Downloads
0
Views
94


.png)
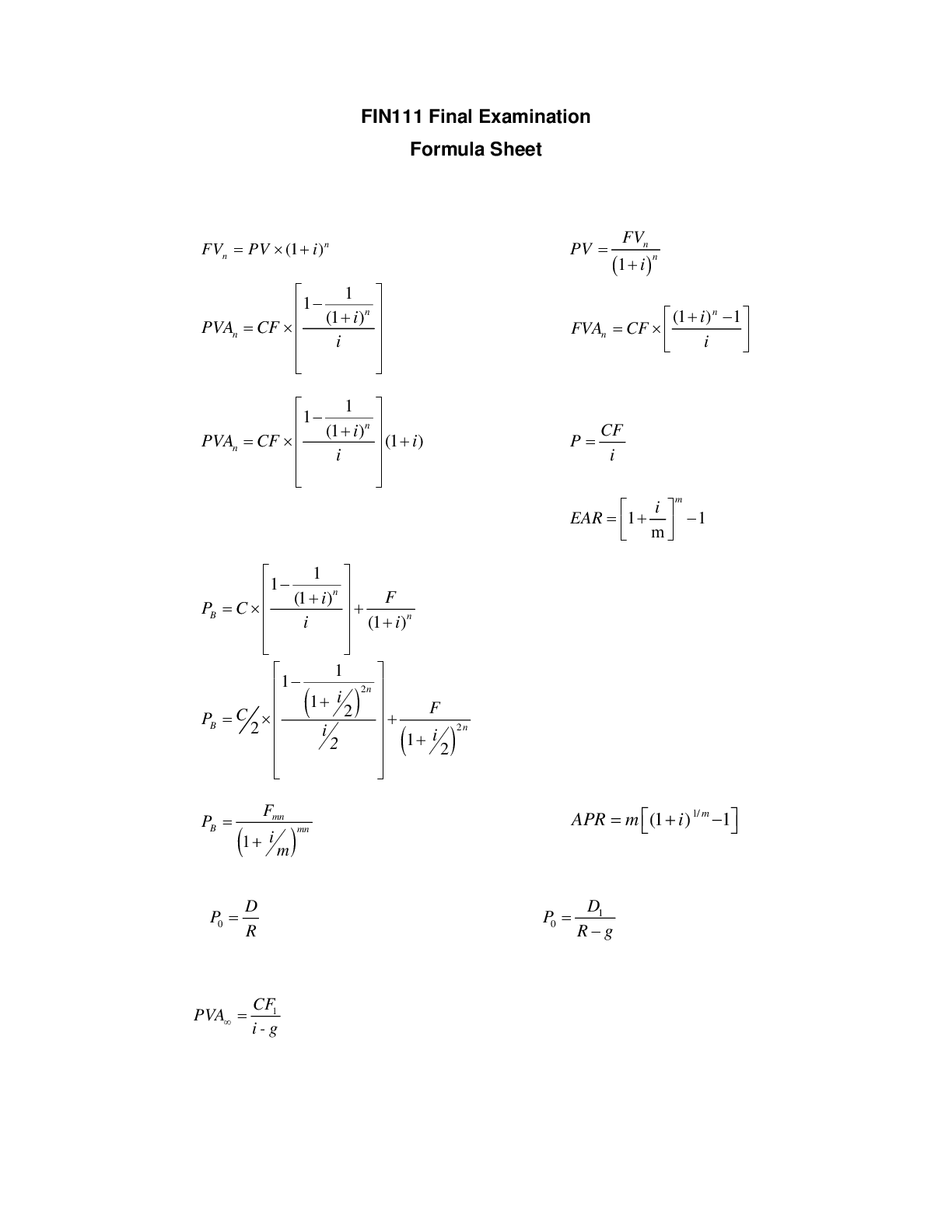
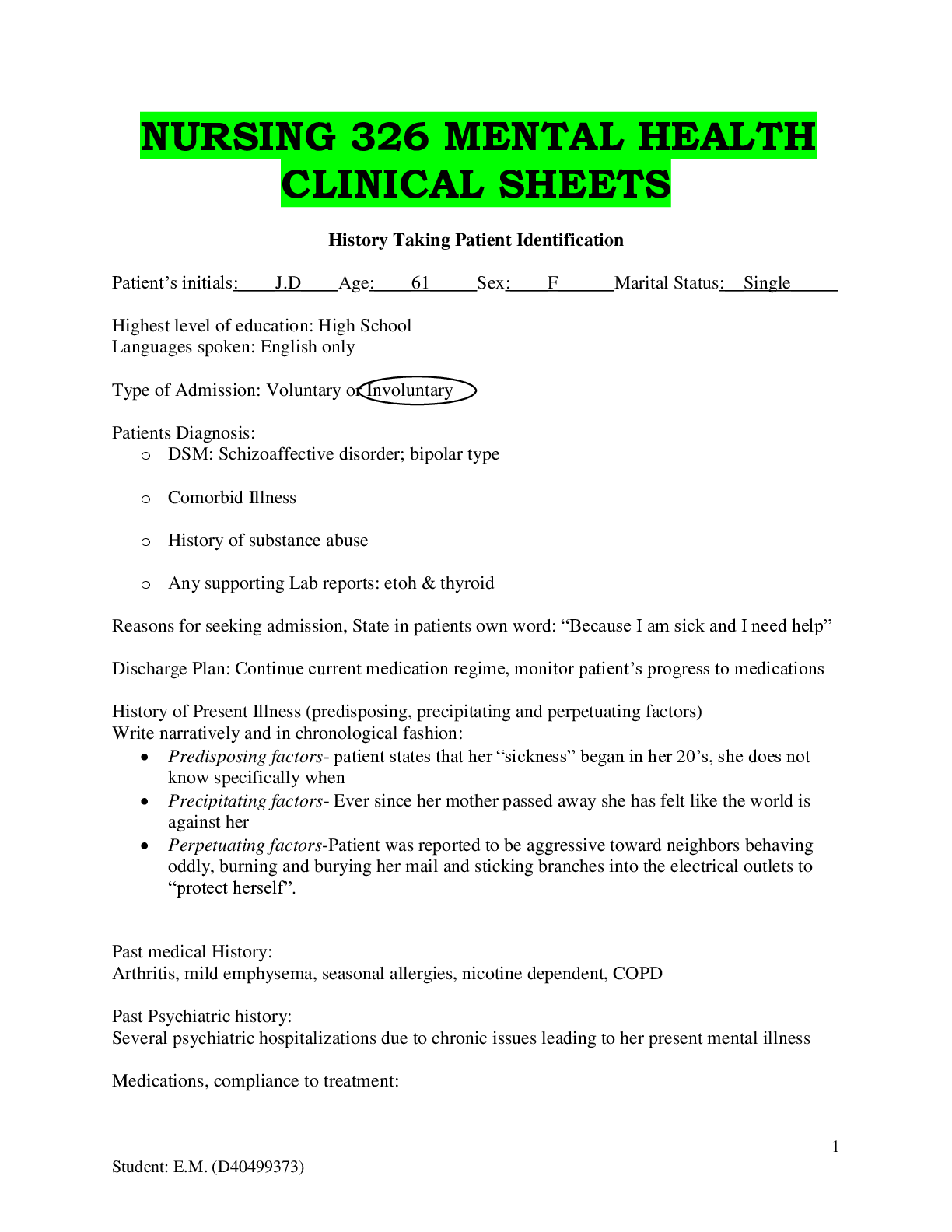
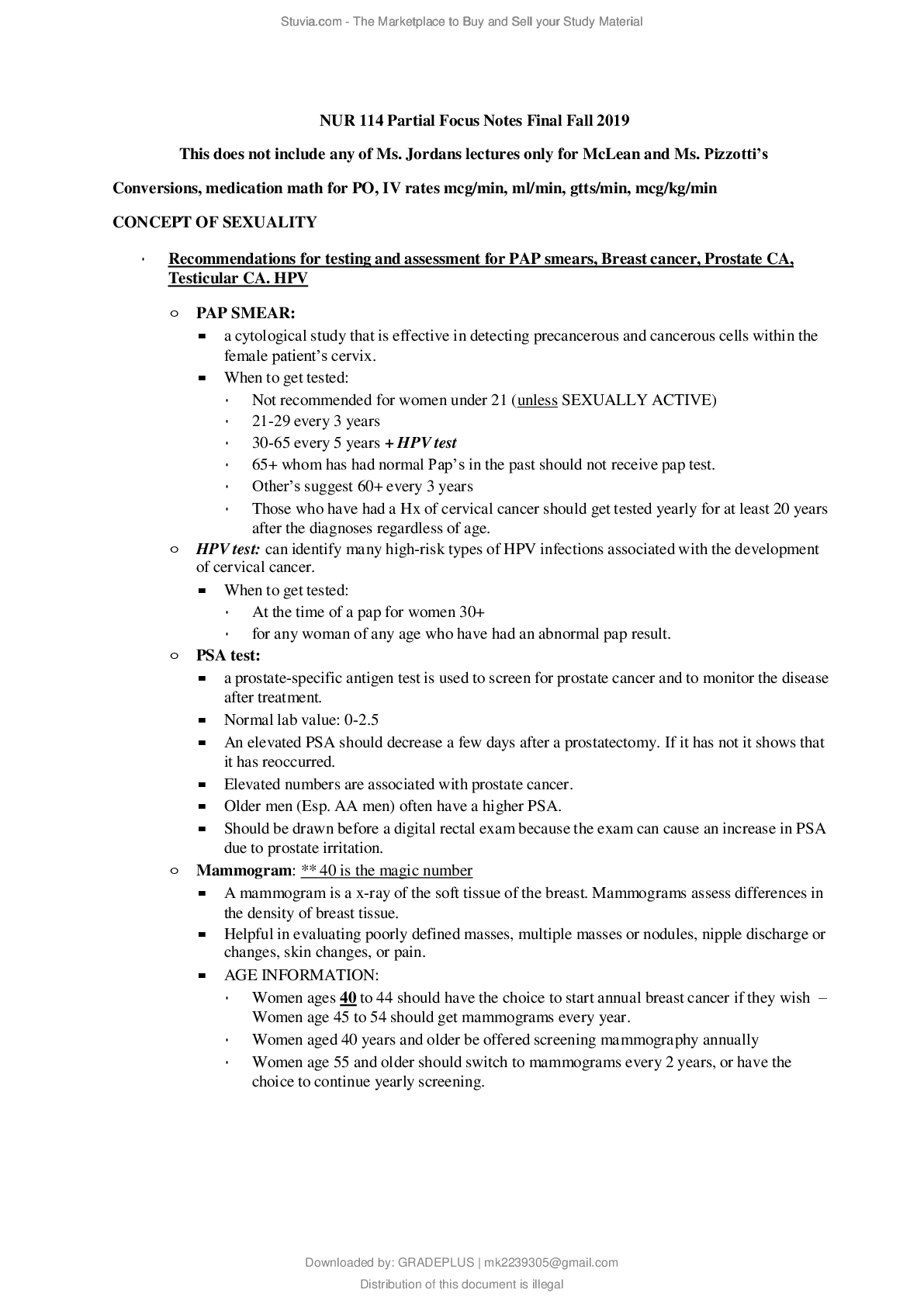
_removed.png)