West Coast University: NURS 100 Ati funds Dosage Calculation,100% CORRECT
Document Content and Description Below
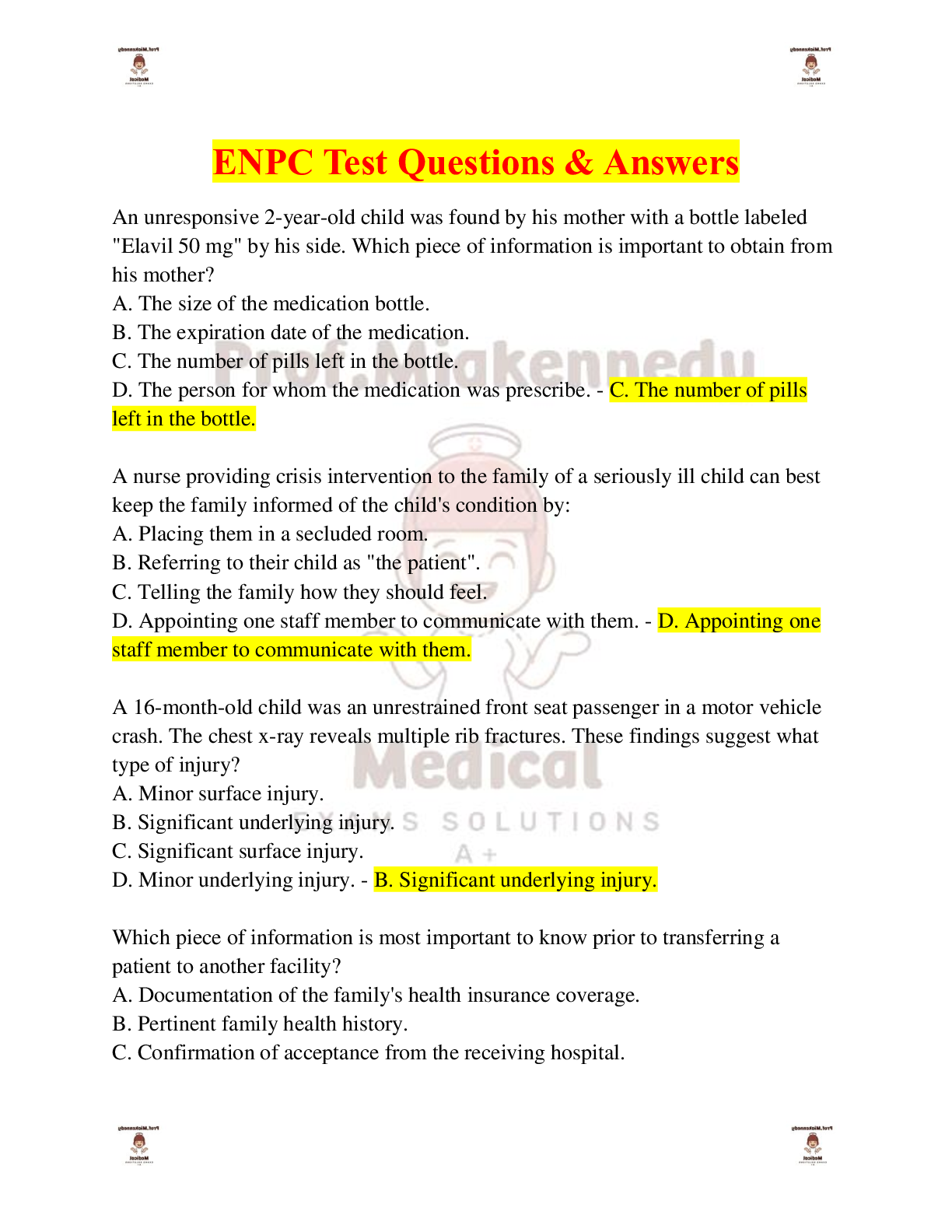
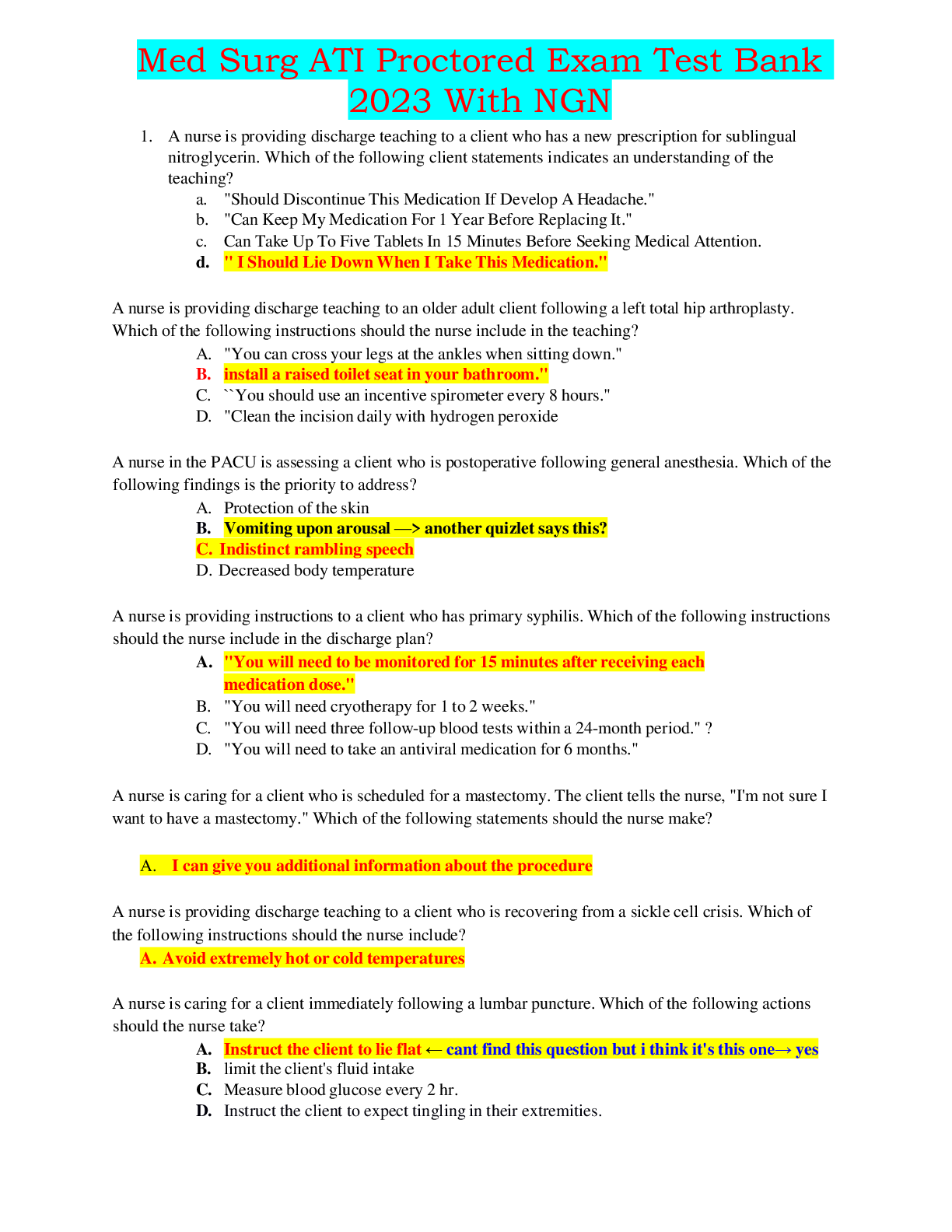
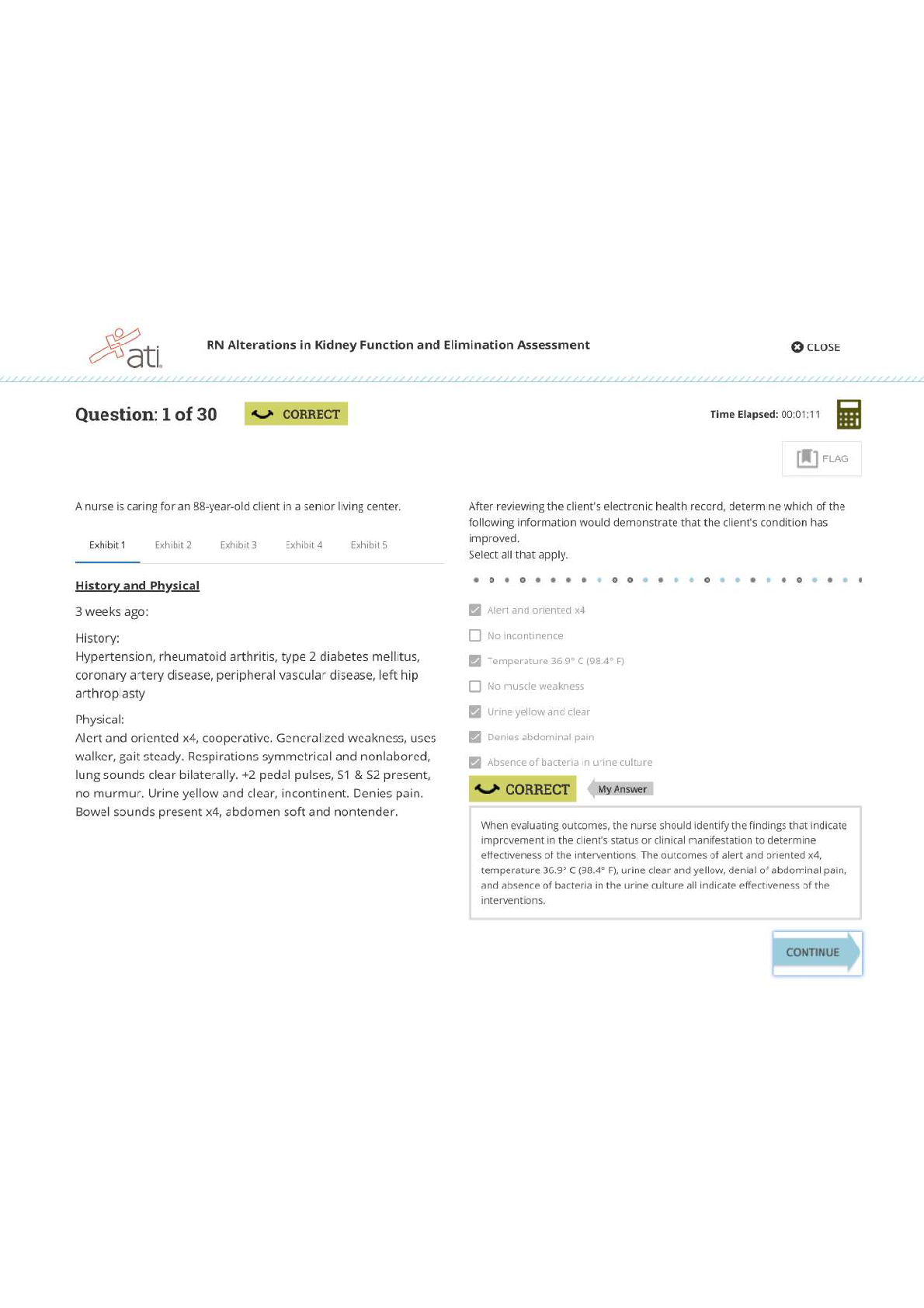
West Coast University: NURS 100 Ati funds Dosage Calculation Chapter 48 Dosage Calculation – Basic medication dose conversion and calculation skills are essential for providing safe nursing care... . – Nurses are responsible for administering the correct amount of medication by calculating the precise amount of medication to give. Nurses can use three different methods for dosage calculation: ratio and proportion, formula (desired over have), and dimensional analysis. TYPES OF CALCULATIONS – Solid oral medication – Liquid oral medication – Injectable medication – Correct doses by weight – IV infusion rates STANDARD CONVERSION FACTORS – 1 mg = 1,000 mcg – 1 g = 1,000 mg – 1 kg = 1,000 g – 1 oz = 30 mL – 1 L = 1,000 mL – 1 tsp = 5 mL – 1 tbsp = 15 mL – 1 tbsp = 3 tsp – 1 kg = 2.2 lb – 1 gr = 60 mg GENERAL ROUNDING GUIDELINES – ROUNDING UP: If the number to the right is equal to or greater than 5, round up by adding 1 to the number on the left. – ROUNDING DOWN: If the number to the right is less than 5, round down by dropping the number, leaving the number to the left as is. – For dosages less than 1.0: Round to the nearest hundredth. o For example (rounding up): 0.746 mL = 0.75 mL. • The calculated dose is 0.746 mL. Look at the number in the thousandths place (6). Six is greater than 5. To round to hundredths, add 1 to the 4 in the hundredths place and drop the 6. The rounded dose is 0.75 mL. o Or (rounding down): 0.743 mL = 0.74 mL. • The calculated dose is 0.743 mL. Look at the number in the thousandths place (3). Three is less than 5. To round to the hundredth, drop the 3 and leave the 4 as is. The rounded dose is 0.74 mL. – For dosages greater than 1.0: Round to the nearest tenth. o For example (rounding up): 1.38 = 1.4. • The calculated dose is 1.38 mg. Look at the number in the hundredths place (8). Eight is greater than 5. To round to the tenth, add 1 to the 3 in the tenth place and drop the 8. The rounded dose is 1.4 mg. o Or (rounding down): 1.34 mL = 1.3 mL. • The calculated dose is 1.34 mL. Look at the number in the hundredths place (4). Four is less than 5. To round to the tenth, drop the 4 and leave the 3 as is. The rounded dose is 1.3 mL. Solid dosage – Example: A nurse is preparing to administer phenytoin 0.2 g PO every 8 hr. The amount available is phenytoin 100 mg/capsule. How many capsules should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? Capsules STEP 2: What is the dose the nurse should administer? Dose to administer = Desired 0.2 g STEP 3: What is the dose available? Dose available = Have 100 mg STEP 4: Should the nurse convert the units of measurement? Yes (g ≠ mg). Set up an equation. 1 g = 0.2 g 1,000 mg X mg Solve for X X mg = 200mg Or you can use your knowledge of equivalents. 1 g = 1,000 mg (1 × 1,000) 0.2 g = 200 mg (0.2 × 1,000) STEP 5: What is the quantity of the dose available? = Quantity 1 capsule STEP 6: Set up the equation and solve for X. Have = Desired Quantity 100 mg 1 capsule X = 200 mg X capsule (s) X capsule(s) = 2 capsules STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 100 mg/capsule and the prescription reads 0.2 g (200 mg), it makes sense to administer 2 capsules. The nurse should administer phenytoin 2 capsules PO. USING DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? capsules STEP 2: What is the dose the nurse should administer? Dose to administer = Desired 0.2 g STEP 3: What is the dose available? Dose available = Have 100 mg STEP 4: Should the nurse convert the units of measurement? Yes (g = ̸ mg) Set up an equation. X mg= 0.2 g x 1,000 mg 1 g X mg = 200 mg Or you can use your knowledge of equivalents. 1 g = 1,000 mg (1 × 1,000) 0.2 g = 200 mg (0.2 × 1,000) STEP 5: What is the quantity of the dose available? = Quantity 1 capsule STEP 6: Set up the equation and solve for X. X = Desired x Quantity Have X capsule (s )= 200 mg x 1 cap 100 mg X capsule(s) = 2 capsules STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 100 mg/capsule and the prescription reads 0.2 g (200 mg), it makes sense to administer 2 capsules. The nurse should administer phenytoin 2 capsules PO. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X capsule(s) = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) X capsule (s )= 1 c apsule 100 mg STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measure. X capsule (s )= 1 capsule x 1,000 mg x 0.2 g 100 mg 1 g 1 STEP 4: Solve for X. X capsule(s) = 2 capsules STEP 5: Round, if necessary. STEP 6: Determine whether the amount to administer makes sense. If there are 100 mg/capsule and the prescription reads 0.2 g, it makes sense to administer 2 capsules. The nurse should administer phenytoin 2 capsules PO. Liquid dosage – Example: A nurse is preparing to administer amoxicillin 0.25 g PO every 8 hr. The amount available is amoxicillin oral suspension 250 mg/5 mL. How many mL should the nurse administer per dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? mL STEP 2: What is the dose the nurse should administer? Dose to administer = Desired 0.25 g STEP 3: What is the dose available? Dose available = Have 250 mg STEP 4: Should the nurse convert the units of measurement? Yes (g ≠ mg) (Place the unit of measure being calculated on the left side of the equation.) Set up an equation. 1 mg = 0.25 g 1,000 mg Xmg X mg = 200 mg Or you can use your knowledge of equivalents. 1 g = 1,000 mg (1 × 1,000) 0.25 g = 250 mg (0.25 × 1,000) STEP 5: What is the quantity of the dose available? = Quantity 5 mL STEP 6: Set up the equation and solve for X. Have = Desired Quantity X 250 mg = 250 mg 5 mL XmL X mL = 5 m STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 250 mg/5 mL and the prescription reads 0.25 g (250 mg), it makes sense to administer 5 mL. The nurse should administer amoxicillin 5 mL PO every 8 hr. USING DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? – mL STEP 2: What is the dose the nurse should administer? Dose to administer = Desired – 0.25 g STEP 3: What is the dose available? Dose available = Have – 250 mg STEP 4: Should the nurse convert the units of measurement? Yes (g ≠ mg) Set up an equation: X mg= 0.25 g x 1,000 mg 1 g X mg = 250 mg Or you can use your knowledge of equivalents. 1 g = 1,000 mg (1 × 1,000) 0.25 g = 250 mg (0.25 × 1,000) STEP 5: What is the quantity of the dose available? = Quantity 5 mL STEP 6: Set up the equation and solve for X. XmL= Desired x Quantity Have XmL=250 mg x 5 mL 250 mg XmL=5 mL STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 250 mg/5 mL and the prescription reads 0.25 g (250 mg), it makes sense to administer 5 mL. The nurse should administer amoxicillin 5 mL PO every 8 hr. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X mL = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) XmL= 5 mL 250 mg STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurement. X mL= 5 mL x 1,000 mg x 0.25 g 250 mg 1 g 1 STEP 4: Solve for X. X mL = 5 mL STEP 5: Round, if necessary. STEP 6: Determine whether the amount to administer makes sense. If there are 250 mg/5 mL and the prescription reads 0.25 g, it makes sense to administer 5 mL. The nurse should administer amoxicillin 5 mL PO every 8 hr Injectable dosage Example: A nurse is preparing to administer heparin 8,000 units subcutaneously every 12 hr. Available is heparin injection 10,000 units/mL. How many mL should the nurse administer per dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? mL STEP 2: What is the dose the nurse should administer? Dose to administer = Desired 8,000 units STEP 3: What is the dose available? Dose available = Have 10,000 units STEP 4: Should the nurse convert the units of measurement? No STEP 5: What is the quantity of the dose available? = Quantity 1 mL STEP 6: Set up the equation and solve for X. Have = Desired Quantity x 10,000 units = 8,000 units 1 mL X mL X mL = 0.8 mL STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 10,000 units/mL and the prescription reads 8,000 units, it makes sense to administer 0.8 mL. The nurse should administer heparin injection 0.8 mL subcutaneously every 12 hr. USING DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? mL STEP 2: What is the dose the nurse should administer? Dose to administer = Desired 8,000 units STEP 3: What is the dose available? Dose available = Have 10,000 units STEP 4: Should the nurse convert the units of measurement? No STEP 5: What is the quantity of the dose available? = Quantity 1 mL STEP 6: Set up an equation and solve for X. X mL= Desired x Quantity Have XmL=8,000 units x 1 mL 10,000 units X mL = 0.8 mL STEP 7: Round, if necessary. STEP 8: Determine whether the amount to administer makes sense. If there are 10,000 units/mL and the prescription reads 8,000 units, it makes sense to administer 0.8 mL. The nurse should administer heparin injection 0.8 mL subcutaneously every 12 hr. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X mL = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) XmL= 1mL 10,000 units STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. XmL= 8,000 units 10,000 units x 1 mL 1 dose STEP 4: Solve for X. X mL = 0.8 mL STEP 5: Round, if necessary. STEP 6: Determine whether the amount to administer makes sense. If there are 10,000 units/mL and the prescription reads 8,000 units, it makes sense to administer 0.8 mL. The nurse should administer heparin injection 0.8 mL subcutaneously every 12 hr. Dosages by weight – Example: A nurse is preparing to administer cefixime 8 mg/kg/day PO to divide equally every 12 hr to a toddler who weighs 22 lb. Available is cefixime suspension 100 mg/5 mL. How many mL should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? kg STEP 2: Set up an equation and solve for X. 2.2 lb = 1 kg Clien t' s desired weight ∈lb X kg 2.2 lb =22 lb 1 kg X kg X kg = 10 kg What is the dose the nurse should calculate? Dose to administer = Desired What is the dose available? Dose available = Have 100 mg STEP 3: What is the unit of measurement the nurse should calculate? mg STEP 4: Set up an equation and solve for X. X mg × kg/day = X mg/day = mg/kg/day × Client’s weight in kg X mg/day = 8 mg/kg/day × 10 kg X mg/day = 10 kg/day STEP 5: The dose is divided equally every 12 hours. Divide X by 2. 80 mg =40 mg 2 STEP 6: What is the unit of measurement the nurse should calculate? mL STEP 7: What is the dose the nurse should administer? Dose to administer = Desired 40 mg STEP 8: What is the dose available? Dose available = Have 100 mg STEP 9: Should the nurse convert the units of measurement? No STEP 10: What is the quantity of the dose available? = Quantity 5 mL STEP 11: Set up the equation and solve for X. Have = Desired Quantity x 100 mg = 40 mg 5 mL X mL X mL =2 mL STEP 12: Round, if necessary. STEP 13: Determine whether the amount to give makes sense. If there are 100 mg/5 mL and the prescription reads 40 mg, it makes sense to give 2 mL. The nurse should administer cefixime suspension 2 mL PO every 12 hr. USING DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? kg STEP 2: Set up an equation and solve for X. Clien t' s weight ∈lb x 1 kg X kg= 2.2 lb X kg= 22lb x 1 kg 2.2 lb X kg = 10 kg STEP 3: What is the unit of measurement the nurse should calculate? mg STEP 4: Set up an equation and solve for X. X = Dose per kg × Client’s weight in kg X mg = 8 mg × 10 kg X mg = 80 mg The dose is divided equally every 12 hours; therefore, divide X by 2. 80 mg =40 mg 2 STEP 5: What is the unit of measurement the nurse should calculate? mL STEP 6: What is the dose the nurse should administer? Dose to administer = Desired 40 mg STEP 7: What is the dose available? Dose available = Have 100 mg STEP 8: Should the nurse convert the units of measurement? No STEP 9: What is the quantity of the dose available? = Quantity 5 mL STEP 10: Set up an equation and solve for X. XmL= Desired x Quantity Have X mL= 40 mg x 5 mL 100 mg X mL = 2mL STEP 11: Round, if necessary. STEP 12: Determine whether the amount to give makes sense. If there are 100 mg/5 mL and the prescription reads 40 mg, it makes sense to give 2 mL. The nurse should administer cefixime suspension 2 mL PO every 12 hr. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X mL/dose = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) XmL = 5 mL dose 100 mg STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. Xml /dose =¿ Xml = 5 mL x 8 mg x 1 kg x 22 lb x 1 day dose 100 mg x 1 kg x 2.2 lb x 1 day x 2 dose STEP 4: Solve for X. X mL = 2 mL STEP 5: Round, if necessary. STEP 6: Determine whether the amount to give makes sense. If there are 100 mg/5 mL and the prescription reads 40 mg, it makes sense to give 2 mL. The nurse should administer cefixime suspension 2 mL PO every 12 hr. IV flow rates – Nurses calculate IV flow rates for large-volume continuous IV infusions and intermittent IV bolus infusions using electronic infusion pumps (mL/hr) and manual IV tubing (gtt/min). IV INFUSIONS WITH ELECTRONIC INFUSION PUMPS – Infusion pumps control an accurate rate of fluid infusion. Infusion pumps deliver a specific amount of fluid during a specific amount of time. For example, an infusion pump can deliver 150 mL in 1 hr or 50 mL in 20 min. Example: A nurse is preparing to administer dextrose 5% in water (D5W) 500 mL IV to infuse over 4 hr. The nurse should set the IV infusion pump to deliver how many mL/hr? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION AND DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? mL/hr STEP 2: What is the volume the nurse should infuse? 500 mL STEP 3: What is the total infusion time? 4 hr STEP 4: Should the nurse convert the units of measurement? No STEP 5: Set up the equation and solve for X. X mL / hr= Volume(mL) Time (hr ) X mL / hr= 500 mL 4 hr STEP 6: Round, if necessary. STEP 7: Determine whether the IV flow rate makes sense. If the prescription reads 500 mL to infuse over 4 hr, it makes sense to administer 125 mL/hr. The nurse should set the IV pump to deliver D5W 500 mL IV at 125 mL/hr. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X mL/hr = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) X mL / hr= 500 mL 4 hr STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. X mL / hr= 500 mL 4 hr STEP 4: Solve for X. X mL/hr = 125 mL/hr STEP 5: Round, if necessary. STEP 6: Determine whether the IV flow rate makes sense. If the prescription reads 500 mL to infuse over 4 hr, it makes sense to administer 125 mL/hr. The nurse should set the IV pump to deliver D5W 500 mL IV at 125 mL/hr. Example: A nurse is preparing to administer cefotaxime 1 g intermittent IV bolus over 45 min. Available is cefotaxime 1 g in 100 mL 0.9% sodium chloride (0.9% NaCl). The nurse should set the IV infusion pump to deliver how many mL/hr? USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? mL/hr STEP 2: What is the volume the nurse should infuse? 100 mL STEP 3: What is the total infusion time? 45 min STEP 4: Should the nurse convert the units of measurement? Yes (min does not equal hr) 60 min = 45 min 1 hr X hr X hr = 0.75 hr Step 5: Set up an equation and solve for X X mL = Volume(mL) hr Time (hr ) X mL = 100 mL hr 0.75 hr X mL/hr = 133.333333 mL/hr STEP 6: Round, if necessary. 133.3333 rounds to 133 STEP 7: Determine whether the IV flow rate makes sense. If the prescription reads 100 mL to infuse over 45 min (0.75 hr), it makes sense to administer 133 mL/hr. The nurse should set the IV pump to deliver cefotaxime 1 g in 100 mL of 0.9% NaCl IV at 133 mL/hr. USING DESIRED OVER HAVE STEP 1: What is the unit of measure the nurse should calculate? mL/hr STEP 2: What is the volume the nurse should infuse? 100 mL STEP 3: What is the total infusion time? 45 min STEP 4: Should the nurse convert the units of measurement? Yes (min does not equal hr) X hr= 45 minx 1hr 60 min X hr = 0.75 hr STEP 5: Set up the equation and solve for X. X mL / hr= Volume (mL) Time X mL / hr= 100 mL 0.75 hr X mL/hr = 133.333333 rounds to 133 STEP 7: Determine whether the amount to administer makes sense. If the prescription reads 100 mL to infuse over 45 min (0.75hr), it makes sense to administer 133 mL/hr. The nurse should set the IV pump to deliver cefotaxime 1 g in 100 mL of 0.9% NaCl IV at 133 mL/hr. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X mL/hr = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) X mL / hr= 100 mL 30 min STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. XmL /hr =100 mL x 60 min 45 minx 1hr STEP 4: Solve for X. X mL/hr = 133.333333 mL/hr STEP 5: Round, if necessary. 133.333333 rounds to 133 STEP 6: Determine whether the IV flow rate makes sense. If the prescription reads 100 mL to infuse over 45 min (0.75 hr), it makes sense to administer 133 mL/hr. The nurse should set the IV pump to deliver cefotaxime 1 g in 100 mL of 0.9% NaCl IV at 133 mL/hr. MANUAL IV INFUSIONS – If an electronic infusion pump is not available, regulate the IV flow rate using the roller clamp on the IV tubing. When setting the flow rate, count the number of drops that fall into the drip chamber over 1 min. Then calculate the flow rate using the drop factor on the manufacturer’s package containing the administration set. The drop factor is the number of drops per milliliter of solution. Example: A nurse is preparing to administer lactated Ringer’s (LR) 1,500 mL IV to infuse over 10 hr. The drop factor of the manual IV tubing is 15 gtt/mL. The nurse should adjust the manual IV infusion to deliver how many gtt/min? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION STEP 1: What is the unit of measurement the nurse should calculate? gtt/min STEP 2: What is the volume the nurse should infuse? 1,500 mL STEP 3: What is the total infusion time? 10 hr STEP 4: Should the nurse convert the units of measurement? No (mL = mL) Yes (hr ≠ min) 1 hr = 10 hr 60 min X min X min = 600 min STEP 5: Set up the equation and solve for X. X =Volume (mL ) x drop factor ( gtt / mL) Time (min) X gtt / min¿ 1,500 mLx 15 gtt 600 min x 1 mL STEP 6: Round, if necessary. 37.5 rounds to 38 STEP 7: Determine whether the IV flow rate makes sense. If the prescription reads 1,500 mL to infuse over 10 hr (600 min), it makes sense to administer 38 gtt/min. The nurse should adjust the manual IV infusion to deliver LR 1,500 mL IV at 38 gtt/min. USING DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? gtt/min STEP 2: What is the volume the nurse should infuse? 1,500 mL STEP 3: What is the total infusion time? 10 hr STEP 4: Should the nurse convert the units of measurement? Yes (hr does not equal min) X hr= 60 min x 10 hr 1 hr X min = 600 min STEP 5: Set up the equation and solve for X. X =Volume (mL ) x drop factor ( gtt / mL) Time (min) X gtt / min= 1,5000 mL x 15 gtt 600 min x 1 mL X gtt / min=37.5 gtt / min STEP 6: Round, if necessary. 37.5 rounds to 38 STEP 7: Determine whether the IV flow rate makes sense. If the prescription reads 1,500 mL to infuse over 10 hr (600 min), it makes sense to administer 38 gtt/min. The nurse should adjust the manual IV infusion to deliver LR 1,500 mL IV at 38 gtt/min. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measurement the nurse should calculate? (Place the unit of measure being calculated on the left side of the equation.) X gtt/min = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on the right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) X gtt / min¿ 10 gtt 1 mL STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. X gtt / min= 10 gtt x 1,500 mL x 1hr 1 mL x 10 hr x 60 min STEP 4: Solve for X. X gtt/min = 37.5 gtt/min STEP 5: Round, if necessary. 37.5 rounds to 38 STEP 6: Determine whether the IV flow rate makes sense. If the prescription reads 1,500 mL to infuse over 10 hr (600 min), it makes sense to administer 38 gtt/min. The nurse should adjust the manual IV infusion to deliver LR 1,500 mL IV at 38 gtt/min. Example: A nurse is preparing to administer ranitidine 150 mg by intermittent IV bolus. Available is ranitidine 150 mg in 100 mL of 0.9% sodium chloride (0.9% NaCl) to infuse over 30 min. The drop factor of the manual IV tubing is 10 gtt/mL. The nurse should adjust the manual IV infusion to deliver how many gtt/min? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) USING RATIO AND PROPORTION AND DESIRED OVER HAVE STEP 1: What is the unit of measurement the nurse should calculate? gtt/min STEP 2: What is the volume the nurse should infuse? 100 mL STEP 3: What is the total infusion time? 30 min STEP 4: Should the nurse convert the units of measurement? No STEP 5: Set up the equation and solve for X. X =Volume (mL ) x drop factor ( gtt / mL) Time (min) X gtt / min¿ 100 mL x 10 gtt 30 min x 1 mL X gtt/min = 33.333333 gtt/min STEP 6: Round if necessary. 33.333333 rounds to 33 STEP 7: Determine whether the IV flow rate makes sense. If the amount prescribed is 100 mL to infuse over 30 min, it makes sense to administer 33 gtt/min. The nurse should adjust the manual IV infusion to deliver ranitidine 150 mg in 100 mL of 0.9% NaCl IV at 33 gtt/min. USING DIMENSIONAL ANALYSIS STEP 1: What is the unit of measure to calculate? (Place the unit of measure being calculated on the left side of the equation.) X gtt/min = STEP 2: Determine the ratio that contains the same unit as the unit being calculated. (Place the ratio on he right side of the equation ensuring that the unit in the numerator matches the unit being calculated.) X gtt / min¿ 10 gtt 1 mL STEP 3: Place any remaining ratios that are relevant to the item on the right side of the equation along with any needed conversion factors to cancel out unwanted units of measurements. X gtt / min¿ 10 gtt x 100 mL 1 mL x 30 min STEP 4: Solve for X. X gtt/min = 33.333333 gtt/min STEP 5: Round if necessary. 33.333333 rounds to 33 STEP 6: Determine whether the IV flow rate makes sense. If the amount prescribed is 100 mL to infuse over 30 min, it makes sense to administer 33 gtt/min. The nurse should adjust the manual IV infusion to deliver ranitidine 150 mg in 100 mL of 0.9% NaCl IV at 33 gtt/min. 1. A nurse is preparing to administer methylprednisolone 10 mg by IV bolus. The amount available is methylprednisolone injection 40 mg/mL. How many mL should the nurse administer? (Round the answer to the nearest tenth. Do not use a trailing zero.) 2. A nurse is preparing to administer lactated Ringer’s (LR) IV 100 mL over 15 min. The nurse should set the IV infusion pump to deliver how many mL/hr? (Round the answer to the nearest whole number. Do not use a trailing zero.) 3. A nurse is preparing to administer 0.9% sodium chloride (0.9% NaCl) 250 mL IV to infuse over 30 min. The drop factor of the manual IV tubing is 10 gtt/mL. The nurse should adjust the manual IV infusion to deliver how many gtt/min? (Round the answer to the nearest whole number. Do not use a trailing zero.) 4. A nurse is preparing to administer metoprolol 200 mg PO daily. The amount available is metoprolol 100 mg/tablet. How many tablets should the nurse administer? (Round the answer to the nearest whole number. Do not use a trailing zero.) 5. A nurse is preparing to administer ketorolac 0.5 mg/kg IV bolus every 6 hr to a school-age child who weighs 66 lb. The amount available is ketorolac injection 30 mg/mL. How many mL should the nurse administer per dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.) 6. A nurse is preparing to administer dextrose 5% in water (D5W) 1,000 mL IV to infuse over 10 hr. The nurse should set the IV infusion pump to deliver how many mL/hr? (Round the answer to the nearest whole number. Do not use a trailing zero.) 7. A nurse is preparing to administer acetaminophen 320 mg PO every 4 hr PRN for pain. The amount available is acetaminophen liquid 160 mg/5 mL. How many mL should the nurse administer per dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.) 8. A nurse is preparing to administer dextrose 5% in lactated Ringer’s (D5LR) 1,000 mL to infuse over 6 hr. The drop factor of the manual IV tubing is 15 gtt/mL. The nurse should adjust the manual IV infusion to deliver how many gtt/min? (Round the answer to the nearest whole number. Do not use a trailing zero.) [Show More]
Last updated: 1 year ago
Preview 1 out of 30 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2023
Number of pages
30
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2023
Downloads
0
Views
19