*NURSING > Class Notes > NR 503 midterm study sheet (All)
NR 503 midterm study sheet
Document Content and Description Below
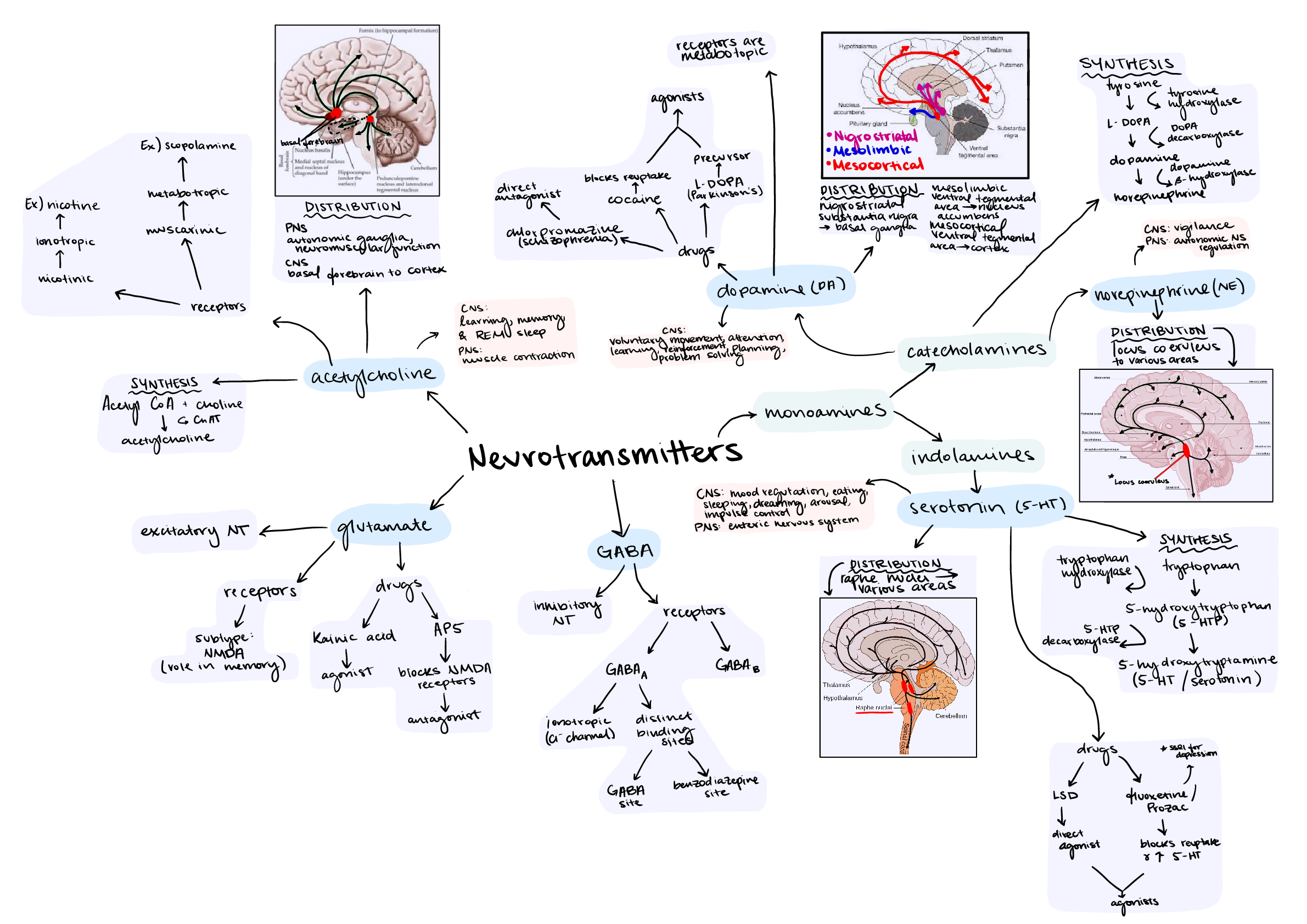
NR 503 midterm study sheet Pulmonary • Anticholinergics and tx for asthma, bronchitis and assoc pathogenesis o Anticholinergics block acetylcholine receptors for bronchoconstriction; thus: bronch... odilation Asthma: short acting counter to expose to trigger Bronchitis: short acting counter exacerbation of dyspnea and bronchoconstriction COPD: Short acting counter to exacerbation, o Epinephrine causes bronchodilation in ER: Beta-2 Adrenergic receptors • Bronchitis associated pathogenesis o Define: bronchial inflammation, hypersecretion mucus, chronic productive cough @ least 3 months in 2 straight years o Patho: ↑ mucus production d/t irritant → hypertrophy of bronchial smooth muscle → hypertrophy & hyperplasia of bronchial mucus producing cells → airway obstruction → ↓ alveolar ventilation • Chronic bronchitis A/B disturbances o Hypercapnia (↑ CO2 → Resp acidosis) • Perfusion o ↓ventilation = ↓perfusion • Blood flow between heart & lungs o Pulmonary Artery: takes deoxygenated blood from RV to Pulmonary capillary beds o Pulmonary Vein: takes oxygenated blood from Pulmonary capillary beds to LA. • Asthma S/Sx o Dyspnea, bronchoconstriction, ↓ventilation = ↓perfusion, • Bronchioles • Alveolar hyperinflation with asthma o Asthma sx: ↑ mucus production → ↑chance of mucus plug in combo with bronchoconstriction, air is trapped within alveolar (→barrel chest, CO2 retention) • Polycythemia vera – too many RBS, increased blood viscosity → systemic HTN Cardiovascular • Concepts of cardiac output • Cardiac contractility o Determined by Ca++ with actin-myosin • Preload/afterload o Preload: degree of myocardial stretch prior to contraction o Afterload: amt of tension ventricle must build up to open SL valves to eject bld • Systole/diastole o Systole: contraction of cardiac muscle and pushed fluid bolus o Diastole: filling of cardiac chamber with blood • Heart valves (open v/s closed during cycle, S1, S2) o S1: Atrioventricular valves close as atrium pushes remaining atrial vol into ventricles. SL open to allow diastole. o S2: Semi lunar valves close as LV and RV push systemic (aorta) & pulmonary (pulm a.) systems. AV open diastole. • Stenosis of heart valves and effects • Stroke volume • Cor pulmonale – right heart failure as a result of pulmonary congestion from LHF • Heart failure & physiologic processes that lead to HF sx o LHF process ↑systemic vascular pressure → ↑LV contraction force (↑afterload : ↑SVR) -overtime→ ↓LV EF→→ ↑LV preload (doesn’t empty) → ↓LA EF →↑LA preload →↑ pulm blod vol. & pressure →forces fluid into lung tissues (clin man: pulm edema, dyspnea, poss RHF & biventricular HF.) o RHF process ↑pulm vascular pressure → ↑RV contraction force (↑afterload: pulm htn) → ↓RV EF → ↑RA preload (backflow too) →↑vena cava z7 systemic venous vol. & P’ → forces fluid into pulm tissues (clin man: jugular distention, hepatosplenomegaly, peripheral edema →LHF = biventricular HF) o High output failure • HTN • Calcium binding and troponin – Ca++ unbinding allows for cardiac muscle relaxation … Hematology • Hematopoiesis – blood cell formation. Varying with age. Bone marrow by 5th month; long bones post 20yrsold. o 7 day cycle: Hemocytoblast + erythropoietin = proerythroblast -> early & late erythroblast -> normoblast (loses nucleus, ribosomes, mitochondria) -> reticulocyte -> erythrocyte o Kidney & liver stimulate growth factors for erythropoietin (EPO) production in response to hypoxia; androgens (testosterone) stimulate increased production *commonality of male dominated ??? anemia o Stimulated by infiltration of yellow marrow with Red marrow. • IDA – most prevalent (20%) o Insufficient Fe intake or inability of mitochondria to utilize • Erythrocyte function and lifespan – 100-120 days, tport oxygen to tissues, tport NO to lungs for exhalation, Vitamin C increases cellular resistance to bacteria & keep Ferrous from ferric(non-oxygen binding). Anaerobic ATP only, no nucleus, ribosomes, or mitochondria o Adult = 2 alpha + 2 beta; Ferrous, B12, folic acid are needed for structure o Tissue oxygenation • Erythropoietin – produced by the kidneys in response to hypoxia, • Functions of hemoglobin o Tport O2, nutrients to the tissues via binding with heme, o Tport NO & metabolic waste volatile acids to exhalation • Development of anemia due to gastrectomy -> pernicious anemia • Effects of being transfused with wrong blood type –> hemolytic anemia • Anemias Name Class Problem Cause Results in patho Aplastic anemia Normocytic-normochromic Decr cell number Exposure from: ATB, viral inf, chemical or radiation, tumors Destroys red bone marrow replaced with yellow marrow only Loss of blood cell producing areas (replaced with fat) Finally: Pancytopenia – cyanosis, blood clotting problems, WBC loss = incr infection. Hemolytic Normocytic-normochromic Lysis of premature RBC d/t toxins/enzymes produced by agent Infection, helminths, autoimmune, transfusion rxn, RH incompatible Megaloblastic Anemia Pernicious Macrocytic-normochromic – cell too large Malabsorption of B12 d/t decr Intrinsic factor (IF) production/ secretion Autosomal rxn, loss of GI cells to produce IF, Decr B12 yields decr DNA synth, decr RBC # & myelination, associated neuropathies Gastritis, gastrectomy Folate Deficiency Macrocytic-normochromic – cell too large Insufficient folate intake or decr absorption from diet d/t GI disease Malnutrition, alcoholism, anticonvulsant Rx Abnormal RBC formation, premature death of RBCs, Female in utero – hi risk neural tube defects Iron Deficiency Microcytic-hypochromic Insufficient Fe available Insufficient intake, chronic & or acute occult bleeding, transferrin deficiency or mitochondrial defects Decr Hb synthesis, decr size & pallor complexion Bleeding: 2-4ml/day = 1-2 mg Fe. 3 stages: S1: bodys Fe depleted. S2: Fe tport to bone marrow diminished, Fe-def erythropoiesis. S3: Hb def RBC enter circ for aged RBC affects seen S3. Sickle cell Hemoglobinopathies – autosomal recessive (both parents) Single A.A on beta chain “glutamic acid -> Valine” – elongated HbS Lack RBC O2 carrying ability on sickled cells, response to stress, anxiety, fear, cold, dehydration = poor O2 binding, incr sickling RBC premature death 10-15 days in circ, incr risk for Fe circ overload (rbc lysis 2 mg per), occlusion of bld vessels & spleen, incr risk CVA, splenic damage Sickle cell trait (only 1 parent gene) [adaptation to fight malaria] typically asymptomatic carrier. Thalassemia Hemoglobinopathies – autosomal recessive (both parents) Many genetic mutations at alpha or beta chain. Possible deletion Synthesis of Hb w/ abnormal or missing chains distorting & dysfunction of RBC Minor or major Cooley’s forms of disease: asymptomatic to lethal Genitourinary/ renal • A&P of kidney o Nephron functional unit Glomerulus • Filters Proximal Tubule • Reabsorption: Na(Major), glucose, K+, Amino acids, HCO3-, Phosphate, urea, H2O (ADH not req.) • Secretion: H+, foreign substances • Tonicity: isotonic Loop of Henle: concentrate urine • Descending: o Reabsorption: H2O, Na+ diffuses in o Tonicity: isotonic • Ascending o Reabsorption: Na+; water is taken away o Tonicity: hypertonic Distal tubule • Reabsorption: Na+, H20 (ADH req.!), HCO3- • Secretion: K+, Urea, H+, NH3, some drugs • Tonicity: hypotonic Collecting duct • Reabsorption: H2O • Secretion or absorb: Na+, K+, H+, NH3 • Final concentration for micturition • Nephron damage o Permanent, apart of the normal aging process At age 75 output ~85ml/min GFR; normal is 125ml/min o • Conditions assoc with renal failure o • Calculi blockage of ureter o Postrenal condition • Benign prostatic hypertrophy o Postrenal condition • Prerenal, Intrarenal, Postrenal disease and cause o Prerenal Renal hypoperfusion d/t hypotension w/ ↓CO or ↓bld vol. Patho: ↓renal bld flow →hypoperfusion → ↓GFR → ↑PCT Na H2O reaborp →↑aldosterone & ADH secretion → ↑DCT Na H2O reabsorp → oliguria o Intrarenal ATN, acute or other glomerulopathies Patho: Renal tubule injury → Cast formation → ↑intratubular Obs → ↑intratubular Pressure → Tubular back flow → ↓ GFR → oliguria o Postrenal UT obstruction Patho: Uni or bilateral obs → ↑ intraluminal Pressure → release of inflammatory mediators & vascular endothelial cell injury → renal vasoconstriction → cellular interstitial edema → ↓glomerular filtration pressure → oliguria • Glomerulonephritis o Patho: 1. trigger event → 2. Ag-Ab complex formation & deposition in glomerulus → 3. activate Complement syst. & WBC infiltration → 4. glomerular injury & leakage → 5-a. proteinuria/ hematuria 5-b. ↓ capillary perfusion + coag. Cascade activate & fibrin deposition. 5-c ↓GFR. 6. Clin man: edema, ↑Crt, azotemia, oliguria • Tx of renal failure • Blood hydrostatic pressure • Kidney filtration • Role of angiotensin converting enzyme (ACE) – angiotensin 1 to angiotensin 2 which ↑ bld vol and ↑ vasoconstriction to improve perfusion to the Kidneys. [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 15, 2021
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
May 15, 2021
Downloads
0
Views
49


.png)