*NURSING > QUESTIONS & ANSWERS > PANCE Practice Exam #2, All Questions and answers, 2022 update, questions bank, rated A+ (All)
PANCE Practice Exam #2, All Questions and answers, 2022 update, questions bank, rated A+
Document Content and Description Below
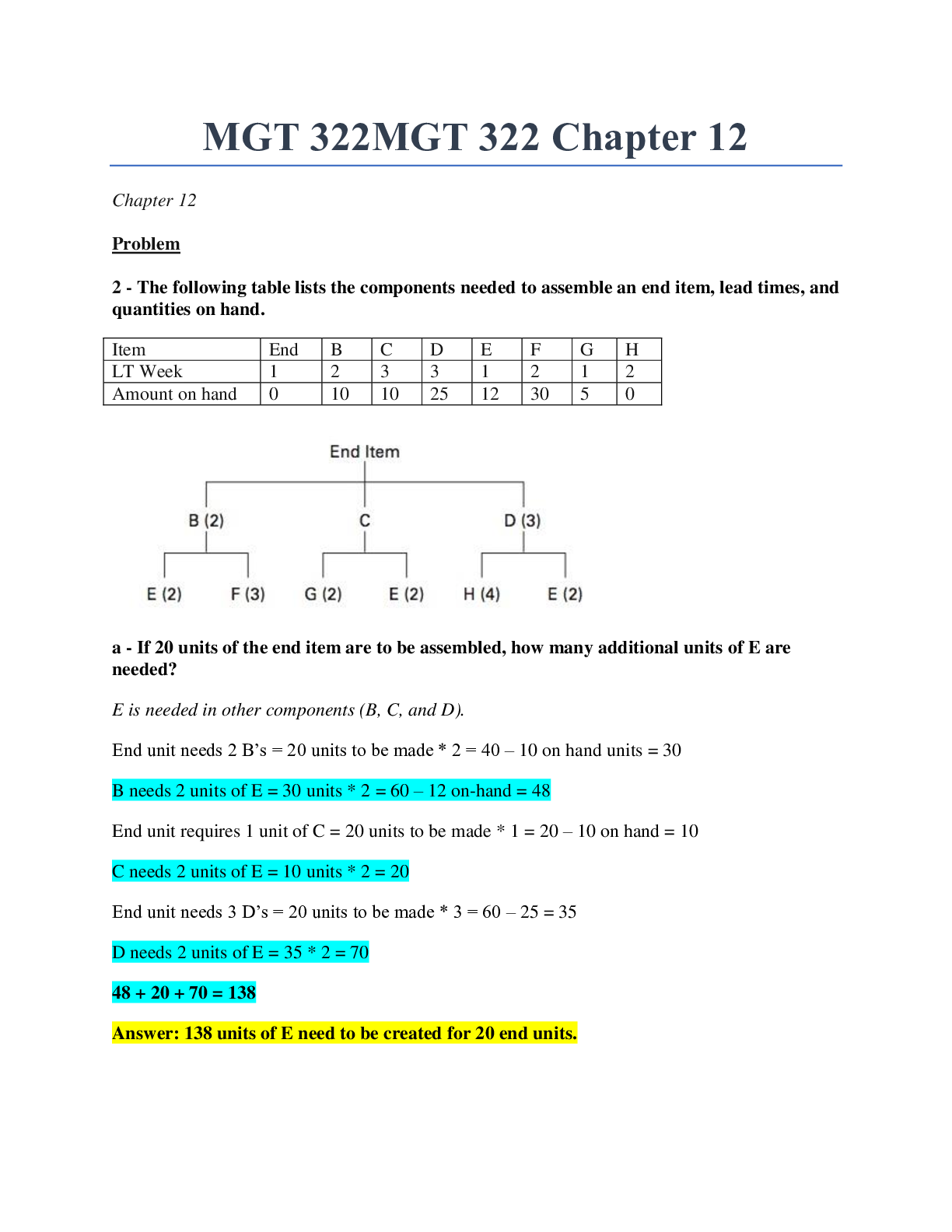
PANCE Practice Exam #2, All Questions and answers, 2022 update, questions bank, rated A+ You are treating a 20-year-old female with multiple aphthous ulcers. She complains of a moderate amount of... pain. You decide to prescribe "magic mouthwash" for the patient to swish and spit. Which of the following combinations of medicines is appropriate? - ✔✔A very commonly used combination of medicines to promote relief of discomfort and healing include liquid diphenhydramine, antacid, tetracycline, and 2% viscous xylocaine. A 17-year-old male is brought to your Emergency Department by his girlfriend. She states that he has been behaving strangely for the last three days, with rapidly fluctuating moods ranging from euphoric to irritable and paranoid. The patient states that he is fine, just a little nervous about an upcoming test in school. His pulse is 126 beats per minute, BP 182/106, pupils are widely dilated, and he is diaphoretic. What is his most likely diagnosis? A. Acute anxiety B. Bipolar disorder C. Cocaine intoxication D. Heroin intoxication - ✔✔he answer is C. EXPLANATION: This patient's presentation with tachycardia, hypertension, diaphoresis, and mydriasis along with the behavioral changes is consistent with cocaine intoxication cause somnolence and pinpoint pupils - ✔✔Heroin withdrawal A 67-year-old man presents with pain and stiffness in his shoulders and hips lasting for several weeks with no history of trauma. He also has complaints of headache, throat pain, and jaw claudication. It is imperative to diagnose this patient promptly in order to prevent which of the following complications? A. anemia B. cerebral aneurysms C. mononeuritis multiplex D. ischemic optic neuropathy E. respiratory tract complications - ✔✔The answer is D. EXPLANATION: The most urgent need for diagnosis of a patient with symptoms of polymyalgia rheumatica (PMR) and giant cell arteritis is to prevent blindness caused by ischemic optic neuropathy as a result of occlusive arteritis of the ophthalmic artery. Early diagnosis is imperative as the neurological damage to the optic nerve is not reversible. Most patients with this diagnosis will have a normochromic-normocytic anemia, but this does not create urgency in treatment. Cerebral aneurysms are not common findings with PMR; large vessels such as the subclavian and aorta may be involved in giant cell arthritis in 15% of patients. Mononeuritis multiplex commonly presents with painful paralysis of a shoulder, and respiratory tract complications are more nonclassic findings with the presentation of PMR. During an ophthalmoscopic exam you notice deep retinal microvascular hemorrhages, and cotton wool spots. What is the most likely cause of her visual disorder? - ✔✔The answer is D. Diabetic retinopathy-EXPLANATION: The patient's symptoms suggest a likelihood of diabetes. Retinal findings can include microaneurysms, deep hemorrhages, a flame-shaped hemorrhage, exudates, and cotton wool spots. A newborn male is diagnosed with Christmas factor deficiency. What is the likelihood that he inherited this disorder from his father? A. 0% B. 25% C. 50% - ✔✔The answer is A. EXPLANATION: All daughters of a hemophilic male are carriers of hemophilia, whereas all sons are normal. Hemophilia B (or Christmas factor deficiency) is one of only two sex-linked pattern-bleeding disorders, and as such the disease occurs almost exclusively in males. Sons of carriers have a 50% chance of being affected and daughters of carriers have a 50% chance of being carriers themselves. A 2-month-old female presents for a well child check. The mother has no concerns and feels that the child is doing well. On exam, there is no evidence of cyanosis and the peripheral pulses are normal and equal. However, there is a fixed and widely split S2, a right ventricular heave, and a systolic ejection murmur present. The murmur is heard best at the left sternal border second intercostal space. What is the most common abnormality present on an ECG? A. Atrioventricular heart block B. Atrial fibrillation C. Bifasicular block D. Right axis deviation - ✔✔The answer is D. EXPLANATION: The most likely diagnosis is an atrial septal defect, which usually shows right axis deviation on ECG. The other ECG abnormalities listed do not commonly occur with an atrial septal defect. A 28-year-old male smoker presents witha complaint of numbness and pain in his fingers. He notices thisafter being exposed to the cold. He states that his fingers appearpale or even blue at times. After warming, his fingers turn redbefore returning to their normal color. What should be includedin appropriate management of this condition? A. Counsel the patient to stop smoking B. Systemic glucocorticoids C. Take aspirin prior to cold exposure - ✔✔The answer is A. EXPLANATION: This patient is experiencing Raynaud phenomenon. This is digitalischemia that can occur after exposure to cold or emotional stress. It is more common in smokers or patients whose occupation involvesusing vibratory tools. Management includes patient education toinclude cold avoidance behavior and wearing loose-fitting clothing.Cessation of smoking is imperative. Drug therapy is used in patientswith progressive and severe Raynaud's. A 45-year-old woman presents with weight gain, fatigue, dry skin, constipation, and oligomenorrhea. On physical exam, bradycardia and slow deep tendon reflexes are noted. Her free T4 is low and TSH is elevated. Which of the following medications may be responsible for her condition? A. amiodarone B. beta-blockers C. levadopa - ✔✔The answer is A. EXPLANATION: Hypothyroidism is reported in up to 10% of patients taking amiodarone, an antiarrhythmic medication. With the high iodine content of the medication and the structural similarities to thyroxine, thyroid abnormalities occur. Common side effects of amiodarone include bradycardia and constipation, so laboratory evaluation for thyroid dysfunction must be used. Common side effects of amiodarone - ✔✔include bradycardia and constipation, so laboratory evaluation for thyroid dysfunction must be used. A 3-week-old male infant is brought in by his mother due to his vomiting. The mother notes that a few days ago her son started vomiting after feeding, and it has become projectile in nature. The vomitus is non-bilious and contains no blood. The child seems hungry and nurses regularly, but the vomiting has become more frequent and is occurring with every feeding now. On physical examination, an oval mass is palpated in the right upper quadrant. Appropriate imaging is obtained and confirms the suspected diagnosis. What is the treatment of choice in this patient? A. Acid supression B. Dilatation of the lower esophageal sphincter C. Diverting colostomy D. Ladd procedure E. Pyloromyotomy - ✔✔The answer is E. EXPLANATION: A pyloromyotomy involves an incision along the length of the pylorus, down to the mucosa, and is the treatment of choice in pyloric stenosis. Acid suppression is the treatment of choice in cases of peptic ulcer disease. Dilatation of the LES is performed in cases of achalasia of the esophagus. A diverting colostomy may be used in cases of Hirschsprung disease, after removal of the aganglionic section of colon. The Ladd procedure is used in surgical treatment of intestinal malrotation. The rotator cuff is comprised of which four muscles? - ✔✔Supraspinatus, infraspinatus, teres minor, subscapularis The patient has a family history of thyroid cancer. You are concerned that the patient may have medullary thyroid cancer. Which of the following lab tests would you monitor in this patient after treatment? - ✔✔serum calcitonin. Both calcitonin and CEA are secreted by medullary thyroid cancer cells, and are used both in diagnosis and monitoring of patients after treatment. Alkaline phosphatase, is elevated in disorders of the - ✔✔bone and biliary tract. serum anti-thyroglobulin antibodies, are most commonly associated with - ✔✔autoimmune disorders of the thyroid, such as Hashimoto's thyroiditis. Serum CA-125 has been used to investigate and follow patients with malignancies, such as? - ✔✔ovarian cancer A 76 year-old woman with steroid dependent chronic obstructive pulmonary disease is hospitalized with fever, chills, and a productive cough. The sputum gram stain shows many WBCs and small, pleomorphic gram-negative rods. Which of the following is the most likely causative agent? A. Chlamydia pneumoniae B. Haemophilus influenzae C. Mycoplasma pneumoniae - ✔✔The answer is B. EXPLANATION: Haemophilus influenzae (B) is a gram-negative pleomorphic coccobacillus. Strep pneumonia (E) and Staph aureus (D) are gram positive organisms. Mycoplasma pneumonia (C) and Chlamydia pneumoniae (A) aren't visible on gram stain. An 8-month-old baby boy is brought in by his mother after noticing redness and swelling around his penis, which she retracted his foreskin to clean after a diaper change. She states the swelling has been increasing over the past 2 hours. His past medical history is unremarkable and he is uncircumcised. On physical examination you see the following: Considering your suspected diagnosis, what would be the management of this patient? A. Observation until the swelling decreases B. Attempt manual reduction and get emergent urologic consultation C. IV fluids and analgesics D. Dorsal penile nerve block with lidocaine and epinephrine - ✔✔he answer is B. EXPLANATION: Paraphimosis occurs when a tight ring of foreskin is retracted proximal to the glans of the penis and becomes trapped in the retracted position. Impaired venous and lymphatic draining can cause swelling and is a true urologic emergency. Immediate attempt with manual reduction should be done and if unsuccessful an emergent surgical consult with urology is appropriate (B). If paraphimosis is not quickly reduced the arterial blood flow can become compromised leading to glans necrosis. Observation would increase the risk for necrosis (A). Manual reduction should be attempted immediately with or without a dorsal penile nerve block. If not reduced promptly then an emergent urologic surgical consult should be made. If a nerve block (D) is given it should be without epinephrine. IV fluids and analgesics (C) are used for sickle cell patients with priapism. What age group is most at risk to develop osteoid osteoma? A. Adolescents B. Elderly C. Middle-aged - ✔✔The answer is A. EXPLANATION: Osteoid osteoma is a benign bone forming tumor that usually develops during a patient's second decade of life. This type of tumor is much more common in boys than girls and typically affects the lower extremities (femur and tibia primarily) and spine more than other areas of the body. Patients typically present with gradually progressive bone pain that is worse at night and does not correlate with activity level. The tumor produces high levels of prostaglandins, so symptoms usually improve in 20-25 minutes if the patient takes a medication like ibuprofen, ASA or other NSAIDS that are prostaglandin inhibitors. A lack of improvement in symptoms with these medications should lead health care providers to consider a different diagnosis. The pain of this condition may cause those afflicted in a leg to limp and have swelling, muscle atrophy or contractures and exquisite point tenderness. The condition usually resolves on its own over time, but symptomatic patients may require surgical resection or radioablation of the tumor. A 29-year-old woman comes to the office because she "just keeps gaining weight and can't stop." Since she was last seen in the office at age 24, she has gained nearly 100#. Physical examination is remarkable for blood pressure of 140/92. She appears depressed. Her trunk and abdomen are heavy with normal-sized extremities. Her facial hair is dark and in a "male" distribution. Large dark violaceous striae are present on her abdomen and proximal extremities. Which of the following additional findings is most consistent with this presentation? A. Buffalo hump B. Doughy, thickened skin C. Exophthalmos - ✔✔The answer is A. EXPLANATION: This woman appears to have Cushing Syndrome (hypercortisolism) which is characterized, in addition to the signs listed above, by plethoric facies, supraclavicular fatpads, and the so-called "buffalo hump." Doughy, thickened skin (B) and thickened tongue (E) may be found in hypothyroidism, exophthalmos (C) in Graves disease, and lid lag (D) in hyperthyroidism from any cause. A 30-year-old female presents to your office for a routine physical exam. She has not seen a health care provider in many years. Upon talking with the patient, you find out that she had been diagnosed with hypertension several years ago, but was unable to afford the antihypertensive medications that were prescribed to her. She has no complaints at this time. Upon exam of the head and neck, you note widened spaces between her lower incisor teeth and a large, fleshy nose. Her skin is oily and she demonstrates mild proximal muscle weakness. Her EKG reveals a left axis deviation and widened QRS. What is the most likely rationale for her clinical presentation? A. Diabetes mellitus B. Cushing's syndrome C. Hypothyroidism D. Acromegaly - ✔✔The answer is D. The correct choice is D, acromegaly. Patients with acromegaly have an abundance of growth hormone secretion. This leads to excessive growth of many areas of the body including soft tissue. Patients with acromegaly also have an increased incidence of hypertension and left ventricular hypertrophy. None of the other choices will cause this patient's constellation of symptoms. Patients with many endocrine disorders may develop weaknesses as seen in this patient, but the large nose and widely spaced teeth are characteristic of acromegaly. A 41-year-old alcoholic male, who lives primarily on the streets, appears pale, cachectic, and mildly icteric. He is complaining of several weeks of increasing fatigue. Laboratory findings note an elevated MCV of 128. What other physical finding would most support the diagnosis for megaloblastic anemia? A. Decreased vibration and position sense B. Dementia C. Difficulty with balance D. Glossitis E. Parethesias - ✔✔The answer is D. EXPLANATION: Features of folate deficiency are similar to vitamin B12 deficiency. However, there are none of the neurologic abnormalities associated with vitamin B12. Glossitis is the only non-neurologic finding in the PE that would support folate deficiency. Alcoholism and poor dietary intake also support the diagnosis of folate deficiency. A 35-year-old male presents complaining of increasingly constant headaches, double vision centrally, and a progressive loss of peripheral vision for two weeks. He has no previous headache history and denies any other medical conditions. Physical examination reveals bitemporal hemianopsia without additional neurologic findings. What is the most likely diagnosis? A. Acute ischemic stroke B. Circle of Willis ruptured aneurysm C. Migraine headache D. Multiple sclerosis E. Pituitary adenoma - ✔✔The answer is E. EXPLANATION: Pituitary adenomas, benign neoplasms associated with pituitary hormone secretory changes, may enlarge and become symptomatic. Symptoms are based upon the location and size of the tumor, and may include bitemporal hemianopsia, double vision, color desaturation, and visual acuity loss. Headaches may occur, due to associated pressure changes within the intrasellar space. Additional evaluation should include a T1-weighted MRI, screening laboratory tests, and a full ophthalmologic evaluation. These tests will also help evaluate for potential differential diagnoses, such as those listed. The patient's history is not consistent with an acute ischemic stroke or migraine headache. Although an unruptured aneurysm may have very similar findings to a pituitary tumor, ruptured aneurysms present with acute headache, nausea, vomiting, and potential changes in consciousness. Multiple sclerosis (MS) should remain on the differential for this patient and will also be evaluated through MRI (although the current findings are more consistent with a pituitary adenoma), and additional neurologic findings would be likely with MS. Which of the following pulmonary function test results demonstrates emphysema, a form of obstructive pulmonary dysfunction? - ✔✔Total lung capacity represents the vital capacity, defined as the amount of gas exhaled after a maximal inhalation, plus the residual volume within the lung after maximum exhalation. With emphysema, the lung parenchymal damage and decreased elasticity results in all flow rates being reduced, including FEV1, FVC, and FEV1/FVC levels. Expiratory time is increased and gas trapping occurs, thus increasing the total lung capacity. A soft tissue neck x-ray of a patient who complains of a progressively worsening sore throat reveals this lateral film (see image). Based on these findings, what is the initial treatment of choice for this patient? pic-thumbprint sign A. Endotracheal intubation B. Intravenous steroids C. Ribovirin injection D. Incision and drainage - ✔✔The answer is B. EXPLANATION: This case of acute epiglottitis is treated with immediate intravenous steroids. Provided that the patient is able to maintain the airway and also keep oxygen saturation rates above 92%, the patient can improve with steroids and supportive care. Antiviral medications have little effect on the overall illness. You decide to treat him with a proton pump inhibitor at this visit, and he achieves good symptomatic relief with this therapy. What length of therapy is appropriate in this patient? - ✔✔If a patient achieves good symptomatic relief with a course of an empiric, once-daily proton pump inhibitor, therapy may be discontinued after eight to twelve weeks. A 6-week-old male with sickle cell disease presents to the pediatric office for his well-child visit. When should this child begin taking daily prophylactic penicillin? - ✔✔2months-Patients with sickle cell disease develop functional asplenia as early as 3 months of age and should begin treatment with prophylactic penicillin at 2 months of age to prevent infection by encapsulated organisms (i.e., pneumococcus). Which of the following sets of disorders is commonly found in multiple endocrine neoplasia (MEN) 2A? - ✔✔The three primary features of MEN type 2A include medullary thyroid carcinoma, parathyroid hyperplasia or adenoma, and pheochromocytoma. pheochromocytoma, medullary thyroid carcinoma, and mucosal neuroma are disorders found in - ✔✔MEN 2B parathyroid adenoma, islet cell hyperplasia, and pituitary adenoma are found in - ✔✔MEN I Your patient is a 66-year-old female who has been dropping her coffee cup and concurrently slurring her speech. The episodes last for approximately 15 minutes. Her blood work, carotid dopplers, and MRI of the brain are normal and you suspect recurrent transient ischemic attacks (TIAs). Which of the following is NOT approved or recommended for the prevention of stroke in this patient? A. aspirin B. extended-release dipyridamole plus aspirin C. clopidogrel D. prasugrel E. warfarin - ✔✔The answer is E. EXPLANATION: Aspirin, aspirin plus extended-release dipyridamole, and clopidogrel are all antiplatelet agents and approved for use to reduce recurrent TIAs and ischemic cerebrovascular accidents (CVAs). Prasugrel is not FDA-approved for this indication. Warfarin is an anticoagulant and has no role in prevention of either recurrent TIA or ischemic CVA. Initial Treatment in TIA - ✔✔Aspirin A 73-year-old female with type 2 diabetes, hypertension, and hyperlipidemia presents to the emergency department complaining of left ear pain, and a yellowish-green, foul-smelling discharge that began about 3 weeks ago. On physical examination, the patient is afebrile and examination reveals a markedly edematous left ear canal draining purulent, green discharge. The tympanic membrane is unable to be visualized. Upon cranial nerve exam the patient has left-sided facial weakness. Which of the following diagnostic studies should be performed first in the initial evaluation of this patient? A. CT scan of the head B. Culture and sensitivity C. Hemoglobin A1C D. HSV-1 antibody testing E. MRI of the brain - ✔✔The answer is A. EXPLANATION: The patient has malignant otitis externa that has most likely extended to osteomyelitis and impingement of the facial nerve. Emergent CT scan (A) is indicated over MRI (E) to assess the extent of disease and the presence of osteomyelitis. Malignant otitis externa is most commonly caused by pseudomonas and empirical antibiotic therapy can be initiated prior to culture and sensitivity (B). Assessment of the patient's diabetes control (C) should occur, but isn't the highest priority study to order first. HSV-1 antibody testing (D) is not indicated in this patient. A 12-year-old female presents with linearlydistributed light brown papules on her arm. They are asymptomaticand have been present for several years. The mother states that theyappear to grow as the child grows. What treatment is necessary? A. Cryotherapy B. Laser ablation C. No treatment is necessary - ✔✔The answer is C. EXPLANATION: This condition is consistent with a linear epidermal nevus. Theycan appear at any age, but are usually present at or shortly afterbirth. The pigmented papules are arranged linearly and can occuron any skin surface. They are not symptomatic and will grow withthe child. There is no treatment necessary. A 24-year-old male has an eight-month history of loose thought associations, social withdrawal, auditory hallucinations, and deterioration in his personal appearance and hygiene. Upon examination, he is noted to have a flat affect, perceptual distortions, and behaves like he is detached from his own actions. If chosen for treatment, which of the following medications would require weekly white blood cell count monitoring for the first six months? A. Clozapine (Clozaril) B. Haloperidol (Haldol) C. Olanzapine (Zyprexa) D. Risperidone (Risperdal) - ✔✔The answer is A. EXPLANATION: Clozapine has a risk of agranulocytosis. While the risk is only 1%, weekly monitoring of the white blood cell count for the first six months, followed by monitoring of the white blood cell count every other week thereafter, is required. The other medications listed do not have the risk of agranulocytosis. An 18-year-old female presents to your office with the complaint of palpitations for the last 2 months. The episodes are frequent and accompanied with lightheadedness and shortness of breath. The patient's mother has taken her pulse when some of the episodes occur and states that the rate gets as high as 170 beats per minute. On exam, she is alert, awake, and oriented. Her resting pulse is 55 and her blood pressure is 122/65. Her lungs are clear throughout, and her cardiac exam revealed a regular rate and rhythm, without murmurs, rubs, or gallops. An ECG is obtained, as shown. Based on her history, physical exam, and ECG, what is the best pharmacologic treatment plan for this patient? A. Flecanide B. Hydrochlorothiazide C. Lisinopril D. Adenosine - ✔✔The answer is A. EXPLANATION: This patient is presenting with Wolff-Parkinson-White syndrome, as evidenced by the delta waves on the ECG. These conditions will generally occur in individuals at the onset of early adulthood. Management for this condition pharmacologically includes the use of class IC drugs, such as flecanide. Other choices include procainamide, sotalol, and amiodarone. Digoxin therapy may worsen and widen the QRS complex and place the patient into a ventricular tachycardia. Which of the following would raise your suspicions the most and likely warrant consideration of testing for an inherited thrombophilia? A. a deep femoral vein deep vein thrombosis (DVT) after a flight from Mumbai, India B. an iliac vein DVT after a round trip bus trip to Atlantic City and playing slots all day C. any DVT after a total knee replacement D. an upper extremity DVT after tripping falling down a flight of stairs - ✔✔The answer is D. EXPLANATION: DVTs most commonly arise from the deep femoral veins and iliac arteries, most commonly in patients who smoke and take oral contraceptives, after immobilizing surgeries, and/or after immobilization due to long periods of time seated, including but not limited to airplane flights, bus rides, etc. Upper extremity DVTs are rare, even after trauma, and warrant a hypercoaguability work-up to rule out inherited disease. Which of the following is the most common cause of hypoparathyroidism? A. Familial hypoparathyroidism B. Idiopathic hypoparathyroidism C. Severe magnesium depletion D. Surgical removal of the parathyroid - ✔✔The answer is D. Choice D, surgical removal of the parathyroid glands, is the correct answer. Surgery for head and neck cancer, thyroidectomy, and parathyroidectomy are the most common causes of hypoparathyroidism. Choices A, B, C, and E are all causes of hypoparathyroidism that occur more infrequently. A 45-year-old woman with recent diagnosis of rheumatoid arthritis has begun treatment with celecoxib. She has been on this medication for 3 months and notes that her pain continues. Early signs of joint involvement are present in the patient's hands. Which of the following medications is the most appropriate to add to her treatment? A. aspirin B. rituximab C. etanercept D. leflunomide E. methotrexate - ✔✔The answer is E. EXPLANATION: The treatment of rheumatoid arthritis (RA) is aimed at reduction of pain, preservation of function, and prevention of deformity. Although non-steroidal anti-inflammatory drugs (NSAIDs) provide symptomatic relief, they do not alter progression or prevent erosion of the joint. Consequently, in addition to NSAID therapy, disease-modifying anti-rheumatological drugs (DMARDs) should also be initiated as soon as the diagnosis is confirmed. The most common initial DMARD used as treatment of choice in RA is methotrexate. Aspirin should not be added because of the increased risk of gastrointestinal side effects as well as having no effect on altering RA disease progression. Rituximab is a biological DMARD and is indicated to be added in patients with RA refractive to treatment with combination therapy of methotrexate and a tumor necrosis factor inhibitor (TNF). Etanercept is a TNF inhibitor. This class of medication is often added in patients with RA who are not responding to methotrexate therapy alone. Leflunomide is a pyrimidine synthesis inhibitor that is approved for the treatment of RA; however, it is contraindicated for use in premenopausal women secondary to its carcinogenic and teratogenic potential A 38 year-old woman with severe-persistent asthma presents to the clinic complaining of nightly nighttime awakens and frequent use of her inhaled albuterol. Which of the following is an antibody that prevents IgE from binding to its receptor on mast cells and basophils and may be considered as a treatment for this patient? A. adlimumab B. daclizumab C. etanercept D. infliximab E. omalizumab - ✔✔The answer is E. EXPLANATION: Omalizumab (E), is an antibody that prevents IgE from binding to its receptor on mast cells and is used in the treatment of allergic disease. Daclizumab (B) is anti-IL-2 antibody used to prevent acute rejection of organ transplants. Adlimumab (A), etanercept (C), and infliximab (D) bind TNF, thus inhibiting the action of TNF and are used in the treatment of disorders such as psoriasis and rheumatoid arthritis. You are evaluating an 80-year-old female for the first time. She has a history of mild Alzheimer's disease, for which she takes Aricept. She states that she feels fine but her daughter feels she is depressed and has been complaining of not feeling well. Her daughter admits that the patient has a history of primary hyperparathyroidism. What laboratory results would be most consistent with her diagnosis of hyperparathyroidism? A. high serum calcium B. low intact PTH C. low cortisol - ✔✔The answer is A. EXPLANATION: The correct answer is (A). The hallmark of primary hyperparathyroidism is a high serum calcium and high intact PTH. A low intact PTH is consistent with hypoparathyroidism. The urine serum calcium is usually high in primary hyperparathyroidism. Cortisol is related to endocrine conditions affecting the adrenal cortex. A 27-year-old man presents to the emergency department with a five-day complaint of substernal pleuritic chest pain, which worsens while lying supine. He is in no distress. A friction rub is noted over the precordium. The patient's vital signs are as follows: temperature is 100.4°F, pulse rate is 94, respiratory rate is 20, and blood pressure is 136/84. An ECG reveals widespread diffuse ST elevations with PR interval depressions. He was recently treated for a viral respiratory infection. Which of the following is the most appropriate initial management for this patient? A. Administer a broad spectrum antibiotic B. Administer intravenous tissue plasminogen activator (T-PA) C. Begin a nonsteroidal anti-inflammatory agent - ✔✔The answer is C. EXPLANATION: This patient's diagnosis is acute inflammatory pericarditis. Viral infections are the most common cause of acute pericarditis, and males are the most commonly affected. A pericardial friction rub and EKG changes are characteristic of this diagnosis. Treatment is focused on the underlying inflammation, with NSAIDS being first-line and short course corticosteroids also being appropriate. Antibiotics are not indicated unless a bacterial etiology is confirmed or there are significant risk factors. Choices B, D, and E are not appropriate for this condition and could be harmful. A 24-year-old male with thalassemia major who has received adequate transfusions, chelation therapy, and regular health checkups is in to establish care. He is 5'4" with a BMI of 17. He eats a balanced healthy diet and gets regular exercise. You know that there are complications of this disease. What is the best next step for this patient? A. Increase threshold for blood transfusions B. Maintain sustained reduction of body iron C. Obtain a Dexa scan for osteoporosis - ✔✔The answer is B. Maintaining sustained reductions in body iron has demonstrated increased overall survival rates through reductions in cardiac disease specifically due to siderosis. While these patients are at increased risk for osteoporosis and cardiac siderosis, the next best step in this patient is to maintain reduced iron levels. There is no place for increased blood transfusion or obtaining regular testosterone levels. Which of the following joints has the lowest occurrence rate of osteoarthritis? A. Elbows B. Hands C. Hips - ✔✔he answer is A. EXPLANATION: Because the elbow is not a weight bearing bone, the rate of osteoarthritis in the elbow is considerably less that what is found in locations like the hips, knees and spine. The hands have one of the highest rates of occurrence of osteoarthritis, likely due to their near constant use and propensity for minor (or major) injury. When elbow arthritis does develop it is often post-traumatic osteoarthritis related to a significant injury in the past that disrupted joint surface integrity or as a result of rheumatoid arthritis, a systemic illness. Osteoarthritis of the elbow will generally present with pain, stiffness, and decreased range of motion. Osteophytes that form on the medial elbow might be implicated should neurological symptoms develop that correlate with ulnar nerve distribution as this nerve does pass in close proximity to the elbow on the medial side. A woman who is pregnant suffered a spontaneous abortion at 12 weeks gestation. She is now a G2P1Ab1 and is Rh negative. When should she receive her next Rhogam (Rho D immune globulin) shot? A. Now B. In one month C. At conception of her next pregnancy - ✔✔The answer is A. EXPLANATION: Placental implantation occurred and separated with the spontaneous miscarriage. Therefore, there is a slight chance of isoimmunization, so Rhogam should be given now so that the mother does not develop antigens that can cross the placenta during the first half of the next pregnancy. It is September and the radio is flooded with public service announcements recommending people get their flu shots early; flu is not yet endemic. Your patient, an 18 year old female, has come to see you in your family practice clinic with complaints of "flu-like" symptoms. She hoped the symptoms would resolve on their own, but it is now a week later and she is still experiencing them, and requests a rapid flu test. Which of the following is true regarding your patient and the rapid influenza tests? A. It is best she waits at least a week before having you perform a rapid test, since a false negative may result if seen too soon from onset of symptoms. B. You may warn your patient that given this time of year, the low prevalence in the community, and her delay in testing, the results are virtually useless and you would not recommend testing. - ✔✔The answer is B. EXPLANATION: The rapid tests vary in terms of sensitivity and specificity. Research indicates that sensitivities are approximately 50% to 70%, while specificities are approximately 90% to 95%. Specimens to be used with rapid tests generally should be collected as close as is possible to the start of symptoms and usually no more than four to five days later in adults. In very young children, influenza viruses can be shed for longer periods; therefore, in some instances, testing for a few days after this period may still be useful. Most importantly, the positive and negative predictive values vary considerably depending upon the prevalence of influenza in the community. False-positive (and true-negative) influenza test results are more likely to occur when disease prevalence is low, which is generally at the beginning and end of the influenza season, as is the case here. False-negative (and true-positive) influenza test results are more likely to occur when disease prevalence is high, which is typically at the height of the influenza season. When disease prevalence is relatively low, the positive predictive value (PPV) is low and false-positive test results are more likely. By contrast, when disease prevalence is low, the negative predictive value (NPV) is high, and negative results are more likely to be true. A 25-year-old female presents with a complaint of dry, stinging hands for the past two months. She has never had any rashes or similar problems. She does not work. The patient stays home to care for her six-month-old baby. She has tried treating her hands with over-the-counter lotions, but reports that they sting upon application. What should appropriate management of this condition include? A. triamcinolone 0.025% ointment bid, moisturize with petrolatum frequently, use gloves when hands in water B. withhold all treatments for one week and have patient undergo patch testing to determine allergen C. punch biopsy at periphery of outbreak, and treat with ketoconazole cream for two weeks - ✔✔The answer is A. EXPLANATION: The patient is experiencing an irritant contact dermatitis, secondary to having her hands in water frequently and using diaper wipes, which can be very irritating due to the alcohol content. The appropriate treatment would consist of reducing the irritant (water and wipes) by using barrier protection (gloves). A mid-potency topical steroid, such as triamcinolone 0.025% ointment twice daily, until the irritation has improved is appropriate treatment. Petrolatum and petrolatum based emollients are best for frequent moisturization. The history given is classic for irritant dermatitis, and withholding treatment for one week along with patch testing is not necessary, unless the patient does not respond to conservative therapy. A biopsy is not indicated, as this is classic irritant dermatitis. Ketoconazole cream is an antifungal medications and bactroban is a topical antibiotic. This patient presentation is not typical for a fungal infection, and should not be treated with an antifungal unless a positive KOH or fungal culture has been done. The bactroban ointment can help prevent a secondary bacterial infection if fissures are present. Upon funduscopic exam, you note marked hemorrhages in all quadrants and disc edema. The contralateral eye shows only mild hypertensive vascular changes. What is your diagnosis? A. Macular degeneration B. Retinal detachment C. Central retinal artery occlusion D. Cerebrovascular accident E. Central retinal vein occlusion - ✔✔The answer is E. EXPLANATION: A central retinal vein occlusion is characterized by a "blood and thunder" fundus, with marked hemorrhages, tortuous vessels, and optic disc edema. Which of the following medications is most likely to result in her blood pressure being elevated? A. loratadine B. simvastatin C. pseudoephedrine D. acetaminophen E. lisinopril - ✔✔The answer is C. EXPLANATION: The correct answer is (B). Decongestants, such as pseudoephedrine, are known to increase blood pressure. Discontinuing pseudoephedrine and rechecking the blood pressure off of this medication may provide further information on the need for additional antihypertensive drug therapy. Loratadine, simvastatin, and acetaminophen are not known to cause secondary hypertension. Lisinopril is an ACE inhibitor used to treat blood pressure. A 50-year-old male states that his eye is bothering him since yesterday. He complains of pain and redness. He states that he mowed his lawn yesterday and that it was windy outside. He attempted to irrigate the eye but still has significant irritation. He notes that it hurts to blink his eyes. What is the correct sequence of steps to treat this condition? A. Anesthetic drops, irrigate the eye, and perform tonometry B. Prescribe antibiotic cream and pain medication C. Fluorescein stain, irrigate the eye, and prescribe antibiotic cream D. Fluorescein stain and lid eversion E. Anesthetic drops, fluorescein stain, and lid eversion - ✔✔The answer is E. EXPLANATION: The history suggests a retained foreign body to the upper eyelid. A fluorescein stain will reveal significant superficial vertical scratches on the cornea. An upper eyelid eversion must be done, to inspect for and remove the foreign body. If the practitioner is successful in removing the foreign body, relief of the irritation will be immediate. A 40-year-old female presents to your office with symptoms of weight gain, hirsuitism, and easy bruising. Past medical and surgical history is noncontributory. She drinks one glass of wine on weekends and does not smoke cigarettes. She takes one multivitamin daily. Upon physical exam, you note facial fullness, central obesity, and thin skin. Which of the following is a valuable biochemical screening test for this patient that will aide in the diagnosis? A. Dexamethasone suppression test B. Radioactive iodine uptake C. Glucose tolerance test D. Cosyntropin stimulating test - ✔✔The answer is A. The correct choice is A, dexamethasone suppression test. This patient is presenting with classic signs and symptoms of Cushing's syndrome. The dexamethasone suppression test is a simple test of the hypothalamic-pituitary-adrenal axis, and requires ingestion of oral dexamethasone at nighttime and a blood test in the morning hour, to measure the amount of plasma cortisol. Most patients with Cushing's syndrome demonstrate a lack of normal axis suppression and present with a morning plasma cortisol level >5 mcg/dL. Choice B, radioactive iodine uptake, is used in patients with suspected thyroid disorders. Choice C, glucose tolerance test, is used in patients with suspected diabetes mellitus and in prenatal testing, to investigate gestational diabetes. Choice D, cosyntropin stimulating test, is used to investigate possible adrenal insufficiency. Choice E, plasma fractionated free metanephrines, is used in the diagnostic workup of pheochromocytoma. [Show More]
Last updated: 1 year ago
Preview 1 out of 100 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Also available in bundle (1)

PANCE EXAM BUNDLE,
ALL YOU NEED TO PASS THE PANCE EXAM, DOWNLOAD TO SCORE HIGH
By bundleHub Solution guider 1 year ago
$38
11
Reviews( 0 )
$12.00
Document information
Connected school, study & course
About the document
Uploaded On
Aug 20, 2022
Number of pages
100
Written in
Additional information
This document has been written for:
Uploaded
Aug 20, 2022
Downloads
0
Views
102


.png)