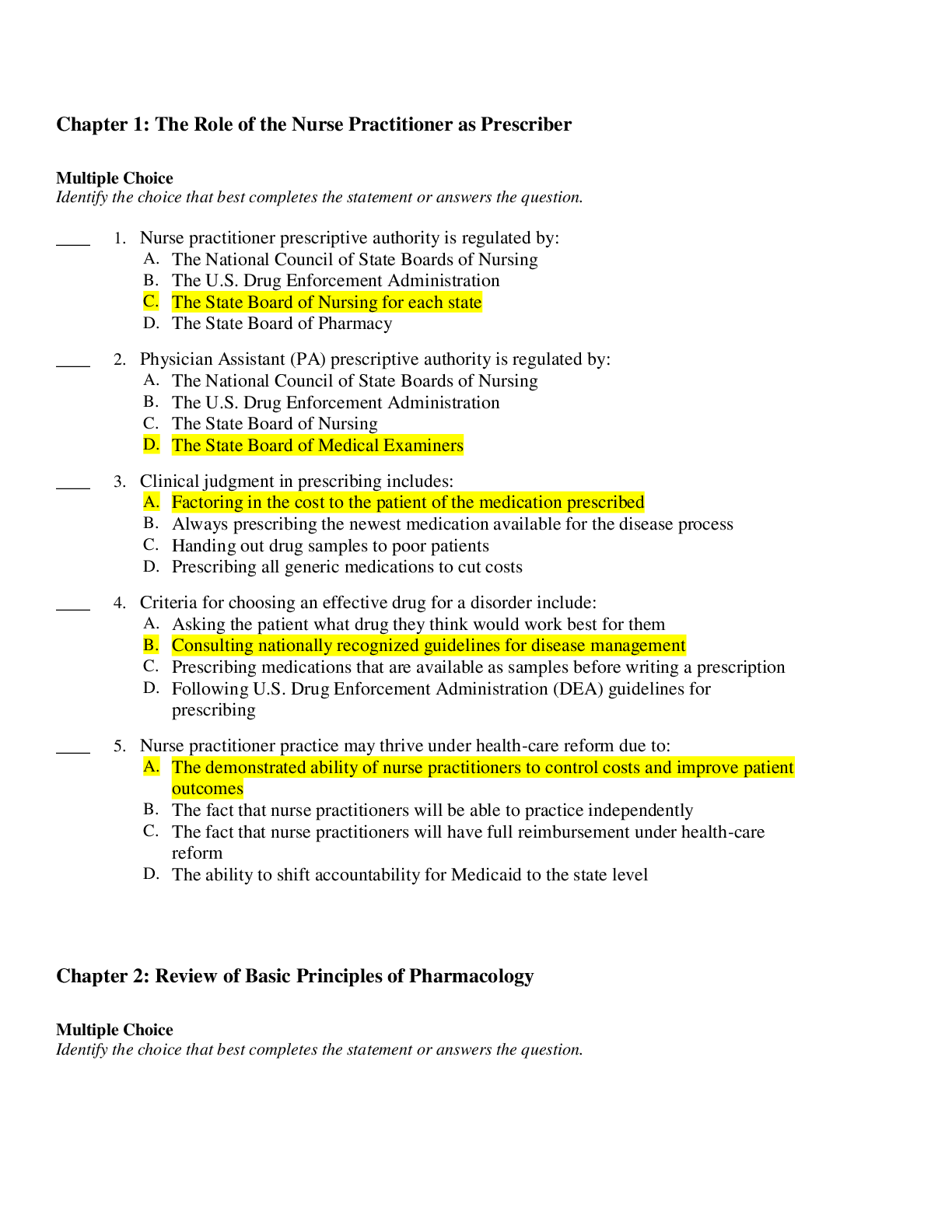
*NURSING > EXAM > Florida International University - NUR 3145 Chapters 1-21 EXAM BANK {2022} Lilley: Pharmacology and (All)
Florida International University - NUR 3145 Chapters 1-21 EXAM BANK {2022} Lilley: Pharmacology and the Nursing Process, 8th Edition.
Document Content and Description Below
Chapter 01: The Nursing Process and Drug Therapy Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is writing a nursing diagnosis for a plan of care for a ... patient who has been newly diagnosed with type 2 diabetes. Which statement reflects the correct format for a nursing diagnosis? a. Anxiety b. Anxiety related to new drug therapy c. Anxiety related to anxious feelings about drug therapy, as evidenced by statements such as “I’m upset about having to test my blood sugars.” d. Anxiety related to new drug therapy, as evidenced by statements such as “I’m upset about having to test my blood sugars.” ANS: D Formulation of nursing diagnoses is usually a three-step process. “Anxiety” is missing the “related to” and “as evidenced by” portions of defining characteristics. “Anxiety related to new drug therapy” is missing the “as evidenced by” portion of defining characteristics. The statement beginning “Anxiety related to anxious feelings” is incorrect because the “related to” section is simply a restatement of the problem “anxiety,” not a separate factor related to the response. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 7 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Safe and Effective Care Environment: Management of Care 2. The patient is to receive oral guaifenesin (Mucinex) twice a day. Today, the nurse was busy and gave the medication 2 hours after the scheduled dose was due. What type of problem does this represent? a. “Right time” b. “Right dose” c. “Right route” d. “Right medication” ANS: A “Right time” is correct because the medication was given more than 30 minutes after the scheduled dose was due. “Dose” is incorrect because the dose is not related to the time the medication administration is scheduled. “Route” is incorrect because the route is not affected. “Medication” is incorrect because the medication ordered will not change. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 11 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 3. The nurse has been monitoring the patient’s progress on a new drug regimen since the first dose and documenting the patient’s therapeutic response to the medication. Which phase of the nursing process do these actions illustrate? a. Nursing diagnosis b. Planning c. Implementation d. Evaluation ANS: D Monitoring the patient’s progress, including the patient’s response to the medication, is part of the evaluation phase. Planning, implementation, and nursing diagnosis are not illustrated by this example. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: pp. 13-14 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 4. The nurse is assigned to a patient who is newly diagnosed with type 1 diabetes mellitus. Which statement best illustrates an outcome criterion for this patient? a. The patient will follow instructions. b. The patient will not experience complications. c. The patient will adhere to the new insulin treatment regimen. d. The patient will demonstrate correct blood glucose testing technique. ANS: D “Demonstrating correct blood glucose testing technique” is a specific and measurable outcome criterion. “Following instructions” and “not experiencing complications” are not specific criteria. “Adhering to new regimen” would be difficult to measure. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 8 TOP: NURSING PROCESS: Planning MSC: NCLEX: Safe and Effective Care Environment: Management of Care 5. Which activity best reflects the implementation phase of the nursing process for the patient who is newly diagnosed with hypertension? a. Providing education on keeping a journal of blood pressure readings b. Setting goals and outcome criteria with the patient’s input c. Recording a drug history regarding over-the-counter medications used at home d. Formulating nursing diagnoses regarding deficient knowledge related to the new treatment regimen ANS: A Education is an intervention that occurs during the implementation phase. Setting goals and outcomes reflects the planning phase. Recording a drug history reflects the assessment phase. Formulating nursing diagnoses reflects analysis of data as part of planning. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 8-9 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 6. The medication order reads, “Give ondansetron (Zofran) 4 mg, 30 minutes before beginning chemotherapy to prevent nausea.” The nurse notes that the route is missing from the order. What is the nurse’s best action? a. Give the medication intravenously because the patient might vomit. b. Give the medication orally because the tablets are available in 4-mg doses. c. Contact the prescriber to clarify the route of the medication ordered. d. Hold the medication until the prescriber returns to make rounds. ANS: C A complete medication order includes the route of administration. If a medication order does not include the route, the nurse must ask the prescriber to clarify it. The intravenous and oral routes are not interchangeable. Holding the medication until the prescriber returns would mean that the patient would not receive a needed medication. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 12 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 7. When the nurse considers the timing of a drug dose, which factor is appropriate to consider when deciding when to give a drug? a. The patient’s ability to swallow b. The patient’s height c. The patient’s last meal d. The patient’s allergies ANS: C The nurse must consider specific pharmacokinetic/pharmacodynamic drug properties that may be affected by the timing of the last meal. The patient’s ability to swallow, height, and allergies are not factors to consider regarding the timing of the drug’s administration. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 12 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care 8. The nurse is performing an assessment of a newly admitted patient. Which is an example of subjective data? a. Blood pressure 158/96 mm Hg b. Weight 255 pounds c. The patient reports that he uses the herbal product ginkgo. d. The patient’s laboratory work includes a complete blood count and urinalysis. ANS: C Subjective data include information shared through the spoken word by any reliable source, such as the patient. Objective data may be defined as any information gathered through the senses or that which is seen, heard, felt, or smelled. A patient’s blood pressure, weight, and laboratory tests are all examples of objective data. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 6 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care MULTIPLE RESPONSE 1. When giving medications, the nurse will follow the rights of medication administration. The rights include the right documentation, the right reason, the right response, and the patient’s right to refuse. Which of these are additional rights? (Select all that apply.) a. Right drug b. Right route c. Right dose d. Right diagnosis e. Right time f. Right patient ANS: A, B, C, E, F Additional rights of medication administration must always include the right drug, right dose, right time, right route, and right patient. The right diagnosis is incorrect. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 9 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 2. Place the phases of the nursing process in the correct order, with 1 as the first phase and 5 as the last phase. (Select all that apply.) a. Planning b. Evaluation c. Assessment d. Implementation e. Nursing Diagnoses ANS: A, B, C, D, E The nursing process is an ongoing process that begins with assessing and continues with diagnosing, planning, implementing, and evaluating. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 4 TOP: NURSING PROCESS: General MSC: NCLEX: Safe and Effective Care Environment: Management of Care Chapter 02: Pharmacologic Principles Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The patient is receiving two different drugs. At current dosages and dosage forms, both drugs are absorbed into the circulation in identical amounts. Which term is used to identify this principle? a. Bioequivalent b. Synergistic c. Prodrugs d. Steady state ANS: A Two drugs absorbed into the circulation in the same amount (in specific dosage forms) have the same bioavailability; thus, they are bioequivalent. A drug’s steady state is the physiologic state in which the amount of drug removed via elimination is equal to the amount of drug absorbed from each dose. The term synergistic refers to two drugs, given together, with a resulting effect that is greater than the sum of the effects of each drug given alone. A prodrug is an inactive drug dosage form that is converted to an active metabolite by various biochemical reactions once it is inside the body. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 21 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. When given an intravenous medication, the patient says to the nurse, “I usually take pills. Why does this medication have to be given in the arm?” What is the nurse’s best answer? a. “The medication will cause fewer adverse effects when given intravenously.” b. “The intravenous medication will have delayed absorption into the body’s tissues.” c. “The action of the medication will begin sooner when given intravenously.” d. “There is a lower chance of allergic reactions when drugs are given intravenously.” ANS: C An intravenous (IV) injection provides the fastest route of absorption. The IV route does not affect the number of adverse effects, nor does it cause delayed tissue absorption (it results in faster absorption). The IV route does not affect the number of allergic reactions. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 22 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. The nurse is administering parenteral drugs. Which statement is true regarding parenteral drugs? a. Parenteral drugs bypass the first-pass effect. b. Absorption of parenteral drugs is affected by reduced blood flow to the stomach. c. Absorption of parenteral drugs is faster when the stomach is empty. d. Parenteral drugs exert their effects while circulating in the bloodstream. ANS: A Drugs given by the parenteral route bypass the first-pass effect. Reduced blood flow to the stomach and the presence of food in the stomach apply to enteral drugs (taken orally), not to parenteral drugs. Parenteral drugs must be absorbed into cells and tissues from the circulation before they can exert their effects; they do not exert their effects while circulating in the bloodstream. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 22 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. When monitoring the patient receiving an intravenous infusion to reduce blood pressure, the nurse notes that the patient’s blood pressure is extremely low, and the patient is lethargic and difficult to awaken. This would be classified as which type of adverse drug reaction? a. Adverse effect b. Allergic reaction c. Idiosyncratic reaction d. Pharmacologic reaction ANS: D A pharmacologic reaction is an extension of a drug’s normal effects in the body. In this case, the antihypertensive drug lowered the patient’s blood pressure levels too much. The other options do not describe a pharmacologic reaction. An adverse effect is a predictable, well-known adverse drug reaction that results in minor or no changes in patient management. An allergic reaction (also known as a hypersensitivity reaction) involves the patient’s immune system. An idiosyncratic reaction is unexpected and is defined as a genetically determined abnormal response to normal dosages of a drug. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 32 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. The nurse is reviewing pharmacology terms for a group of newly graduated nurses. Which sentence defines a drug’s half-life? a. The time it takes for the drug to cause half of its therapeutic response b. The time it takes for one half of the original amount of a drug to reach the target cells c. The time it takes for one half of the original amount of a drug to be removed from the body d. The time it takes for one half of the original amount of a drug to be absorbed into the circulation ANS: C A drug’s half-life is the time it takes for one half of the original amount of a drug to be removed from the body. It is a measure of the rate at which drugs are removed from the body. The other options are incorrect definitions of half-life. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 27 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. When administering drugs, the nurse remembers that the duration of action of a drug is defined as which of these? a. The time it takes for a drug to elicit a therapeutic response b. The amount of time needed to remove a drug from circulation c. The time it takes for a drug to achieve its maximum therapeutic response d. The time period at which a drug’s concentration is sufficient to cause a therapeutic response ANS: D Duration of action is the time during which drug concentration is sufficient to elicit a therapeutic response. The other options do not define duration of action. A drug’s onset of action is the time it takes for the drug to elicit a therapeutic response. A drug’s peak effect is the time it takes for the drug to reach its maximum therapeutic response. Elimination is the length of time it takes to remove a drug from circulation. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 28 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. When reviewing the mechanism of action of a specific drug, the nurse reads that the drug works by selective enzyme interaction. Which of these processes describes selective enzyme interaction? a. The drug alters cell membrane permeability. b. The drug’s effectiveness within the cell walls of the target tissue is enhanced. c. The drug is attracted to a receptor on the cell wall, preventing an enzyme from binding to that receptor. d. The drug binds to an enzyme molecule and inhibits or enhances the enzyme’s action with the normal target cell. ANS: D With selective enzyme interaction, the drug attracts the enzymes to bind with the drug instead of allowing the enzymes to bind with their normal target cells. As a result, the target cells are protected from the action of the enzymes. This results in a drug effect. The actions described in the other options do not occur with selective enzyme interactions. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 29 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. When administering a new medication to a patient, the nurse reads that it is highly protein bound. Assuming that the patient’s albumin levels are normal, the nurse would expect which result, as compared to a medication that is not highly protein bound? a. Renal excretion will be faster. b. The drug will be metabolized quickly. c. The duration of action of the medication will be shorter. d. The duration of action of the medication will be longer. ANS: D Drugs that are bound to plasma proteins are characterized by longer duration of action. Protein binding does not make renal excretion faster, does not speed up drug metabolism, and does not cause the duration of action to be shorter. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 24-25 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The patient is experiencing chest pain and needs to take a sublingual form of nitroglycerin. Where does the nurse instruct the patient to place the tablet? a. Under the tongue b. On top of the tongue c. At the back of the throat d. In the space between the cheek and the gum ANS: A Drugs administered via the sublingual route are placed under the tongue. Drugs administered via the buccal route are placed in the space between the cheek and the gum; oral drugs are swallowed. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 22 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. The nurse is administering medications to the patient who is in renal failure resulting from end-stage renal disease. The nurse is aware that patients with kidney failure would most likely have problems with which pharmacokinetic phase? a. Absorption b. Distribution c. Metabolism d. Excretion ANS: D The kidneys are the organs that are most responsible for drug excretion. Renal function does not affect the absorption and distribution of a drug. Renal function may affect metabolism of drugs to a small extent. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 26 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient who has advanced cancer is receiving opioid medications around the clock to keep him comfortable as he nears the end of his life. Which term best describes this type of therapy? a. Palliative therapy b. Maintenance therapy c. Empiric therapy d. Supplemental therapy ANS: A The goal of palliative therapy is to make the patient as comfortable as possible. It is typically used in the end stages of illnesses when all attempts at curative therapy have failed. Maintenance therapy is used for the treatment of chronic illnesses such as hypertension. Empiric therapy is based on clinical probabilities and involves drug administration when a certain pathologic condition has an uncertain but high likelihood of occurrence based on the patient’s initial presenting symptoms. Supplemental (or replacement therapy) supplies the body with a substance needed to maintain normal function. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 30 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. The patient is complaining of a headache and asks the nurse which over-the-counter medication form would work the fastest to help reduce the pain. Which medication form will the nurse suggest? a. A capsule b. A tablet c. An enteric-coated tablet d. A powder ANS: D Of the types of oral medications listed, the powder form would be absorbed the fastest, thus having a faster onset. The tablet, the capsule, and, finally, the enteric-coated tablet would be absorbed next, in that order. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 20 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 13. The nurse will be injecting a drug into the fatty tissue of the patient’s abdomen. Which route does this describe? a. Intradermal b. Subcutaneous c. Intramuscular d. Transdermal ANS: B Injections into the fatty subcutaneous tissue under the dermal layer of skin are referred to as subcutaneous injections. Injections under the more superficial skin layers immediately underneath the epidermal layer of skin and into the dermal layer are known as intradermal injections. Injections into the muscle beneath the subcutaneous fatty tissue are referred to as intramuscular injections. Transdermal drugs are applied to the skin via an adhesive patch. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 24 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. Which drugs would be affected by the first-pass effect? (Select all that apply.) a. Morphine given by IV push injection b. Sublingual nitroglycerin tablets c. Diphenhydramine (Benadryl) elixir d. Levothyroxine (Synthroid) tablets e. Transdermal nicotine patches f. Esomeprazole (Nexium) capsules g. Penicillin given by IV piggyback infusion ANS: C, D, F Orally administered drugs (elixirs, tablets, capsules) undergo the first-pass effect because they are metabolized in the liver after being absorbed into the portal circulation from the small intestine. IV medications (IV push and IV piggyback) enter the bloodstream directly and do not go directly to the liver. Sublingual tablets and transdermal patches also enter the bloodstream without going directly to the liver, thus avoiding the first-pass effect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 24 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A drug dose that delivers 250 mg has a half-life of 5 hours. Identify how much drug will remain in the body after one half-life. _______ ANS: 125 mg A drug’s half-life is the time required for one half of an administered dose of a drug to be eliminated by the body, or the time it takes for the blood level of a drug to be reduced by 50%. Therefore, one half of 250 mg equals 125 mg. DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 03: Lifespan Considerations Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. Drug transfer to the fetus is more likely during the last trimester of pregnancy for which reason? a. Decreased fetal surface area b. Increased placental surface area c. Enhanced blood flow to the fetus d. Increased amount of protein-bound drug in maternal circulation ANS: C Drug transfer to the fetus is more likely during the last trimester as a result of enhanced blood flow to the fetus. The other options are incorrect. Increased fetal surface area, not decreased, is a factor that affects drug transfer to the fetus. The placenta’s surface area does not increase during this time. Drug transfer is increased because of an increased amount of free drug, not protein-bound drug, in the mother’s circulation. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 37 TOP: NURSING PROCESS: General MSC: NCLEX: Health Promotion and Maintenance 2. The nurse is monitoring a patient who is in the 26th week of pregnancy and has developed gestational diabetes and pneumonia. She is given medications that pose a possible fetal risk, but the potential benefits may warrant the use of the medications in her situation. The nurse recognizes that these medications are in which U.S. Food and Drug Administration pregnancy safety category? a. Category X b. Category B c. Category C d. Category D ANS: D Pregnancy category D fits the description given. Category B indicates no risk to animal fetus; information for humans is not available. Category C indicates adverse effects reported in animal fetus; information for humans is not available. Category X consists of drugs that should not be used in pregnant women because of reports of fetal abnormalities and positive evidence of fetal risk in humans. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 37 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 3. When discussing dosage calculation for pediatric patients with a clinical pharmacist, the nurse notes that which type of dosage calculation is used most commonly in pediatric calculations? a. West nomogram b. Clark rule c. Height-to-weight ratio d. Milligram per kilogram of body weight formula ANS: D The milligram per kilogram formula, based on body weight, is the most common method of calculating doses for pediatric patients. The other options are available methods but are not the most commonly used. Height-to-weight ratio is not used. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 39 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is assessing a newly admitted 83-year-old patient and determines that the patient is experiencing polypharmacy. Which statement most accurately illustrates polypharmacy? a. The patient is experiencing multiple illnesses. b. The patient uses one medication for an illness several times per day. c. The patient uses over-the-counter drugs for an illness. d. The patient uses multiple medications simultaneously. ANS: D Polypharmacy usually occurs when a patient has several illnesses and takes medications for each of them, possibly prescribed by different specialists who may be unaware of other treatments the patient is undergoing. The other options are incorrect. Polypharmacy addresses the medications taken, not just the illnesses. Polypharmacy means the patient is taking several different medications, not just one, and can include prescription drugs, over-the-counter medications, and herbal products. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 40 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. The nurse is aware that confusion, forgetfulness, and increased risk for falls are common responses in an elderly patient who is taking which type of drug? a. Laxatives b. Anticoagulants c. Sedatives d. Antidepressants ANS: C Sedatives and hypnotics often cause confusion, daytime sedation, ataxia, lethargy, forgetfulness, and increased risk for falls in the elderly. Laxatives, anticoagulants, and antidepressants may cause adverse effects in the elderly, but not the ones specified in the question. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 43 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 6. For accurate medication administration to pediatric patients, the nurse must take into account which criteria? a. Organ maturity b. Renal output c. Body temperature d. Height ANS: A To administer medications to pediatric patients accurately, one must take into account organ maturity, body surface area, age, and weight. The other options are incorrect; renal output and body temperature are not considerations, and height alone is not sufficient. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 39 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. The nurse recognizes that it is not uncommon for an elderly patient to experience a reduction in the stomach’s ability to produce hydrochloric acid. This change may result in which effect? a. Delayed gastric emptying b. Increased gastric acidity c. Decreased intestinal absorption of medications d. Altered absorption of weakly acidic drugs ANS: D Reduction in the stomach’s ability to produce hydrochloric acid is an aging-related change that results in a decrease in gastric acidity and may alter the absorption of weakly acidic drugs. The other options are not results of reduced hydrochloric acid production. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 42 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is administering drugs to neonates and will consider which factor may contribute the most to drug toxicity? a. The lungs are immature. b. The kidneys are small. c. The liver is not fully developed. d. Excretion of the drug occurs quickly. ANS: C A neonate’s liver is not fully developed and cannot detoxify many drugs. The other options are incorrect. The lungs and kidneys do not play major roles in drug metabolism. Renal excretion is slow, not fast, because of organ immaturity, but this is not the factor that contributes the most to drug toxicity. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 38 TOP: NURSING PROCESS: Planning MSC: NCLEX: Health Promotion and Maintenance 9. An 83-year-old woman has been given a thiazide diuretic to treat mild heart failure. She and her daughter should be told to watch for which problems? a. Constipation and anorexia b. Fatigue, leg cramps, and dehydration c. Daytime sedation and lethargy d. Edema, nausea, and blurred vision ANS: B Electrolyte imbalance, leg cramps, fatigue, and dehydration are common complications when thiazide diuretics are given to elderly patients. The other options do not describe complications that occur when these drugs are given to the elderly. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 43 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. An elderly patient with a new diagnosis of hypertension will be receiving a new prescription for an antihypertensive drug. The nurse expects which type of dosing to occur with this drug therapy? a. Drug therapy will be based on the patient’s weight. b. Drug therapy will be based on the patient’s age. c. The patient will receive the maximum dose that is expected to reduce the blood pressure. d. The patient will receive the lowest possible dose at first, and then the dose will be increased as needed. ANS: D As a general rule, dosing for elderly patients should follow the admonition, “Start low, and go slow,” which means to start with the lowest possible dose (often less than an average adult dose) and increase the dose slowly, if needed, based on patient response. The other responses are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 40 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. The nurse is trying to give a liquid medication to a -year-old child and notes that the medication has a strong taste. Which technique is the best way for the nurse to give the medication to this child? a. Give the medication with a spoonful of ice cream. b. Add the medication to the child’s bottle. c. Tell the child you have candy for him. d. Add the medication to a cup of milk. ANS: A Ice cream or another nonessential food disguises the taste of the medication. The other options are incorrect. If the child does not drink the entire contents of the bottle, medication is wasted and the full dose is not administered. Using the word candy with drugs may lead to the child thinking that drugs are actually candy. If the medication is mixed with a cup of milk, the child may not drink the entire cup of milk, and the distasteful drug may cause the child to refuse milk in the future. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 45 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. The nurse is preparing to give an injection to a 4-year-old child. Which intervention is age appropriate for this child? a. Give the injection without any advanced preparation. b. Give the injection, and then explain the reason for the procedure afterward. c. Offer a brief, concrete explanation of the procedure at the patient’s level and with the parent or caregiver present. d. Prepare the child in advance with details about the procedure without the parent or caregiver present. ANS: C For a 4-year-old child, offering a brief, concrete explanation about a procedure just beforehand, with the parent or caregiver present, is appropriate. The other options are incorrect for any age group. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 39 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 1. Which statements are true regarding pediatric patients and pharmacokinetics? (Select all that apply.) a. The levels of microsomal enzymes are decreased. b. Perfusion to the kidneys may be decreased and may result in reduced renal function. c. First-pass elimination is increased because of higher portal circulation. d. First-pass elimination is reduced because of the immaturity of the liver. e. Total body water content is much less than in adults. f. Gastric emptying is slowed because of slow or irregular peristalsis. g. Gastric emptying is more rapid because of increased peristaltic activity. ANS: A, B, D, F In children, first-pass elimination by the liver is reduced because of the immaturity of the liver, and microsomal enzymes are decreased. In addition, gastric emptying is reduced because of slow or irregular peristalsis. Perfusion to the kidneys may be decreased, resulting in reduced renal function. The other options are incorrect. In addition, remember that total body water content is greater in children than in adults. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 38 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Health Promotion and Maintenance 2. Which statements are true regarding the elderly and pharmacokinetics? (Select all that apply.) a. The levels of microsomal enzymes are decreased. b. Fat content is increased because of decreased lean body mass. c. Fat content is decreased because of increased lean body mass. d. The number of intact nephrons is increased. e. The number of intact nephrons is decreased. f. Gastric pH is less acidic. g. Gastric pH is more acidic. ANS: A, B, E, F In the elderly, levels of microsomal enzymes are decreased because the aging liver is less able to produce them; fat content is increased because of decreased lean body mass; the number of intact nephrons is decreased as the result of aging; and gastric pH is less acidic because of a gradual reduction of the production of hydrochloric acid. The other options are incorrect statements. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 41 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Health Promotion and Maintenance COMPLETION 1. A 7-year-old child will be receiving amoxicillin (Amoxil) 80 mg/kg/day in two divided doses. The child weighs 55 pounds. The medication, once reconstituted, is available as an oral suspension of 50 mg/mL. Identify how many milliliters will the child receive per dose. _______ ANS: 20 mL Convert pounds to kilograms: 55 pounds = 25 kg. To get the amount per dose, divide 2000 by 2, which equals 1000 mg/dose. To calculate the milliliters: DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 04: Cultural, Legal, and Ethical Considerations Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. During the development of a new drug, which would be included in the study by the researcher to prevent any bias or unrealistic expectations of the new drug’s usefulness? a. A placebo b. FDA approval c. Informed consent d. Safety information ANS: A To prevent bias that may occur as a result of unrealistic expectations of an investigational new drug, a placebo is incorporated into the study. The other options are incorrect. FDA approval, if given, does not occur until after phase III. Informed consent is required in all drug studies. Safety information is not determined until the study is under way. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 55 TOP: NURSING PROCESS: General MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 2. A member of an investigational drug study team is working with healthy volunteers whose participation will help to determine the optimal dosage range and pharmacokinetics of the drug. The team member is participating in what type of study? a. Phase I b. Phase II c. Phase III d. Phase IV ANS: A Phase I studies involve small numbers of healthy volunteers to determine optimal dosage range and the pharmacokinetics of the drug. The other phases progressively involve volunteers who have the disease or ailment that the drug is designed to diagnose or treat. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 55 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. During discharge patient teaching, the nurse reviews prescriptions with a patient. Which statement is correct about refills for an analgesic that is classified as Schedule C-III? a. No prescription refills are permitted. b. Refills are allowed only by written prescription. c. The patient may have no more than five refills in a 6-month period. d. Written prescriptions expire in 12 months. ANS: C Schedule C-III medications may be refilled no more than five times in a 6-month period. The patient should be informed of this regulation. No prescription refills are permitted for Schedule C-II drugs. Requiring refills by written prescription only applies to Schedule C-II drugs. Schedule C-III prescriptions (written or oral) expire in 6 months. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 54 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A patient has been selected as a potential recipient of an experimental drug for heart failure. The nurse knows that when informed consent has been obtained, it indicates which of these? a. The patient has been informed of the possible benefits of the new therapy. b. The patient will be informed of the details of the study as the research continues. c. The patient will receive the actual drug during the experiment. d. The patient has had the study’s purpose, procedures, and the risks involved explained to him. ANS: D Informed consent involves the careful explanation of the purpose of the study, the procedures to be used, and the risks involved. The other options do not describe informed consent. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 55 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 5. For which cultural group must the health care provider respect the value placed on preserving harmony with nature and the belief that disease is a result of ill spirits? a. Hispanics b. Asian Americans c. Native Americans d. African Americans ANS: C Some Native Americans believe in preserving harmony with nature and that disease is a result of ill spirits. The groups listed in the other options do not typically reflect these practices. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 51 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Psychosocial Integrity 6. The nurse is assessing an elderly Hispanic woman who is being treated for hypertension. During the assessment, what is important for the nurse to remember about cultural aspects? a. The patient should be discouraged from using folk remedies and rituals. b. The nurse will expect the patient to value protective bracelets and “root workers” as healers. c. The nurse will remember that the balance among body, mind, and environment is important for this patient’s health beliefs. d. The nurse’s assessment needs to include gathering information regarding religious practices and beliefs regarding medication, treatment, and healing. ANS: D All beliefs need to be considered clearly so as to prevent a conflict from arising between the goals of nursing and health care and the dictates of a patient’s cultural background. Assessing religious practices and beliefs is part of a thorough cultural assessment. The other options are incorrect. The nurse should not ignore a patient’s cultural practices. The concept of balance among body, mind, and environment and the valuing of protective bracelets and root workers reflect beliefs or practices that usually do not apply to the Hispanic cultural group. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 52 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Psychosocial Integrity 7. When reviewing the various schedules of controlled drugs, the nurse knows that which description correctly describes Schedule II drugs? a. Drugs with high potential for abuse that have accepted medical use b. Drugs with high potential for abuse that do not have accepted medical use c. Medically accepted drugs that may cause moderate physical or psychologic dependence d. Medically accepted drugs with limited potential for causing physical or psychologic dependence ANS: A Schedule II drugs are those with high potential for abuse but that have accepted medical use. Drugs that have high potential for abuse but do not have accepted medical use are Schedule I drugs. Medically accepted drugs that may cause moderate physical or psychologic dependence are Schedule III drugs. Medically accepted drugs with limited potential for causing physical or psychologic dependence are Schedule IV and V drugs. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 54 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. The nurse is reviewing facts about pharmacology for a review course. The term legend drug refers to which item? a. Over-the-counter drugs b. Prescription drugs c. Orphan drugs d. Older drugs ANS: B The term legend drug refers to prescription drugs, which were differentiated from over-the-counter drugs by the 1951 Durham-Humphrey Amendment. Orphan drugs are drugs that are developed for rare diseases. The other options are not examples of legend drugs. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 53 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. Nurses have the ethical responsibility to tell the truth to their patients. What is this principle known as? a. Justice b. Veracity c. Beneficence d. Autonomy ANS: B Veracity is defined as the duty to tell the truth. Justice is the ethical principle of being fair or equal in one’s actions. Beneficence is the ethical principle of doing or actively promoting good. Autonomy is self-determination, or the ability to make one’s own decisions. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 57 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 10. A patient is undergoing major surgery and asks the nurse about a living will. He states, “I don’t want anybody else making decisions for me. And I don’t want to prolong my life.” The patient is demonstrating which ethical term? a. Autonomy b. Beneficence c. Justice d. Veracity ANS: A Autonomy includes self-determination, or the ability to act on one’s own, including making one’s own decisions about health care. Veracity is defined as the duty to tell the truth. Justice is the ethical principle of being fair or equal in one’s actions. Beneficence is the ethical principle of doing or actively promoting good. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 57 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is reviewing a list of scheduled drugs and notes that Schedule C-I drugs are not on the list. Which is a characteristic of Schedule C-I drugs? a. No refills are permitted. b. They may be obtained over-the-counter with a signature. c. They are available only by written prescription. d. They are used only with approved protocols. ANS: D Schedule C-I drugs are used only with approved protocols. Schedule C-II drugs are available only by written prescription, and refills are not permitted. Being available over-the-counter with a signature may be true of Schedule C-V drugs in certain states. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 54 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. During a busy night shift, a new nurse administered an unfamiliar medication without checking it in a drug handbook. Later that day, the patient had a severe reaction because he has renal problems, which was a contraindication to that drug. The nurse may be liable for which of these? a. Medical negligence b. Nursing negligence c. Nonmaleficence d. Autonomy ANS: B Negligence is the failure to act in a reasonable and prudent manner or failure of the nurse to give the care that a reasonably prudent (cautious) nurse would render or use under similar circumstances. In this case, nursing negligence applies to nurses, not medical negligence. Nonmaleficence is defined as the duty to do no harm; autonomy is defined as the right to make one’s own decisions, or self-determination. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 57 TOP: NURSING PROCESS: General MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control MULTIPLE RESPONSE 1. The nurse is reviewing the concept of drug polymorphism. Which factors contribute to drug polymorphism? (Select all that apply.) a. The number of drugs ordered by the physician b. Inherited factors c. The patient’s diet and nutritional status d. Different dosage forms of the same drug e. The patient’s health beliefs and practices f. The patient’s drug history g. The various available forms of a drug ANS: B, C, E Inherited factors, diet and nutritional status, and health beliefs and practices are some of the factors that contribute to drug polymorphism. The other options are not factors that contribute to drug polymorphism. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 51 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The nurse is performing an admission assessment. Which findings reflect components of a cultural assessment? (Select all that apply.) a. The patient uses aspirin as needed for pain. b. The patient has a history of hypertension. c. The patient uses herbal tea to relax in the evenings. d. The patient does not speak English. e. The patient is allergic to shellfish. f. The patient does not eat pork products for religious reasons. ANS: A, C, D, F The past use of medicines, use of herbal treatments, languages spoken, and religious practices and beliefs are components of a cultural assessment. The other options reflect components of a general medication assessment or health history. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 52 TOP: NURSING PROCESS: Assessment Chapter 05: Medication Errors: Preventing and Responding Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is reviewing medication errors. Which situation is an example of a medication error? a. A patient refuses her morning medications. b. A patient receives a double dose of a medication because the nurse did not cut the pill in half. c. A patient develops hives after having started an IV antibiotic 24 hours earlier. d. A patient complains of severe pain still present 60 minutes after a pain medication was given. ANS: B A medication error is defined as a preventable adverse drug event that involves inappropriate medication use by a patient or health care provider. The other options are not preventable. The patient’s refusing to take medications and complaining of pain after a medication is given are patient behaviors, and the development of hives is a possible allergic reaction. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 67 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 2. The nurse is reviewing a list of verbal medication orders. Which is the proper notation of the dose of the drug ordered? a. Digoxin .125 mg b. Digoxin .1250 mg c. Digoxin 0.125 mg d. Digoxin 0.1250 mg ANS: C Digoxin 0.125 mg illustrates the correct notation with a leading zero before the decimal point. Omitting the leading zero may cause the order to be misread, resulting in a large drug overdose. Digoxin .125 mg and digoxin .1250 mg do not have the leading zero before the decimal point. Digoxin 0.1250 mg has a trailing zero, which also is incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 69 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care 3. When given a scheduled morning medication, the patient states, “I haven’t seen that pill before. Are you sure it’s correct?” The nurse checks the medication administration record and verifies that it is listed. Which is the nurse’s best response? a. “It’s listed here on the medication sheet, so you should take it.” b. “Go ahead and take it, and then I’ll check with your doctor about it.” c. “It wouldn’t be listed here if it were not ordered for you!” d. “Let me check on the order first before you take it.” ANS: D When giving medications, the nurse should always listen to and honor any concerns or doubts expressed by the patient. If the patient doubts an order, the nurse should check the written order and/or check with the prescriber. The other options illustrate that the nurse is not listening to the patient’s concerns. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 69 TOP: NURSING PROCESS: Planning MSC: NCLEX: Safe and Effective Care Environment: Management of Care 4. During a period of time when the computerized medication order system was down, the prescriber wrote admission orders, and the nurse is transcribing them. The nurse is having difficulty transcribing one order because of the prescriber’s handwriting. Which is the best action for the nurse to take at this time? a. Ask a colleague what the order says. b. Contact the prescriber to clarify the order. c. Wait until the prescriber makes rounds again to clarify the order. d. Ask the patient what medications he takes at home. ANS: B If a prescriber writes an order that is illegible, the nurse should contact the prescriber for clarification. Asking a colleague is not useful because the colleague did not write the order. Waiting for the prescriber to return is incorrect because it would delay implementation of the order. Asking the patient about medications is incorrect because this question will not clarify the current order written by the prescriber. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 69 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 5. When taking a telephone order for a medication, which action by the nurse is most appropriate? a. Verify the order with the charge nurse. b. Call back the prescriber to review the order. c. Repeat the order to the prescriber before hanging up the telephone. d. Ask the pharmacist to double-check the order. ANS: C For telephone or verbal orders, repeat the order back to the prescriber before hanging up the telephone. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 69 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care MULTIPLE RESPONSE 1. The nurse can prevent medication errors by following which principles? (Select all that apply.) a. Assess for allergies after giving medications. b. Use two patient identifiers before giving medications. c. Do not give a medication that another nurse has drawn up in a syringe. d. Minimize the use of verbal and telephone orders. e. Use trade names instead of generic names to avoid confusion. ANS: B, C, D Measures that prevent medication errors include using two patient identifiers, giving only medications that you have drawn up or prepared, and minimizing the use of verbal and telephone orders. Assessment for allergies should be done before medications are given. Generic names should be used to avoid the many sound-alike trade names of medications. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 69 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 1. Levothyroxine is available in 88-mcg tablet form. Convert this dose to milligram strength. (do not round) _______ ANS: 0.088 mg One mg equals 1000 mcg. To convert 88 mcg to mg, divide 88 by 1000 to equal 0.088 mg, or move the decimal point to the left three spaces. Do not forget to include the leading zero. DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. Digoxin is available in 0.125-mg tablet form. Convert this dose to microgram strength. (do not round) _______ ANS: 125 mcg One mg equals 1000 mcg. To convert 0.125 mg to mcg, multiply by 1000 to equal 125 mcg, or move the decimal point to the right three spaces. DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 06: Patient Education and Drug Therapy Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. Which nursing diagnosis is appropriate for the patient who has just received a prescription for a new medication? a. Noncompliance related to new drug therapy b. Impaired memory related to new drug therapy c. Lack of knowledge regarding newly prescribed drug therapy d. Deficient knowledge related to newly prescribed drug therapy ANS: D A patient who has a limited understanding of newly prescribed drug therapy may have the nursing diagnosis of deficient knowledge. Noncompliance is incorrect because that term implies that the patient does not follow a recommended regimen, which is not the case with a newly prescribed drug. Impaired memory is not appropriate in this situation. “Lack of knowledge” is not a nursing diagnosis. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 77 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Safe and Effective Care Environment: Management of Care 2. The nurse is developing a care plan for a patient who will be self-administering insulin injections. Which statement reflects a measurable outcome? a. The patient will know about self-administration of insulin injections. b. The patient will understand the principles of self-administration of insulin injections. c. The patient will demonstrate the proper technique of self-administering insulin injections. d. The patient will comprehend the proper technique of self-administering insulin injections. ANS: C The word demonstrate is a measurable verb, and measurable terms should be used when developing goals and outcome criteria statements. The other options are incorrect because the terms know, understand, and comprehend are not measurable terms. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 77 TOP: NURSING PROCESS: Planning MSC: NCLEX: Safe and Effective Care Environment: Management of Care 3. During a nursing assessment, which question by the nurse allows for greater clarification and additional discussion with the patient? a. “Are you allergic to penicillin?” b. “What medications do you take?” c. “Have you had a reaction to this drug?” d. “Are you taking this medication with meals?” ANS: B Asking “What medications do you take?” is an open-ended question that will encourage greater clarification and additional discussion with the patient. The other options are examples of closed-ended questions, which prompt only a “yes” or “no” answer and provide limited information. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 77 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care 4. The nurse is setting up a teaching session with an 85-year-old patient who will be going home on anticoagulant therapy. Which educational strategy would reflect consideration of the age-related changes that may exist with this patient? a. Show a video about anticoagulation therapy. b. Present all the information in one session just before discharge. c. Give the patient pamphlets about the medications to read at home. d. Develop large-print handouts that reflect the verbal information presented. ANS: D Developing large-print handouts addresses altered perception in two ways. First, by using visual aids to reinforce verbal instructions, one addresses the possibility of decreased ability to hear high-frequency sounds. By developing the handouts in large print, one addresses the possibility of decreased visual acuity. Showing a video does not allow discussion of the information; furthermore, the text and print may be small and difficult to read and understand. Presenting all the information in one session before discharge also does not allow for discussion, and the patient may not be able to hear or see the information sufficiently. Because of the possibility of decreased short-term memory and slowed cognitive function, giving pamphlets to read may not be appropriate. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 79 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Health Promotion and Maintenance 5. When the nurse teaches a skill such as self-injection of insulin to the patient, what is the best way to set up the teaching/learning session? a. Provide written pamphlets for instruction. b. Show a video, and allow the patient to practice as needed on his own. c. Verbally explain the procedure, and provide written handouts for reinforcement. d. After demonstrating the procedure, allow the patient to do several return demonstrations. ANS: D Return demonstration allows the nurse to evaluate the patient’s newly learned skills. The techniques in the other options are incorrect because those suggestions do not allow for evaluation of the patient’s technique. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 75 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 6. A patient with a new prescription for a diuretic has just reviewed with the nurse how to include more potassium in her diet. This reflects learning in which domain? a. Cognitive b. Affective c. Physical d. Psychomotor ANS: A The cognitive domain refers to problem-solving abilities and may involve recall and knowledge of facts. The affective domain refers to values and beliefs. The term physical does not refer to one of the learning domains. The psychomotor domain involves behaviors such as learning how to perform a procedure. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 75 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 7. During an admission assessment, the nurse discovers that the patient does not speak English. Which is considered the ideal resource for translation? a. A family member of the patient b. A close family friend of the patient c. A translator who does not know the patient d. Prewritten note cards with both English and the patient’s language ANS: C The nurse should communicate with the patient in the patient’s native language if at all possible. If the nurse is not able to speak the patient’s native language, a translator should be made available so as to prevent communication problems, minimize errors, and help boost the patient’s level of trust and understanding of the nurse. In practice, this translator may be another nurse or health care professional, a nonprofessional member of the health care team, or a layperson, family member, adult friend, or religious leader or associate. However, it is best to avoid family members as translators, if possible, because of issues with bias, misinterpretation, and potential confidentiality issues. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 78 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 8. The nurse is teaching a 16-year-old patient who has a new diagnosis of type 1 diabetes about blood glucose monitoring and the importance of regulating glucose intake. When developing a teaching plan for this teenager, which of Erikson’s stages of development should the nurse consider? a. Trust versus mistrust b. Intimacy versus isolation c. Industry versus inferiority d. Identity versus role confusion ANS: D According to Erikson, the adolescent (12 to 18 years of age) is in the identity versus role confusion stage of development. Trust versus mistrust reflects the infancy stage; intimacy versus isolation reflects the young adulthood stage; and industry versus inferiority reflects the school-age stage of development. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 76 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Psychosocial Integrity 9. A 60-year-old patient is on several new medications and expresses worry that she will forget to take her pills. Which action by the nurse would be most helpful in this situation? a. Teaching effective coping strategies b. Asking the patient’s prescriber to reduce the number of drugs prescribed c. Assuring the patient that she will not forget once she is accustomed to the routine d. Assisting the patient with obtaining and learning to use a calendar or pill container ANS: D Calendars, pill containers, or diaries may be helpful to patients who may forget to take prescribed drugs as scheduled. The nurse must ensure that the patient knows how to use these reminder tools. Teaching coping strategies is a helpful suggestion but will not help with remembering to take medications. Asking the prescriber to reduce the number of drugs that are prescribed is not an appropriate action by the nurse. Assuring the patient that she will not forget is false reassurance by the nurse and inappropriate when education is needed. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 78 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 1. Which are appropriate considerations when the nurse is assessing the learning needs of a patient? (Select all that apply.) a. Cultural background b. Family history c. Level of education d. Readiness to learn e. Health beliefs ANS: A, C, D, E Family history is not a part of what the nurse considers when assessing learning needs. The other options are appropriate to consider when the nurse is assessing learning needs. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: pp. 75-77 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care COMPLETION 1. A patient is to receive prednisone 7.5 mg PO daily. The tablets are available in a 2.5- mg strength. Identify how many tablets will the patient receive. _______ ANS: 3 tablets Chapter 07: Over-the-Counter Drugs and Herbal and Dietary Supplements Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A 25-year-old woman is visiting the prenatal clinic and shares with the nurse her desire to go “natural” with her pregnancy. She shows the nurse a list of herbal remedies that she wants to buy so that she can “avoid taking any drugs.” Which statement by the nurse is correct? a. “Most herbal remedies are not harmful and are safe for use during pregnancy.” b. “Please read each label carefully before use to check for cautionary warnings.” c. “Keep in mind that products from different manufacturers are required to contain consistent amounts of the herbal products.” d. “It’s important to remember that herbal remedies do not have proven safety ratings for pregnant women.” ANS: D The fact that a drug is an herbal or a dietary supplement does not mean that it can be safely administered to children, infants, or pregnant or lactating women. Many herbal products have not been tested for safety during pregnancy. Simply reading the labels may not provide enough information for use during pregnancy. Last, manufacturers of herbal products are not required to guarantee the reliability of the contents. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 93 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. The patient is asking the nurse about current U.S. laws and regulations of herbal products. According to the Dietary Supplement and Health Education Act of 1994, which statement is true? a. Medicinal herbs are viewed as dietary supplements. b. Herbal remedies are held to the same standards as drugs. c. Producers of herbal products must prove therapeutic efficacy. d. Herbal remedies are protected by patent laws. ANS: A Current U.S. laws view herbal products as dietary supplements and do not hold them to the same efficacy standards as drugs. The other options do not correctly reflect current U.S. laws regarding herbal supplements. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 89 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. The patient wants to take the herb valerian to help him rest at night. The nurse would be concerned about potential interactions if he is taking a medication from which class of drugs? a. Digitalis b. Anticoagulants c. Sedatives d. Immunosuppressants ANS: C Valerian may cause increased central nervous system depression if used with sedatives. Digitalis, anticoagulants, and immunosuppressants do not have interactions with valerian. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 90 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. The patient has been taking an over-the-counter (OTC) acid-reducing drug because he has had “stomach problems” for several months. He tells the nurse that the medicine helps as long as he takes it, but once he stops it, the symptoms return. Which statement by the nurse is the best advice for this patient? a. “The over-the-counter drug has helped you, so you should continue to take it.” b. “The over-the-counter dosage may not be strong enough. You should be taking prescription-strength for best effects.” c. “For best results, you need to watch what you eat in addition to taking this drug.” d. “Using this drug may relieve your symptoms, but it does not address the cause. You should be seen by your health care provider.” ANS: D The use of OTC drugs may postpone effective management of chronic disease states and may delay treatment of serious or life-threatening disorders because these drugs may relieve symptoms without necessarily addressing the cause of the disorder. The other options do not address the need to investigate the cause of the symptoms and are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 87 TOP: NURSING PROCESS: Planning MSC: NCLEX: Safe and Effective Care Environment: Management of Care 5. During an assessment, the patient tells the nurse that he eats large amounts of garlic for its cardiovascular benefits. Which drug or drug class, if taken, would have a potential interaction with the garlic? a. Acetaminophen (Tylenol) b. Insulin c. Antilipemic drugs d. Sedatives ANS: B The use of garlic may interfere with hypoglycemic drugs. The other options are incorrect because acetaminophen, antilipemic drugs, and sedatives do not have interactions with garlic. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 90 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A patient calls the clinic to ask about taking cranberry dietary supplement capsules because a friend recommended them. The nurse will discuss which possible concern when a patient is taking cranberry supplements? a. It may increase the risk for bleeding if the patient is taking anticoagulants. b. It may increase the risk of toxicity of some psychotherapeutic drugs. c. It may reduce elimination of drugs that are excreted by the kidneys. d. Cranberry may increase the intensity and duration of effects of caffeine. ANS: C The use of cranberry decreases the elimination of many drugs that are renally excreted. The other concerns do not occur with cranberry supplements. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 90 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. A patient wants to take the herb gingko to help his memory. The nurse reviews his current medication list and would be concerned about potential interactions if he is taking a medication from which class of drugs? a. Digitalis b. Anticoagulants c. Sedatives d. Immunosuppressants ANS: B The use of gingko increases the risk of bleeding with anticoagulants (warfarin, heparin) and antiplatelets (aspirin, clopidogrel). The other concerns do not occur with gingko supplements. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 90 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 1. The nurse is conducting a class for senior citizens about the use of over-the-counter (OTC) drugs. Which statements are true regarding the use of OTC drugs? (Select all that apply.) a. Use of OTC drugs may delay treatment of serious ailments. b. Drug interactions with OTC medications are rare. c. OTC drugs may relieve symptoms without addressing the cause of the problem. d. OTC drugs are indicated for long-term treatment of conditions. e. Patients may misunderstand product labels and use the drugs improperly. ANS: A, C, E It is true that use of OTC drugs may delay treatment of serious ailments; OTC drugs may relieve symptoms without addressing the cause of the problem, and patients may misunderstand product labels and use the drugs improperly. These statements should be included when teaching patients about their use. In contrast, drug interactions with OTC medications are not rare and may indeed occur with prescription medications and other OTC drugs. Normally, OTC drugs are intended for short-term treatment of minor ailments. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 86-88 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The nurse is reviewing the criteria for over-the-counter drugs. Which criteria for over-the-counter status in the United States are accurate? (Select all that apply.) a. The drug must be easy to use. b. The drug must have a low therapeutic index. c. The consumer must be able to monitor the drug’s effectiveness. d. The drug must have a low potential for abuse. e. The drug must not have any interactions with other drugs. ANS: A, C, D In the United States, criteria for over-the-counter status include the drug being easy to use, the drug having a low potential for abuse, and the consumer must be able to monitor the drug’s effectiveness for the condition. The drug must have a high therapeutic index (not a low one), and the drug must have limited interactions with other drugs. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 87 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 08: Gene Therapy and Pharmacogenomics Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is reviewing the applications of gene therapy. Which drug is manufactured as a result of indirect gene therapy? a. Vitamin K b. Warfarin c. Human insulin d. Heparin ANS: C A recombinant form of human insulin is one of the most widespread uses of indirect gene therapy. Other examples include hormones, vaccines, antitoxins, and monoclonal antibodies. The other options listed are not examples of drugs manufactured by indirect gene therapy. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 98 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The nurse is discussing gene therapy in a continuing education class. Which is the best definition of eugenics? a. The use of gene therapy to prevent disease b. The development of new drugs based on gene therapy c. Intentional selection, before birth, of genotypes that are considered more desirable than others d. The determination of genetic factors that influence a person’s response to medications ANS: C Eugenics is the intentional selection of genotypes, before birth, that are considered more desirable than others, and it is a major ethical issue concerning gene therapy. The other options do not describe eugenics. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 99 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 3. The nurse is explaining the Human Genome Project to colleagues. Which of these is the main purpose of the Human Genome Project? a. The study of genetic diseases. b. The study of genetic traits in humans. c. The discovery new genetic diseases. d. To describe the entire genome of a human being. ANS: D The Human Genome Project was undertaken to describe in detail the entire genome of a human being. The other options do not describe the Human Genome Project. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 98 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A patient has just been told that she has the genetic markers for a severe type of breast cancer. After the patient meets with the physician, the patient’s daughter asks the nurse, “What did the doctor tell my mother? She seems upset.” What is the nurse’s best response? a. “I’m sorry, but I’m not allowed to discuss that.” b. “The physician will discuss this with you.” c. “It seems that your mother has the genetic markers for a type of breast cancer.” d. “This is information that your mother will need to discuss with you.” ANS: D Maintaining privacy and confidentiality is of utmost importance during genetic testing and counseling. The patient (not the nurse or the physician) is the one who decides whether to include or exclude any family members from the discussion and from knowledge of the results of genetic testing. Telling the patient’s daughter that you are “not allowed” to discuss the matter would cause more anxiety. Telling the daughter about the genetic markers would be a violation of the patient’s privacy. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 100-101 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is asking a patient about his family history as part of an assessment. Which component is included in an effective family history? a. Asking the patient about the current and past health status of the patient’s children b. Covering at least three generations of family history c. Obtaining a family history of the patient’s spouse d. Asking about the family history for the patient’s siblings and parents only ANS: B The family history is most effective if it covers at least three generations and includes the current and past health status of each family member. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 100 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 1. The nurse is performing an assessment of a patient. Which assessment findings may indicate a higher risk for genetic disorders? (Select all that apply.) a. The patient’s father was diagnosed with heart disease at 60 years of age. b. The patient’s mother was diagnosed with breast cancer at 33 years of age. c. The patient’s grandfather died of a cerebral vascular accident at 78 years of age. d. The patient’s sister has a history of both renal and lung cancer. e. The patient has two uncles and a grandparent who have been diagnosed with Alzheimer’s disease. ANS: B, D, E The nurse should assess for factors that may indicate a risk for genetic disorders. A few examples of factors that may indicate a risk for genetic disorders are a higher incidence of a particular disease or disorder in the patient’s family than in the general population; diagnosis of a disease in family members at an unusually young age; or diagnosis of a family member with an unusual form of cancer or with more than one type of cancer. The options regarding heart disease at 60 years of age and cerebral vascular accident at 78 years of age are not factors that indicate a higher risk for genetic disorders. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 100 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential Chapter 09: Photo Atlas of Drug Administration Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. Before administering any medication, what is the nurse’s priority action regarding patient safety? a. Verifying orders with another nurse b. Documenting the medications given c. Counting medications in the medication cart drawers d. Checking the patient’s identification using two identifiers ANS: D Verifying the patient’s identity, using two identifiers, before administering any medication is essential for the patient’s safety and reflects checking one of the “Nine Rights” of medication administration. Documentation is done after the medications are given. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 104-105 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 2. The nurse is giving an intradermal (ID) injection and will choose which syringe for this injection? a. b. c. d. ANS: B The proper size syringe for ID injection is 1-mL tuberculin. The other syringes pictured are incorrect. Insulin syringes (marked in units) are not used for intradermal injections. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: pp. 116-117 TOP: NURSING PROCESS: Planning MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 3. A patient is to receive a penicillin intramuscular (IM) injection in the ventrogluteal site. The nurse will use which angle for the needle insertion? a. 15 degrees b. 45 degrees c. 60 degrees d. 90 degrees ANS: D The proper angle for IM injections is 90 degrees. The other angles are incorrect. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 116 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. When administering medication by IV bolus (push), the nurse will occlude the IV line by which method? a. Not pinching the IV tubing at all b. Pinching the tubing just above the injection port c. Pinching the tubing just below the injection port d. Pinching the tubing just above the drip chamber of the infusion set ANS: B Before a medication is injected by IV push, the IV line is occluded by pinching the tubing just above the injection port. The other locations are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 128 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. The nurse has an order to administer an intramuscular (IM) immunization to a 2-month-old child. Which site is considered the best choice for this injection? a. Deltoid b. Dorsogluteal c. Ventrogluteal d. Vastus lateralis ANS: D The vastus lateralis is the preferred site of injection of drugs such as immunizations for infants. The other sites are not appropriate for infants. The ventrogluteal site is the preferred site for adults and children. The deltoid site is used only for the administration of immunizations to toddlers, older children, and adults (not infants) and only for small volumes of medication. The dorsogluteal site is no longer recommended because of the possibility of nerve injury. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 122 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. The nurse needs to administer insulin subcutaneously to an obese patient. Which is the proper technique for this injection? a. Using the Z-track method b. Inserting the needle at a 5- to 15-degree angle until resistance is felt c. Pinching the skin at the injection site, and then inserting the needle to below the tissue fold at a 90-degree angle d. Spreading the skin tightly over the injection site, inserting the needle, and then releasing the skin ANS: C The proper technique for a subcutaneous injection for an obese patient is to pinch the skin at the site and inject the needle to below the skin fold at a 90-degree angle. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 116 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. The nurse will plan to use the Z-track method of intramuscular (IM) injections for which situation? a. The medication is known to be irritating to tissues. b. The patient is emaciated and has very little muscle mass. c. The medication must be absorbed quickly into the tissues. d. The patient is obese and has a deep fat layer below the muscle mass. ANS: A The Z-track method is used for medications known to irritate tissues or for medications that are painful or cause stains to the tissues. It also prevents the deposit of medication into more sensitive subcutaneous tissues. The other options are not appropriate situations for the Z-track method. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 120 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 8. After administering an intradermal (ID) injection for a skin test, the nurse notices a small bleb at the injection site. The best action for the nurse to take at this time is to: a. apply heat. b. massage the area. c. do nothing. d. report the bleb to the physician. ANS: C The formation of a small bleb is expected after an ID injection for skin testing. The other actions are not appropriate. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 116 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The nurse is administering an IV push medication through an IV lock. After injecting the medication, which action will be taken next? a. Flushing the lock b. Regulating the IV flow c. Clamping the tubing for 10 minutes d. Holding the patient’s arm up to improve blood flow ANS: A IV locks are to be flushed before and after each use; either heparin or saline flush is used, depending on the individual institution’s policy. The other actions are not appropriate. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 128 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. When adding medications to a bag of intravenous (IV) fluid, the nurse will use which method to mix the solution? a. Shaking the bag or bottle vigorously b. Turning the bag or bottle gently from side to side c. Inverting the bag or bottle one time after injecting the medication d. Allowing the IV solution to stand for 10 minutes to enhance even distribution of medication ANS: B When medications are added to IV fluid containers, the medication and the IV solution are mixed by holding the bag or bottle and turning it end-to-end, mixing it gently. Shaking vigorously is not appropriate; inverting the bag just once or simply allowing the bag to stand for 10 minutes may not be sufficient to mix the medication into the fluid. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 124 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. The nurse is measuring 4 mL of a liquid cough elixir for a child. Which method is most appropriate? a. Using a teaspoon to measure and administer b. Holding the medication cup at eye level and filling it to the desired level c. Withdrawing the elixir from the container using a syringe without a needle attached d. Withdrawing the elixir from the container using a calibrated oral syringe ANS: D Small doses of liquid medications must be withdrawn using a calibrated oral syringe. A hypodermic syringe or a syringe with a needle or syringe cap must not be used. If hypodermic syringes are used, the drug may be inadvertently given parenterally, or the syringe cap or needle, if not removed from the syringe, may become dislodged and accidentally aspirated by the patient when the syringe plunger is pressed. The other methods are not accurate for small volumes. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 109 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. While the nurse is assisting a patient in taking his medications, the medication cup falls to the floor, spilling the tablets. What is the nurse’s best action at this time? a. Discarding the medications and repeating preparation b. Asking the patient if he will take the medications c. Waiting until the next dose time, and then giving the medications d. Retrieving the medications and administering them to avoid waste ANS: A Medications that fall to the floor must be discarded, and the procedure must be repeated with new medications. The other actions are not appropriate. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 105 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 13. When giving a buccal medication to a patient, which action by the nurse is appropriate? a. Encouraging the patient to swallow, if necessary b. Administering water after the medication has been given c. Placing the medication between the upper or lower molar teeth and the cheek d. Placing the tablet under the patient’s tongue and allowing it to dissolve completely ANS: C Buccal medications are properly administered between the upper or lower molar teeth and the cheek. Caution the patient against swallowing, and do not administer with water. Medications given under the tongue are sublingually administered. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 106 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 14. The nurse is giving medications through a percutaneous endoscopic gastrostomy (PEG) tube. Which technique is correct? a. Administering the medications using a 3-mL medication syringe b. Applying firm pressure on the syringe’s piston to infuse the medication c. Flushing the tubing with 30 mL of saline after the medication has been given d. Using the barrel of the syringe, allowing the medication to flow via gravity into the tube ANS: D For PEG tubes (and nasogastric tubes), medications are poured into the barrel of the syringe with the piston removed, and the medication is allowed to flow via gravity into the tube. Fluid must never be forced into the tube. The tubing is to be flushed with 30 mL of tap water (not saline) to ensure that the medication is cleared from the tube after the medication has been given. A 3-mL syringe is too small for this procedure. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 110 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 15. The nurse is about to give a rectal suppository to a patient. Which technique would facilitate the administration and absorption of the rectal suppository? a. Having the patient lie on his or her right side, unless contraindicated b. Having the patient hold his or her breath during insertion of the medication c. Lubricating the suppository with a small amount of petroleum-based lubricant before insertion d. Encouraging the patient to lie on his or her left side for 15 to 20 minutes after insertion ANS: D Position the patient on his or her left side for rectal suppository insertion. The suppository is then lubricated with a small amount of water-soluble lubricant, not petroleum-based substances. The patient is told to take a deep breath and exhale through the mouth during insertion. Then the patient needs to remain lying on the left side for 15 to 20 minutes to allow absorption of the drug. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 111 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 16. A patient is receiving eyedrops that contain a beta-blocker medication. The nurse will use what method to reduce systemic effects after administering the eyedrops? a. Wiping off excess liquid immediately after instilling the drops b. Having the patient close the eye tightly after the drops are instilled c. Having the patient try to keep the eye open for 30 seconds after the drops are instilled d. Applying gentle pressure to the patient’s nasolacrimal duct for 30 to 60 seconds after instilling the drops ANS: D When administering ophthalmic drugs that may cause systemic effects, one’s finger should be protected by a clean tissue or glove and gentle pressure applied to the patient’s nasolacrimal duct for 30 to 60 seconds. The other actions are not appropriate. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 130 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 17. A 2-year-old child is to receive eardrops. The nurse is teaching the parent about giving the eardrops. Which statement reflects the proper technique for administering eardrops to this child? a. Administer the drops without pulling on the ear lobe. b. Straighten the ear canal by pulling the lobe upward and back. c. Straighten the ear canal by pulling the pinna down and back. d. Straighten the ear canal by pulling the pinna upward and outward. ANS: C In an infant or a child younger than 3 years of age, the ear canal is straightened by pulling the pinna down and back. In adults, the pinna is pulled up and outward. Pulling the lobe and administering eardrops without pulling on the ear lobe are not appropriate actions. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 131 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 18. A patient with asthma is to begin medication therapy using a metered-dose inhaler. What is an important reminder to include during teaching sessions with the patient? a. Repeat subsequent puffs, if ordered, after 5 minutes. b. Inhale slowly while pressing down to release the medication. c. Inhale quickly while pressing down to release the medication. d. Administer the inhaler while holding it 3 to 4 inches away from the mouth. ANS: B Position the inhaler to an open mouth, with the inhaler 1 to 2 inches away from the mouth, or attach a spacer to the mouthpiece of the inhaler, or place the mouthpiece in the mouth. To administer, press down on the inhaler to release the medication while inhaling slowly. Wait 1 to 2 minutes between puffs if a second puff of the same medication has been ordered. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 132 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 19. When giving medications, the nurse will use Standard Precautions, which include what action? a. Bending the needle to prevent reuse b. Recapping needles to prevent needle sticks c. Discarding all syringes and needles in the trash can d. Discarding all syringes and needles in a puncture-resistant container ANS: D Standard Precautions include wearing clean gloves when there is potential exposure to a patient’s blood or other body fluids; never recapping needles; never bending needles or syringes; and discarding all disposable syringes and needles in the appropriate puncture-resistant container. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 108 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 20. A patient says he prefers to chew rather than swallow his pills. One of the pills has the abbreviation SR behind the name of the medication. The nurse needs to remember which correct instruction regarding how to give this medication? a. Break the tablet into halves or quarters. b. Dissolve the tablet in a small amount of water before giving it. c. Do not crush or break the tablet before administration. d. Crush the tablet as needed to ease administration. ANS: C Sustained-release (SR) and enteric-coated tablets or capsules are forms of medications that must not be crushed before administration so as to protect the gastrointestinal lining or the medication itself. Do not break, dissolve, or crush these tablets before administering. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 106 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 21. When administering nasal spray, which instruction by the nurse is appropriate? a. “You will need to blow your nose before I give this medication.” b. “You will need to blow your nose after I give this medication.” c. “When I give this medication, you will need to hold your breath.” d. “You need to sit up for 5 minutes after you receive the nasal spray.” ANS: A Clear the nasal passages before receiving nasal spray. Blowing one’s nose after receiving the medication will remove the medication from the nasal passages. The patient will receive the spray while inhaling through the open nostril and needs to remain in a supine position for 5 minutes afterward. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 136 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is preparing to give an aqueous intramuscular (IM) injection to an average-sized adult. Which actions are appropriate? (Select all that apply.) a. Choose a 26- or 27-gauge, - to -inch needle. b. Choose a 22- to 27-gauge, 1- to -inch needle. c. Choose the dorsogluteal site, the preferred site for IM injections for adults. d. Insert the needle at a 45-degree angle. e. Insert the needle at a 90-degree angle. f. Before injecting the medication, withdraw the plunger to check for blood return. ANS: B, E, F In general, aqueous medications can be given with a 22- to 27-gauge needle, and average needle lengths for adults range from 1 to inches. Insert the needle at a 90-degree angle. Checking for blood return is also part of the technique for IM injections to prevent inadvertent administration into the bloodstream. The ventrogluteal site is the preferred site for IM injections in adults. The dorsogluteal site is to be avoided because of proximity to nerves and blood vessels. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 116 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A patient is to receive hydromorphone (Dilaudid) 1.5 mg IV push now. The medication comes in a prefilled syringe, 2 mg/mL. Identify how many milliliters will the nurse administer for this dose. _______ ANS: 0.75 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 10: Analgesic Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A patient was diagnosed with pancreatic cancer last month, and has complained of a dull ache in the abdomen for the past 4 months. This pain has been gradually increasing, and the pain relievers taken at home are no longer effective. What type of pain is the patient experiencing? a. Acute pain b. Chronic pain c. Somatic pain d. Neuropathic pain ANS: B Chronic pain is associated with cancer and is characterized by slow onset, long duration, and dull, persistent aching. The patient’s symptoms are not characteristics of acute pain, somatic pain, or neuropathic pain. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 145 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 2. An 18-year-old basketball player fell and twisted his ankle during a game. The nurse will expect to administer which type of analgesic? a. Synthetic opioid, such as meperidine (Demerol) b. Opium alkaloid, such as morphine sulfate c. Opioid antagonist, such as naloxone HCL (Narcan) d. Nonopioid analgesic, such as indomethacin (Indocin) ANS: D Somatic pain, which originates from skeletal muscles, ligaments, and joints, usually responds to nonopioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs). The other options are not the best choices for somatic pain. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 145-146 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. A patient is recovering from abdominal surgery, which he had this morning. He is groggy but complaining of severe pain around his incision. What is the most important assessment data to consider before the nurse administers a dose of morphine sulfate to the patient? a. His pulse rate b. His respiratory rate c. The appearance of the incision d. The date of his last bowel movement ANS: B One of the most serious adverse effects of opioids is respiratory depression. The nurse must assess the patient’s respiratory rate before administering an opioid. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 153 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. A 78-year-old patient is in the recovery room after having a lengthy surgery on his hip. As he is gradually awakening, he requests pain medication. Within 10 minutes after receiving a dose of morphine sulfate, he is very lethargic and his respirations are shallow, with a rate of 7 per minute. The nurse prepares for which priority action at this time? a. Assessment of the patient’s pain level b. Immediate intubation and artificial ventilation c. Administration of naloxone (Narcan) d. Close observation of signs of opioid tolerance ANS: C Naloxone, an opioid-reversal agent, is used to reverse the effects of acute opioid overdose and is the drug of choice for reversal of opioid-induced respiratory depression. This situation is describing an opioid overdose, not opioid tolerance. Intubation and artificial ventilation are not appropriate because the patient is still breathing at 7 breaths/min. It would be inappropriate to assess the patient’s level of pain. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 153 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. A patient will be discharged with a 1-week supply of an opioid analgesic for pain management after abdominal surgery. The nurse will include which information in the teaching plan? a. How to prevent dehydration due to diarrhea b. The importance of taking the drug only when the pain becomes severe c. How to prevent constipation d. The importance of taking the drug on an empty stomach ANS: C Gastrointestinal (GI) adverse effects, such as nausea, vomiting, and constipation, are the most common adverse effects associated with opioid analgesics. Physical dependence usually occurs in patients undergoing long-term treatment. Diarrhea is not an effect of opioid analgesics. Taking the dose with food may help minimize GI upset. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 149 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A patient has been treated for lung cancer for 3 years. Over the past few months, the patient has noticed that the opioid analgesic is not helping as much as it had previously and more medication is needed for the same pain relief. The nurse is aware that this patient is experiencing which of these? a. Opioid addiction b. Opioid tolerance c. Opioid toxicity d. Opioid abstinence syndrome ANS: B Opioid tolerance is a common physiologic result of long-term opioid use. Patients with opioid tolerance require larger doses of the opioid agent to maintain the same level of analgesia. This situation does not describe toxicity (overdose), addiction, or abstinence syndrome (withdrawal). DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 147 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. A 38-year-old man has come into the urgent care center with severe hip pain after falling from a ladder at work. He says he has taken several pain pills over the past few hours but cannot remember how many he has taken. He hands the nurse an empty bottle of acetaminophen (Tylenol). The nurse is aware that the most serious toxic effect of acute acetaminophen overdose is which condition? a. Tachycardia b. Central nervous system depression c. Hepatic necrosis d. Nephropathy ANS: C Hepatic necrosis is the most serious acute toxic effect of an acute overdose of acetaminophen. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 158 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 8. A 57-year-old woman being treated for end-stage breast cancer has been using a transdermal opioid analgesic as part of the management of pain. Lately, she has been experiencing breakthrough pain. The nurse expects this type of pain to be managed by which of these interventions? a. Administering NSAIDs b. Administering an immediate-release opioid c. Changing the opioid route to the rectal route d. Making no changes to the current therapy ANS: B If a patient is taking long-acting opioid analgesics, breakthrough pain must be treated with an immediate-release dosage form that is given between scheduled doses of the long-acting opioid. The other options are not appropriate actions. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 147 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The nurse is reviewing herbal therapies. Which is a common use of the herb feverfew? a. Muscle aches b. Migraine headaches c. Leg cramps d. Incision pain after surgery ANS: B Feverfew is commonly used for migraine headaches, menstrual problems, arthritis, and fever. Possible adverse effects include muscle stiffness and muscle and joint pain. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 162 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. A patient is to receive acetylcysteine (Mucomyst) as part of the treatment for an acetaminophen (Tylenol) overdose. Which action by the nurse is appropriate when giving this medication? a. Giving the medication undiluted for full effect b. Avoiding the use of a straw when giving this medication c. Disguising the flavor with soda or flavored water d. Preparing to give this medication via a nebulizer ANS: C Acetylcysteine has the flavor of rotten eggs and so is better tolerated if it is diluted and disguised by mixing with a drink such as cola or flavored water to help increase its palatability. The use of a straw helps to minimize contact with the mucous membranes of the mouth and is recommended. The nebulizer form of this medication is used for certain types of pneumonia, not for acetaminophen overdose. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 162 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient is receiving gabapentin (Neurontin), an anticonvulsant, but has no history of seizures. The nurse expects that the patient is receiving this drug for which condition? a. Inflammation pain b. Pain associated with peripheral neuropathy c. Depression associated with chronic pain d. Prevention of seizures ANS: B Anticonvulsants are often used as adjuvants for treatment of neuropathic pain to enhance analgesic efficacy. The other indications listed are not correct. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 166 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. The nurse is assessing a patient who has been admitted to the emergency department for a possible opioid overdose. Which assessment finding is characteristic of an opioid drug overdose? a. Dilated pupils b. Restlessness c. Respiration rate of 6 breaths/min d. Heart rate of 55 beats/min ANS: C The most serious adverse effect of opioid use is CNS depression, which may lead to respiratory depression. Pinpoint pupils, not dilated pupils, are seen. Restlessness and a heart rate of 55 beats/min are not indications of an opioid overdose. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 152 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 13. The drug nalbuphine (Nubain) is an agonist-antagonist (partial agonist). The nurse understands that which is a characteristic of partial agonists? a. They have anti-inflammatory effects. b. They are given to reverse the effects of opiates. c. They have a higher potency than agonists. d. They have a lower dependency potential than agonists. ANS: D Partial agonists such as nalbuphine are similar to the opioid agonists in terms of their therapeutic indications; however, they have a lower risk of misuse and addiction. They do not have anti-inflammatory effects, nor are they given to reverse the effects of opiates. They do not have a higher potency than agonists. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 156 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 14. The nurse is assessing a patient for contraindications to drug therapy with acetaminophen (Tylenol). Which patient should not receive acetaminophen? a. A patient with a fever of 101° F (38.3° C) b. A patient who is complaining of a mild headache c. A patient with a history of liver disease d. A patient with a history of peptic ulcer disease ANS: C Liver disease is a contraindication to the use of acetaminophen. Fever and mild headache are both possible indications for the medication. Having a history of peptic ulcer disease is not a contraindication. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 157 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 15. A patient arrives at the urgent care center complaining of leg pain after a fall when rock climbing. The x-rays show no broken bones, but he has a large bruise on his thigh. The patient says he drives a truck and does not want to take anything strong because he needs to stay awake. Which statement by the nurse is most appropriate? a. “It would be best for you not to take anything if you are planning to drive your truck.” b. “We will discuss with your doctor about taking an opioid because that would work best for your pain.” c. “You can take acetaminophen, also known as Tylenol, for pain, but no more than 1000 mg per day.” d. “You can take acetaminophen, also known as Tylenol, for pain, but no more than 3000 mg per day.” ANS: D Acetaminophen is indicated for mild-to-moderate pain and does not cause drowsiness, as an opioid would. Currently, the maximum daily amount of acetaminophen is 3000 mg/day. The 1000-mg amount per day is too low. Telling the patient not to take any pain medications is incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 157 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 16. A patient is suffering from tendonitis of the knee. The nurse is reviewing the patient’s medication administration record and recognizes that which adjuvant medication is most appropriate for this type of pain? a. Antidepressant b. Anticonvulsant c. Corticosteroid d. Local anesthesia ANS: C Corticosteroids have an anti-inflammatory effect, which may help to reduce pain. The other medications do not have anti-inflammatory properties. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 166 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. Vicodin (acetaminophen/hydrocodone) is prescribed for a patient who has had surgery. The nurse informs the patient that which common adverse effects can occur with this medication? (Select all that apply.) a. Diarrhea b. Constipation c. Lightheadedness d. Nervousness e. Urinary retention f. Itching ANS: B, C, E, F Constipation (not diarrhea), lightheadedness (not nervousness), urinary retention, and itching are some of the common adverse effects that the patient may experience while taking Vicodin. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 152 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies COMPLETION 1. A patient is to receive codeine, 40 mg subcutaneously, every 6 hours as needed for pain. The solution is available in a concentration of 30 mg/mL. Identify how many milliliters of codeine will be drawn up for this dose. (record answer to one decimal place) _______ ANS: 1.3 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 11: General and Local Anesthetics Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. During a fishing trip, a patient pierced his finger with a large fishhook. He is now in the emergency department to have it removed. The nurse anticipates that which type of anesthesia will be used for this procedure? a. No anesthesia b. Topical benzocaine spray on the area c. Topical prilocaine (EMLA) cream around the site d. Infiltration of the puncture wound with lidocaine ANS: D Infiltration anesthesia is commonly used for minor surgical procedures. It involves injecting the local anesthetic solution intradermally, subcutaneously, or submucosally across the path of nerves supplying the area to be anesthetized. The local anesthetic may be administered in a circular pattern around the operative field. The other types are not appropriate for this injury. This is a painful procedure; therefore, the option of “no anesthesia” is incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 176 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. While monitoring a patient who had surgery under general anesthesia 2 hours ago, the nurse notes a sudden elevation in body temperature. This finding may be an indication of which problem? a. Tachyphylaxis b. Postoperative infection c. Malignant hypertension d. Malignant hyperthermia ANS: D A sudden elevation in body temperature during the postoperative period may indicate the occurrence of malignant hyperthermia, a life-threatening emergency. The elevated temperature does not reflect the other problems listed. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 174 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Safe and Effective Care Environment: Management of Care 3. When assessing patients in the preoperative area, the nurse knows that which patient is at a higher risk for an altered response to anesthesia? a. The 21-year-old patient who has never had surgery before b. The 35-year-old patient who stopped smoking 8 years ago c. The 40-year-old patient who is to have a kidney stone removed d. The 82-year-old patient who is to have gallbladder removal ANS: D The elderly patient is more affected by anesthesia than the young or middle-aged adult patient because of the effects of aging on the hepatic, cardiac, respiratory, and renal systems. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 173 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. A patient is undergoing abdominal surgery and has been anesthetized for 3 hours. Which nursing diagnosis would be appropriate for this patient? a. Anxiety related to the use of an anesthetic b. Risk for injury related to increased sensorium from general anesthesia c. Decreased cardiac output related to systemic effects of local anesthesia d. Impaired gas exchange related to central nervous system depression produced by general anesthesia ANS: D The nursing diagnosis of impaired gas exchange is appropriately worded for this patient. Anxiety would not be appropriate while the patient is in surgery. Sensorium would be decreased during surgery, not increased. Cardiac output is affected by general anesthesia, not local anesthesia. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 183 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. When administering a neuromuscular blocking drug, the nurse needs to remember which principle? a. It is used instead of general anesthesia during surgery. b. Only skeletal muscles are paralyzed; respiratory muscles remain functional. c. It causes sedation and pain relief while allowing for lower doses of anesthetics. d. Artificial mechanical ventilation is required because of paralyzed respiratory muscles. ANS: D Patients receiving neuromuscular blocking drugs require artificial mechanical ventilation because of the resultant paralysis of the respiratory muscles. In addition, they do not cause sedation or pain relief. They are used along with, not instead of, general anesthesia during surgery. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 178 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. A patient is being prepared for an oral endoscopy, and the nurse anesthetist reminds him that he will be awake during the procedure but probably will not remember it. What type of anesthetic technique is used in this situation? a. Local anesthesia b. Moderate sedation c. Topical anesthesia d. Spinal anesthesia ANS: B Moderate sedation effectively reduces patient anxiety, sensitivity to pain, and recall of the medical procedure, yet it preserves a patient’s ability to maintain his or her own airway and respond to verbal commands. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 175 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. During the immediate postoperative period, the Post Anesthesia Care Unit nurse is assessing a patient who had hip surgery. The patient is experiencing tachycardia, tachypnea, and muscle rigidity, and his temperature is 103° F (39.4° C). The nurse will prepare for what immediate treatment? a. Naltrexone hydrochloride (Narcan) injection, an opioid reversal drug b. Dantrolene (Dantrium) injection, a skeletal muscle relaxant c. An anticholinesterase drug, such as neostigmine d. Cardiopulmonary resuscitation (CPR) and intubation ANS: B Tachycardia, tachypnea, muscle rigidity, and raised temperature are symptoms of malignant hyperthermia, which is treated with cardiorespiratory supportive care as needed to stabilize heart and lung function as well as with immediate treatment with the skeletal muscle relaxant dantrolene. CPR is not immediately needed because the patient still has a pulse and respirations. Naltrexone and anticholinesterase drugs are not appropriate in this situation. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 174 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is preparing to administer dexmedetomidine (Precedex) to a patient. Which is an appropriate indication for dexmedetomidine? (Select all that apply.) a. Procedural sedation b. Surgeries of short duration c. Surgeries of long duration d. Postoperative anxiety e. Sedation of mechanically ventilated patients ANS: A, B, E Dexmedetomidine (Precedex) is used for procedural sedation and for surgeries of short duration, and it is also used in the intensive care setting for sedation of mechanically ventilated patients. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 174 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A patient is to receive midazolam (Versed) 2 mg IV push over 2 minutes just before an endoscopy procedure. The medication is available in a strength of 1 mg/mL. Identify how many milliliters of medication will the nurse draw up into the syringe for this dose. _______ ANS: 2 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 12: Central Nervous System Depressants and Muscle Relaxants Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A patient who has received some traumatic news is panicking and asks for some medication to help settle down. The nurse anticipates giving which drug that is most appropriate for this situation? a. Diazepam (Valium) b. Zolpidem (Ambien) c. Phenobarbital d. Cyclobenzaprine (Flexeril) ANS: A Benzodiazepines such as diazepam are used as anxiolytics, or sedatives. Zolpidem is used as a hypnotic for sleep. Phenobarbital is not used as an anxiolytic but is used for seizure control. Cyclobenzaprine is a muscle relaxant and is not used to reduce anxiety. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 191 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. A patient has been taking phenobarbital for 2 weeks as part of his therapy for epilepsy. He tells the nurse that he feels tense and that “the least little thing” bothers him now. Which is the correct explanation for this problem? a. These are adverse effects that usually subside after a few weeks. b. The drug must be stopped immediately because of possible adverse effects. c. This drug causes the rapid eye movement (REM) sleep period to increase, resulting in nightmares and restlessness. d. This drug causes deprivation of REM sleep and may cause the inability to deal with normal stress. ANS: D Barbiturates such as phenobarbital deprive people of REM sleep, which can result in agitation and the inability to deal with normal stress. A rebound phenomenon occurs when the drug is stopped (not during therapy), and the proportion of REM sleep increases, sometimes resulting in nightmares. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 194 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. A 50-year-old man who has been taking phenobarbital for 1 week is found very lethargic and unable to walk after eating out for dinner. His wife states that he has no other prescriptions and that he did not take an overdose—the correct number of pills is in the bottle. The nurse suspects that which of these may have happened? a. He took a multivitamin. b. He drank a glass of wine. c. He took a dose of aspirin. d. He developed an allergy to the drug. ANS: B Alcohol has an additive effect when combined with barbiturates and causes central nervous system (CNS) depression. Multivitamins and aspirin do not interact with barbiturates, and this situation does not illustrate an allergic reaction. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 195 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A patient has been taking temazepam (Restoril) for intermittent insomnia. She calls the nurse to say that when she takes it, she sleeps well, but the next day she feels “so tired.” Which explanation by the nurse is correct? a. “Long-term use of this drug results in a sedative effect.” b. “If you take the drug every night, this hangover effect will be reduced.” c. “These drugs affect the sleep cycle, resulting in daytime sleepiness.” d. “These drugs increase the activity of the central nervous system, making you tired the next day.” ANS: C Benzodiazepines suppress REM sleep to a degree (although not as much as barbiturates) and, thus, result in daytime sleepiness (a hangover effect). The other statements are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 191 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. A patient is recovering from a minor automobile accident that occurred 1 week ago. He is taking cyclobenzaprine (Flexeril) for muscular pain and goes to physical therapy three times a week. Which nursing diagnosis would be appropriate for him? a. Risk for injury related to decreased sensorium b. Risk for addiction related to psychologic dependency c. Decreased fluid volume related to potential adverse effects d. Disturbed sleep pattern related to the drug’s interference with REM sleep ANS: A Musculoskeletal relaxants have a depressant effect on the CNS; thus, the patient needs to be taught the importance of taking measures to minimize self-injury and falls related to decreased sensorium. “Risk for addiction” is not a NANDA nursing diagnosis. The other nursing diagnoses are not appropriate for this situation. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 198 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A patient is taking flurazepam (Dalmane) three to four nights a week for sleeplessness. She is concerned that she cannot get to sleep without taking the medication. What nonpharmacologic measures should the nurse suggest to promote sleep for this patient? a. Providing a quiet environment b. Exercising before bedtime to become tired c. Consuming heavy meals in the evening to promote sleepiness d. Drinking hot tea or coffee just before bedtime ANS: A Nonpharmacologic approaches to induce sleep include providing a quiet environment, avoiding heavy exercise before bedtime, avoiding heavy meals late in the evening, and drinking warm decaffeinated drinks, such as warm milk, before bedtime. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 201 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. A patient is brought to the emergency department for treatment of a suspected overdose. The patient was found with an empty prescription bottle of a barbiturate by his bedside. He is lethargic and barely breathing. The nurse would expect which immediate intervention? a. Starting an intravenous infusion of diluted bicarbonate solution b. Administering medications to increase blood pressure c. Implementing measures to maintain the airway and support respirations d. Administrating naloxone (Narcan) as an antagonist ANS: C There are no antagonists/antidotes for barbiturates. Treatment supports respirations and maintains the airway. The other interventions are not appropriate. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 195 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. Ramelteon (Rozerem) is prescribed for a patient with insomnia. The nurse checks the patient’s medical history, knowing that this medication is contraindicated in which disorder? a. Coronary artery disease b. Renal insufficiency c. Liver disease d. Anemia ANS: C Ramelteon is contraindicated in cases of severe liver dysfunction. The other conditions are not contraindications. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 193 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The nurse notes in the patient’s medication history that the patient is taking cyclobenzaprine (Flexeril). Based on this finding, the nurse interprets that the patient has which disorder? a. A musculoskeletal injury b. Insomnia c. Epilepsy d. Agitation ANS: A Cyclobenzaprine (Flexeril) is the muscle relaxant most commonly used to reduce spasms following musculoskeletal injuries. It is not appropriate for insomnia, epilepsy, or agitation. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 197 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. A patient has experienced insomnia for months, and the physician has prescribed a medication to help with this problem. The nurse expects which drug to be used for long-term treatment of insomnia? a. Secobarbital (Seconal), a barbiturate b. Diazepam (Valium), a benzodiazepine c. Midazolam (Versed), a benzodiazepine d. Eszopiclone (Lunesta), a nonbenzodiazepine sleep aid ANS: D Eszopiclone (Lunesta) is one of the newest prescription hypnotics to be approved for long-term use in treatment of insomnia. Barbiturates and benzodiazepines are not appropriate for long-term treatment of insomnia; midazolam is used for procedural (moderate) sedation. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 193 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient tells the nurse that he likes to drink kava herbal tea to help him relax. Which statement by the patient indicates that additional teaching about this herbal product is needed? a. “I will not drink wine with the kava tea.” b. “If I notice my skin turning yellow, I will stop taking the tea.” c. “I will not take sleeping pills if I have this tea in the evening.” d. “I will be able to drive my car after drinking this tea.” ANS: D Patients should not drive after drinking this tea because it may cause sedation. Kava tea may cause skin discoloration (with long-term use). In addition, it must not be taken with alcohol, barbiturates, and psychoactive drugs. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 192 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 1. The nurse is preparing to administer a barbiturate. Which conditions or disorders would be a contraindication to the use of these drugs? (Select all that apply.) a. Gout b. Pregnancy c. Epilepsy d. Severe chronic obstructive pulmonary disease e. Severe liver disease f. Diabetes mellitus ANS: B, D, E Contraindications to barbiturates include pregnancy, significant respiratory difficulties, and severe liver disease. The other disorders are not contraindications. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 194 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The barbiturate phenobarbital is prescribed for a patient with epilepsy. While assessing the patient’s current medications, the nurse recognizes that interactions may occur with which drugs? (Select all that apply.) a. Antihistamines b. Opioids c. Diuretics d. Anticoagulants e. Oral contraceptives f. Insulin ANS: A, B, D, E The co-administration of barbiturates and alcohol, antihistamines, benzodiazepines, opioids, and tranquilizers may result in additive CNS depression. Co-administration of anticoagulants and barbiturates can result in decreased anticoagulation response and possible clot formation. Co-administration of barbiturates and oral contraceptives can result in accelerated metabolism of the contraceptive drug and possible unintended pregnancy. There are no interactions with diuretics and insulin. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 195 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies Chapter 13: Central Nervous System Stimulants and Related Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A patient is receiving instructions regarding the use of caffeine. The nurse shares that caffeine should be used with caution if which of these conditions is present? a. A history of peptic ulcers b. Migraine headaches c. Asthma d. A history of kidney stones ANS: A Caffeine should be used with caution by patients who have histories of peptic ulcers or cardiac dysrhythmias or who have recently had myocardial infarctions. The other conditions are not contraindications to the use of caffeine. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 212 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. A patient who started taking orlistat (Xenical) 1 month ago calls the clinic to report some “embarrassing” adverse effects. She tells the nurse that she has had episodes of “not being able to control my bowel movements.” Which statement is true about this situation? a. These are expected adverse effects that will eventually diminish. b. The patient will need to stop this drug immediately if these adverse effects are occurring. c. The patient will need to increase her fat intake to prevent these adverse effects. d. The patient will need to restrict fat intake to less than 30% to help reduce these adverse effects. ANS: D Restricting dietary intake of fat to less than 30% of total calories can help reduce some of the GI adverse effects, which include oily spotting, flatulence, and fecal incontinence. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 208 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. A 6-year-old boy has been started on an extended-release form of methylphenidate hydrochloride (Ritalin) for the treatment of attention deficit hyperactivity disorder (ADHD). During a follow-up visit, his mother tells the nurse that she has been giving the medication at bedtime so that it will be “in his system” when he goes to school the next morning. What is the nurse’s appropriate evaluation of the mother’s actions? a. She is giving him the medication dosage appropriately. b. The medication should not be taken until he is at school. c. The medication should be taken with meals for optimal absorption. d. The medication should be given 4 to 6 hours before bedtime to diminish insomnia. ANS: D Central nervous system stimulants should be taken 4 to 6 hours before bedtime to decrease insomnia. Generally speaking, once-a-day dosing is used with extended-release or long-acting preparations. These formulations eliminate the need to take this medication at school. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 214 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A 22-year-old nursing student has been taking NoDoz (caffeine) tablets for the past few weeks to “make it through” the end of the semester and exam week. She is in the university clinic today because she is “exhausted.” What nursing diagnosis may be appropriate for her? a. Noncompliance b. Impaired physical mobility c. Disturbed sleep pattern d. Imbalanced nutrition: less than body requirements ANS: C The main ingredient in NoDoz, caffeine, is a central nervous system stimulant that can be used to increase mental alertness. Restlessness, anxiety, and insomnia are common adverse effects. Thus, disturbed sleep pattern is the most appropriate nursing diagnosis of those listed. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 213 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. A 10-year-old patient will be started on methylphenidate hydrochloride (Ritalin) therapy. The nurse will perform which essential baseline assessment before this drug is started? a. Eye examination b. Height and weight c. Liver function studies d. Hearing test ANS: B Assessment of baseline height and weight is important before beginning Ritalin therapy because it may cause a temporary slowing of growth in prepubertal children. The other studies are not as essential at this time. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 212 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. When evaluating a patient who is taking orlistat (Xenical), which is an intended therapeutic effect? a. Increased wakefulness b. Increased appetite c. Decreased weight d. Decreased hyperactivity ANS: C Orlistat (Xenical) is a nonstimulant drug that is used as part of a weight loss program. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 208 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. The nurse is teaching a patient how to self-administer triptan injections for migraine headaches. Which statement by the patient indicates that he needs further teaching? a. “I will take this medication regularly to prevent a migraine headache from occurring.” b. “I will take this medication when I feel a migraine headache starting.” c. “This medication does not reduce the number of migraines I will have.” d. “I will keep a journal to record the headaches I have and how the injections are working.” ANS: A Although they may be taken during aura symptoms by patients who have auras with their headaches, these drugs are not indicated for preventive migraine therapy. The medication is intended to relieve the migraine and not to prevent it or to reduce the number of attacks. The triptans do not reduce the number of migraines a person will have. Journal recordings of headaches and the patient’s responses to the medication are helpful. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 209 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is reviewing the use of central nervous system stimulants. Which of these are indications for this class of drugs? (Select all that apply.) a. Narcolepsy b. Depression c. Panic attacks d. Neonatal apnea e. Attention deficit hyperactivity disorder (ADHD) f. Appetite suppression ANS: A, D, E, F Central nervous system stimulants can be used for narcolepsy, neonatal apnea, ADHD, and appetite suppression in the treatment of obesity. They are not used for depression and panic attacks. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 204 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. A patient has a new prescription for phentermine (Ionamin) as part of the treatment for weight loss. Which information will the nurse include when teaching this patient about a stimulant such as phentermine? (Select all that apply.) a. Take this medication after meals. b. Take this medication in the morning. c. This drug is taken along with supervised exercise and suitable diet. d. Use mouth rinses, sugarless gum, or hard candies to minimize dry mouth. e. Avoid foods that contain caffeine, such as coffee, tea, and colas. ANS: B, C, D, E This drug should be taken in the morning to avoid interference with sleep, and the patient should also be on a supervised exercise and dietary regime. Caffeine-containing products should be avoided because of possible additional stimulation. Dry mouth can be minimized by the use of mouth rinses, sugarless gum, or hard candy. The other option is incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 214 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. The order reads, “Give atomoxetine (Strattera) 0.5 mg/kg/day once daily in the morning before school.” The child weighs 88 pounds. Identify how many milligrams will be administered per dose. _______ ANS: 20 mg DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 14: Antiepileptic Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is reviewing the dosage schedule for several different antiepileptic drugs (AEDs). Which antiepileptic drug allows for once-a-day dosing? a. Levetiracetam (Keppra) b. Phenobarbital c. Valproic acid (Depakote) d. Gabapentin (Neurontin) ANS: B Phenobarbital has the longest half-life of all standard AEDs, including those listed in the other options, so it allows for once-a-day dosing. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 224 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The nurse has given medication instructions to a patient receiving phenytoin (Dilantin). Which statement by the patient indicates that the patient has an adequate understanding of the instructions? a. “I will need to take extra care of my teeth and gums while on this medication.” b. “I can go out for a beer while on this medication.” c. “I can skip doses if the side effects bother me.” d. “I will be able to stop taking this drug once the seizures stop.” ANS: A Scrupulous dental care is necessary to prevent gingival hypertrophy during therapy with phenytoin. Alcohol and other central nervous system depressants may cause severe sedation. Consistent dosing is important to maintain therapeutic drug levels. Therapy with AEDs usually must continue for life and must not be stopped once seizures stop. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 225 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 3. When teaching a patient about taking a newly prescribed antiepileptic drug (AED) at home, the nurse will include which instruction? a. “Driving is allowed after 2 weeks of therapy.” b. “If seizures recur, take a double dose of the medication.” c. “Antacids can be taken with the AED to reduce gastrointestinal adverse effects.” d. “Regular, consistent dosing is important for successful treatment.” ANS: D Consistent dosing, taken regularly at the same time of day, at the recommended dose, and with meals to reduce the common gastrointestinal adverse effects, is the key to successful management of seizures when taking AEDs. Noncompliance is the factor most likely to lead to treatment failure. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 231 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Management of Care 4. A patient has a 9-year history of a seizure disorder that has been managed well with oral phenytoin (Dilantin) therapy. He is to be NPO (consume nothing by mouth) for surgery in the morning. What will the nurse do about his morning dose of phenytoin? a. Give the same dose intravenously. b. Give the morning dose with a small sip of water. c. Contact the prescriber for another dosage form of the medication. d. Notify the operating room that the medication has been withheld. ANS: C If there are any questions about the medication order or the medication prescribed, contact the prescriber immediately for clarification and for an order of the appropriate dose form of the medication. Do not change the route without the prescriber’s order. There is an increased risk of seizure activity if one or more doses of the AED are missed. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 231 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. The nurse is monitoring a patient who has been taking carbamazepine (Tegretol) for 2 months. Which effects would indicate that autoinduction has started to occur? a. The drug levels for carbamazepine are higher than expected. b. The drug levels for carbamazepine are lower than expected. c. The patient is experiencing fewer seizures. d. The patient is experiencing toxic effects from the drug. ANS: B With carbamazepine, autoinduction occurs and leads to lower than expected drug concentrations. Therefore, the dosage may have to be adjusted with time. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 226 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. The nurse is giving an intravenous dose of phenytoin (Dilantin). Which action is correct when administering this drug? a. Give the dose as a fast intravenous (IV) bolus. b. Mix the drug with normal saline, and give it as a slow IV push. c. Mix the drug with dextrose (D5W), and give it as a slow IV push. d. Mix the drug with any available solution as long as the administration rate is correct. ANS: B Intravenous phenytoin is given only with normal saline solution to prevent precipitation formation caused by incompatibilities. The IV push dose must be given slowly (not exceeding 50 mg/min in adults), and the patient must be monitored for bradycardia and decreased blood pressure. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 226 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. The U.S. Food and Drug Administration has issued a warning for users of antiepileptic drugs. Based on this report, the nurse will monitor for which potential problems with this class of drugs? a. Increased risk of suicidal thoughts and behaviors b. Signs of bone marrow depression c. Indications of drug addiction and dependency d. Increased risk of cardiovascular events, such as strokes ANS: A In December 2008, the U.S. Food and Drug Administration (FDA) required black box warnings on all antiepileptic drugs regarding the risk of suicidal thoughts and behaviors. Patients being treated with antiepileptic drugs for any indication need to be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, or any unusual changes in mood or behavior. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 222 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. A patient is experiencing status epilepticus. The nurse prepares to give which drug of choice for the treatment of this condition? a. Diazepam (Valium) b. Midazolam (Versed) c. Valproic acid (Depakote) d. Carbamazepine (Tegretol) ANS: A Diazepam (Valium) is considered by many to be the drug of choice for status epilepticus. Other drugs that are used are listed in Table 14-3 and do not include the drugs listed in the other options. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 221 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. Phenytoin (Dilantin) has a narrow therapeutic index. The nurse recognizes that this characteristic indicates which of these? a. The safe and the toxic plasma levels of the drug are very close to each other. b. The phenytoin has a low chance of being effective. c. There is no difference between safe and toxic plasma levels. d. A very small dosage can result in the desired therapeutic effect. ANS: A Having a “narrow therapeutic index” means that there is a small difference between safe and toxic drug levels. These drugs require monitoring of therapeutic plasma levels. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 222 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. A patient has been taking an AED for several years as part of his treatment for partial seizures. His wife has called because he ran out of medication this morning and wonders if he can go without it for a week until she has a chance to go to the drugstore. What is the nurse’s best response? a. “He is taking another antiepileptic drug, so he can go without the medication for a week.” b. “Stopping this medication abruptly may cause withdrawal seizures. A refill is needed right away.” c. “He can temporarily increase the dosage of his other antiseizure medications until you get the refill.” d. “He can stop all medications because he has been treated for several years now.” ANS: B Abrupt discontinuation of antiepileptic drugs can lead to withdrawal seizures. The other options are incorrect. The nurse cannot change the dose or stop the medication without a prescriber’s order. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 220 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. During a routine appointment, a patient with a history of seizures is found to have a phenytoin (Dilantin) level of 23 mcg/mL. What concern will the nurse have, if any? a. The patient is at risk for seizures because the drug level is not at a therapeutic level. b. The patient’s seizures should be under control because this is a therapeutic drug level. c. The patient’s seizures should be under control if she is also taking a second antiepileptic drug. d. The drug level is at a toxic level, and the dosage needs to be reduced. ANS: D Therapeutic drug levels for phenytoin are usually 10 to 20 mcg/mL (see Table 14-6). The other options are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 224 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 12. A patient is taking gabapentin (Neurontin), and the nurse notes that there is no history of seizures on his medical record. What is the best possible rationale for this medication order? a. The medication is used for the treatment of neuropathic pain. b. The medication is helpful for the treatment of multiple sclerosis. c. The medication is used to reduce the symptoms of Parkinson’s disease. d. The medical record is missing the correct information about the patient’s history of seizures. ANS: A Gabapentin (Neurontin) is commonly used to treat neuropathic pain. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 227 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is reviewing antiepileptic drug (AED) therapy. Which statements about AED therapy are accurate? (Select all that apply.) a. AED therapy can be stopped when seizures are stopped. b. AED therapy is usually lifelong. c. Consistent dosing is the key to controlling seizures. d. A dose may be skipped if the patient is experiencing adverse effects. e. Do not abruptly discontinue AEDs because doing so may cause rebound seizure activity. ANS: B, C, E Patients need to know that AED therapy is usually lifelong, and compliance (with consistent dosing) is important for effective seizure control. Abruptly stopping AED therapy may cause withdrawal (or rebound) seizure activity. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 232 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A 9-year-old child will be receiving carbamazepine (Tegretol) suspension, 200 mL daily. The medication is available in a strength of 100 mg/5 mL. Identify how many milliliters will the nurse give to the patient for each dose. _______ ANS: 10 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 15: Antiparkinson Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A patient has been taking selegiline (Eldepryl), 20 mg/day for 1 month. Today, during his office visit, he tells the nurse that he forgot and had a beer with dinner last evening, and “felt awful.” What did the patient most likely experience? a. Hypotension b. Hypertension c. Urinary discomfort d. Gastrointestinal upset ANS: B At doses that exceed 10 mg/day, selegiline becomes a nonselective monoamine oxidase inhibitor (MAOI), contributing to the development of the cheese effect, so-called because it interacts with tyramine-containing foods (cheese, red wine, beer, and yogurt) and can cause severe hypertension. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 238 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 2. A patient has been given a prescription for levodopa-carbidopa (Sinemet) for her newly diagnosed Parkinson’s disease. She asks the nurse, “Why are there two drugs in this pill?” The nurse’s best response reflects which fact? a. Carbidopa allows for larger doses of levodopa to be given. b. Carbidopa prevents the breakdown of levodopa in the periphery. c. There are concerns about drug-food interactions with levodopa therapy that do not exist with the combination therapy. d. Carbidopa is the biologic precursor of dopamine and can penetrate into the central nervous system. ANS: B When given in combination with levodopa, carbidopa inhibits the breakdown of levodopa in the periphery and thus allows smaller doses of levodopa to be used. Lesser amounts of levodopa result in fewer unwanted adverse effects. Levodopa, not carbidopa, is the biologic precursor of dopamine and can penetrate into the CNS. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 243 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. When a patient is taking an anticholinergic such as benztropine (Cogentin) as part of the treatment for Parkinson’s disease, the nurse should include which information in the teaching plan? a. Minimize the amount of fluid taken while on this drug. b. Discontinue the medication if adverse effects occur. c. Take the medication on an empty stomach to enhance absorption. d. Use artificial saliva, sugarless gum, or hard candy to counteract dry mouth. ANS: D Dry mouth can be managed with artificial saliva through drops or gum, frequent mouth care, forced fluids, and sucking on sugar-free hard candy. Anticholinergics should be taken with or after meals to minimize GI upset and must not be discontinued suddenly. The patient must drink at least 3000 mL/day unless contraindicated. Drinking water is important, even if the patient is not thirsty or in need of hydration, to prevent and manage the adverse effect of constipation. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 246 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A patient has been treated with antiparkinson medications for 3 months. What therapeutic responses should the nurse look for when assessing this patient? a. Decreased appetite b. Gradual development of cogwheel rigidity c. Newly developed dyskinesias d. Improved ability to perform activities of daily living ANS: D Therapeutic responses to antiparkinson agents include an improved sense of well-being, improved mental status, increased appetite, increased ability to perform activities of daily living and to concentrate and think clearly, and less intense parkinsonian manifestations. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 247 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. Carbidopa-levodopa (Sinemet) is prescribed for a patient with Parkinson’s disease. The nurse informs the patient that which common adverse effects can occur with this medication? a. Drowsiness, headache, weight loss b. Dizziness, insomnia, nausea c. Peripheral edema, fatigue, syncope d. Heart palpitations, hypotension, urinary retention ANS: D Common adverse reactions associated with carbidopa-levodopa include palpitations, hypotension, urinary retention, dyskinesia, and depression. The other effects may occur with other antiparkinson drugs. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 239 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. The nurse is assessing the medication history of a patient with a new diagnosis of Parkinson’s disease. Which condition is a contraindication for the patient, who will be taking tolcapone (Tasmar)? a. Glaucoma b. Seizure disorder c. Liver failure d. Benign prostatic hyperplasia ANS: C Tolcapone is contraindicated in patients who have shown a hypersensitivity reaction to it, and it should be used with caution in patients with pre-existing liver disease. The other conditions listed are not contraindications. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 241 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse is developing a care plan for a patient who is taking an anticholinergic drug. Which nursing diagnosis would be appropriate for this patient? a. Diarrhea b. Urinary retention c. Risk for infection d. Disturbed sleep pattern ANS: B Patients receiving anticholinergic drugs are at risk for urinary retention and constipation, not diarrhea. The other nursing diagnoses are not applicable to anticholinergic drugs. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 245 TOP: NURSING PROCESS: Nursing Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. A patient has a new order for a catechol ortho-methyltransferase (COMT) inhibitor as part of treatment for Parkinson’s disease. The nurse recognizes that which of these is an advantage of this drug class? a. It has a shorter duration of action. b. It causes less gastrointestinal distress. c. It has a slower onset than traditional Parkinson’s disease drugs. d. It is associated with fewer wearing-off effects. ANS: D COMT inhibitors are associated with fewer wearing-off effects and have prolonged therapeutic benefits. They have a quicker onset, and they prolong the duration of action of levodopa. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: pp. 240-241 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. A patient taking entacapone (Comtan) for the first time calls the clinic to report a dark discoloration of his urine. After listening to the patient, the nurse realizes that what is happening in this situation? a. This is a harmless effect of the drug. b. The patient has taken this drug along with red wine or cheese. c. The patient is having an allergic reaction to the drug. d. The ordered dose is too high for this patient. ANS: A COMT inhibitors, including entacapone, may darken a patient’s urine and sweat. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 239 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. While a patient is receiving drug therapy for Parkinson’s disease, the nurse monitors for dyskinesia, which is manifested by which finding? a. Rigid, tense muscles b. Difficulty in performing voluntary movements c. Limp extremities with weak muscle tone d. Confusion and altered mental status ANS: B Dyskinesia is the difficulty in performing voluntary movements that is experienced by some patients with Parkinson’s disease. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 237 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. When treating patients with medications for Parkinson’s disease, the nurse knows that the wearing-off phenomenon occurs for which reason? a. There are rapid swings in the patient’s response to levodopa. b. The patient cannot tolerate the medications at times. c. The medications begin to lose effectiveness against Parkinson’s disease. d. The patient’s liver is no longer able to metabolize the drug. ANS: C The wearing-off phenomenon occurs when antiparkinson medications begin to lose their effectiveness, despite maximal dosing, as the disease progresses. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 237 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. When assessing the medication history of a patient with a new diagnosis of Parkinson’s disease, which conditions are contraindications for the patient who will be taking carbidopa-levodopa? (Select all that apply.) a. Angle-closure glaucoma b. History of malignant melanoma c. Hypertension d. Benign prostatic hyperplasia e. Concurrent use of monoamine oxidase inhibitors (MAOIs) ANS: A, B, E Angle-closure glaucoma, a history of melanoma or other undiagnosed skin conditions, and concurrent use of MAOIs are contraindications to the use of carbidopa-levodopa. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 242-243 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 1. The prescriber writes this order, “Give amantadine (Symmetrel) 100 mg per PEG tube twice a day.” The medication is available in a liquid form with a concentration 50 mg/5 mL. Identify how many milliliters will the nurse give with each dose. _______ ANS: 10 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 16: Psychotherapeutic Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse reads in the patient’s medication history that the patient is taking buspirone (BuSpar). The nurse interprets that the patient may have which disorder? a. Anxiety disorder b. Depression c. Schizophrenia d. Bipolar disorder ANS: A Buspirone is indicated for the treatment of anxiety disorders, not depression, schizophrenia, or bipolar disorder. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 253 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. Before beginning a patient’s therapy with selective serotonin reuptake inhibitor (SSRI) antidepressants, the nurse will assess for concurrent use of which medications or medication class? a. Aspirin b. Anticoagulants c. Diuretics d. Nonsteroidal anti-inflammatory drugs ANS: B Use of selective serotonin reuptake inhibitor (SSRI) antidepressants with warfarin results in an increased anticoagulant effect. SSRI antidepressants do not interact with the other drugs or drug classes listed. See Table 16-6 for important drug interactions with SSRIs. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 258 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 3. When a patient is receiving a second-generation antipsychotic drug, such as risperidone (Risperdal), the nurse will monitor for which therapeutic effect? a. Fewer panic attacks b. Decreased paranoia and delusions c. Decreased feeling of hopelessness d. Improved tardive dyskinesia ANS: B The therapeutic effects of the antipsychotic drugs include improvement in mood and affect, and alleviation or decrease in psychotic symptoms (decrease in hallucinations, paranoia, delusions, garbled speech). Tardive dyskinesia is a potential adverse effect of these drugs. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 272 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A patient has been taking haloperidol (Haldol) for 3 months for a psychotic disorder, and the nurse is concerned about the development of extrapyramidal symptoms. The nurse will monitor the patient closely for which effects? a. Increased paranoia b. Drowsiness and dizziness c. Tremors and muscle twitching d. Dry mouth and constipation ANS: C Extrapyramidal symptoms are manifested by tremors and muscle twitching, and the incidence of such symptoms is high during haloperidol therapy. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 264 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. A patient has been taking the monoamine oxidase inhibitor (MAOI) phenelzine (Nardil) for 6 months. The patient wants to go to a party and asks the nurse, “Will just one beer be a problem?” Which advice from the nurse is correct? a. “You can drink beer as long as you have a designated driver.” b. “Now that you’ve had the last dose of that medication, there will be no further dietary restrictions.” c. “If you begin to experience a throbbing headache, rapid pulse, or nausea, you’ll need to stop drinking.” d. “You need to avoid all foods that contain tyramine, including beer, while taking this medication.” ANS: D Foods containing tyramine, such as beer and aged cheeses, should be avoided while a patient is taking an MAOI. Drinking beer while taking an MAOI may precipitate a dangerous hypertensive crisis. The other options are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 258 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Safe and Effective Care Environment: Safety and Infection Control 6. A 22-year-old patient has been taking lithium for 1 year, and the most recent lithium level is 0.9 mEq/L. Which statement about the laboratory result is correct? a. The lithium level is therapeutic. b. The lithium level is too low. c. The lithium level is too high. d. Lithium is not usually monitored with blood levels. ANS: A Desirable long-term maintenance lithium levels range between 0.6 and 1.2 mEq/L. The other responses are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 269 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. A patient with the diagnosis of schizophrenia is hospitalized and is taking a phenothiazine drug. Which statement by this patient indicates that he is experiencing a common adverse effect of phenothiazines? a. “I can’t sleep at night.” b. “I feel hungry all the time.” c. “Look at how red my hands are.” d. “My mouth has been so dry lately.” ANS: D Phenothiazines produce anticholinergic-like adverse effects of dry mouth, urinary hesitancy, and constipation. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 270 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. A patient has been taking the selective serotonin reuptake inhibitor (SSRI) sertraline (Zoloft) for about 6 months. At a recent visit, she tells the nurse that she has been interested in herbal therapies and wants to start taking St. John’s wort. Which response by the nurse is appropriate? a. “That should be no problem.” b. “Good idea! Hopefully you’ll be able to stop taking the Zoloft.” c. “Be sure to stop taking the herb if you notice a change in side effects.” d. “Taking St. John’s wort with Zoloft may cause severe interactions and is not recommended.” ANS: D The herbal product St. John’s wort must not be used with SSRIs. Potential interactions include confusion, agitation, muscle spasms, twitching, and tremors. The other responses by the nurse are inappropriate. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 260 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. While monitoring a depressed patient who has just started SSRI antidepressant therapy, the nurse will observe for which problem during the early time frame of this therapy? a. Hypertensive crisis b. Self-injury or suicidal tendencies c. Extrapyramidal symptoms d. Loss of appetite ANS: B In 2005, the U.S. Food and Drug Administration (FDA) issued special black-box warnings regarding the use of all classes of antidepressants in both adult and pediatric patient populations. Data from the FDA indicated a higher risk for suicide in patients receiving these medications. As a result, current recommendations for all patients receiving antidepressants include regular monitoring for signs of worsening depressive symptoms, especially when the medication is started or the dosage is changed. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 256 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 10. A patient has been admitted to the emergency department with a suspected overdose of a tricyclic antidepressant. The nurse will prepare for what immediate concern? a. Hypertension b. Renal failure c. Cardiac dysrhythmias d. Gastrointestinal bleeding ANS: C Tricyclic antidepressant overdoses are notoriously lethal. The primary organ systems affected are the central nervous system and the cardiovascular system, and death usually results from either seizures or dysrhythmias. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 256 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. The wife of a patient who has been diagnosed with depression calls the office and says, “It’s been an entire week since he started that new medicine for his depression, and there’s no change! What’s wrong with him?” What is the nurse’s best response? a. “The medication may not be effective for him. He may need to try another type.” b. “It may take up to 6 weeks to notice any therapeutic effects. Let’s wait a little longer to see how he does.” c. “It sounds like the dose is not high enough. I’ll check about increasing the dosage.” d. “Some patients never recover from depression. He may not respond to this therapy.” ANS: B Patients and family members need to be told that antidepressant drugs commonly require several weeks before full therapeutic effects are noted. The other answers are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 257 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. Chlorpromazine (Thorazine) is prescribed for a patient, and the nurse provides instructions to the patient about the medication. The nurse includes which information? a. The patient needs to avoid caffeine while on this drug. b. The patient needs to wear sunscreen while outside because of photosensitivity. c. Long-term therapy may result in nervousness and excitability. d. The medication may be taken with an antacid to reduce gastrointestinal upset. ANS: B Sun exposure and tanning booths need to be avoided with conventional antipsychotics because of the adverse effect of photosensitivity. Instruct the patient to apply sunscreen liberally and to wear sun-protective clothing and hats. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 264 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 13. The nurse is reviewing the food choices of a patient who is taking a monoamine oxidase inhibitor ( MAOI). Which food choice would indicate the need for additional teaching? a. Orange juice b. Fried eggs over-easy c. Salami and Swiss cheese sandwich d. Biscuits and honey ANS: C Aged cheeses, such a Swiss or cheddar cheese, and Salami contain tyramine. Patients who are taking MAOIs need to avoid tyramine-containing foods because of a severe hypertensive reaction that may occur. Orange juice, eggs, biscuits, and honey do not contain tyramine. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 260 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. A patient wants to take a ginseng dietary supplement. The nurse instructs the patient to look for which potential adverse effect? a. Drowsiness b. Palpitations and anxiety c. Dry mouth d. Constipation ANS: B Elevated blood pressure, chest pain or palpitations, anxiety, insomnia, headache, nausea, vomiting, and diarrhea are potential adverse effects of ginseng. Drowsiness, difficulty with urination, and constipation are not potential adverse effects of ginseng. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 269 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. The nurse is reviewing medications used for depression. Which of these statements is a reason that selective serotonin reuptake inhibitors (SSRIs) are more widely prescribed today than tricyclic antidepressants? a. SSRIs have fewer sexual side effects. b. Unlike tricyclic antidepressants, SSRIs do not have drug-food interactions. c. Tricyclic antidepressants cause serious cardiac dysrhythmias if an overdose occurs. d. SSRIs cause a therapeutic response faster than tricyclic antidepressants. ANS: C Death from overdose of tricyclic antidepressants usually results from either seizures or dysrhythmias. SSRIs are associated with significantly fewer and less severe systemic adverse effects, especially anticholinergic and cardiovascular adverse effects. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 257 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. A patient who has been taking a selective serotonin reuptake inhibitor (SSRI) is complaining of “feeling so badly” when he started taking an over-the-counter St. John’s wort herbal product at home. The nurse suspects that he is experiencing serotonin syndrome. Which of these are symptoms of serotonin syndrome? (Select all that apply.) a. Agitation b. Drowsiness c. Tremors d. Bradycardia e. Sweating f. Constipation ANS: A, C, E Common symptoms of serotonin syndrome include delirium, agitation, tachycardia, sweating, hyperreflexia, shivering, coarse tremors, and others. See Box 16-1 for a full list of symptoms. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 260 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. Which statements are true regarding the selective serotonin reuptake inhibitors (SSRIs)? (Select all that apply.) a. Avoid foods and beverages that contain tyramine. b. Monitor the patient for extrapyramidal symptoms. c. Therapeutic effects may not be seen for about 4 to 6 weeks after the medication is started. d. If the patient has been on an MAOI, a 2- to 5-week or longer time span is required before beginning an SSRI medication. e. These drugs have anticholinergic effects, including constipation, urinary retention, dry mouth, and blurred vision. f. Cogentin is often also prescribed to reduce the adverse effects that may occur. ANS: C, D During SSRI medication, therapeutic effects may not be seen for 4 to 6 weeks. To prevent the potentially fatal pharmacodynamic interactions that can occur between the SSRIs and the MAOIs, a 2- to 5-week washout period is recommended between uses of these two classes of medications. The other options apply to other classes of psychotherapeutic drugs, not SSRIs. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 261 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. An agitated patient is to receive an intravenous dose of diazepam (Valium). The order reads, “Give diazepam, 2 mg, IV push, now. Repeat in 15 minutes if needed.” Identify how many milliliters will the nurse administer for this dose. The medication vial contains 5 mg/mL. _______ ANS: 0.4 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 17: Substance Abuse Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. A 38-year-old male patient stopped smoking 6 months ago. He tells the nurse that he still feels strong cigarette cravings and wonders if he is ever going to feel “normal” again. Which statement by the nurse is correct? a. “It’s possible that these cravings will never stop.” b. “These cravings may persist for several months.” c. “The cravings tell us that you are still using nicotine.” d. “The cravings show that you are about to experience nicotine withdrawal.” ANS: B Cigarette cravings may persist for months after nicotine withdrawal. The other statements are false. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 285 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. A patient in a rehabilitation center is beginning to experience opioid withdrawal symptoms. The nurse expects to administer which drug as part of the treatment? a. Diazepam (Valium) b. Methadone c. Disulfiram (Antabuse) d. Bupropion (Zyban) ANS: B Opioid withdrawal can be managed with either methadone or clonidine (Catapres). Diazepam and disulfiram are used for treatment of alcoholism, and bupropion is used to assist with smoking cessation. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 279 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. A patient has been taking naltrexone (ReVia) as part of the treatment for addiction to heroin. The nurse expects that the naltrexone will have which therapeutic effect for this patient? a. Naltrexone prevents the cravings for opioid drugs. b. Naltrexone works as a safer substitute for the heroin until the patient completes withdrawal. c. The patient will experience flushing, sweating, and severe nausea if he takes heroin while on naltrexone. d. If opioid drugs are used while taking naltrexone, euphoria is not produced; thus, the opioid’s desired effects are lost. ANS: D Naltrexone works to eliminate the euphoria that occurs with opioid drug use; therefore, the reinforcing effect of the drug is lost. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 279 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. The nurse is presenting a substance-abuse lecture for teenage girls and is asked about “roofies.” The nurse recognizes that this is the slang term for which substance? a. Cocaine b. Flunitrazepam c. Secobarbital d. Methamphetamine ANS: B Flunitrazepam is a benzodiazepine that has recently gained popularity as a recreational drug and is commonly called roofies (the “date-rape” drug). The other drugs are not known as roofies. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 281 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. A 29-year-old male patient is admitted to the intensive care unit with the following symptoms: restlessness, hyperactive reflexes, talkativeness, confusion and periods of panic and euphoria, tachycardia, and fever. The nurse suspects that he may be experiencing the effects of taking which substance? a. Opioids b. Alcohol c. Stimulants d. Depressants ANS: C The adverse effects listed may occur with use of stimulants and are commonly an extension of their therapeutic effects. Opioids, alcohol, and depressants do not have these effects. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 280 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. When admitting a patient with a suspected diagnosis of chronic alcohol use, the nurse will keep in mind that chronic use of alcohol might result in which condition? a. Renal failure b. Cerebrovascular accident c. Korsakoff’s psychosis d. Alzheimer’s disease ANS: C A variety of serious neurologic and mental disorders, such as Korsakoff’s psychosis and Wernicke’s encephalopathy, as well as cirrhosis of the liver, may occur with chronic use of alcohol. Renal failure, cerebrovascular accident, and Alzheimer’s disease are not associated directly with chronic use of alcohol. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 283 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. A patient is being treated for ethanol alcohol abuse in a rehabilitation center. The nurse will include which information when teaching him about disulfiram (Antabuse) therapy? a. He should not smoke cigarettes while on this drug. b. He needs to know about the common over-the-counter substances that contain alcohol. c. This drug will cause the same effects as the alcohol did, without the euphoric effects. d. Mouthwashes and cough medicines that contain alcohol are safe because they are used in small amounts. ANS: B The use of disulfiram (Antabuse) with alcohol-containing over-the-counter products will elicit severe adverse reactions. As little as 7 mL of alcohol may cause symptoms in a sensitive person. Cigarette smoking does not cause problems when taking disulfiram. Disulfiram does not have the same effects as alcohol. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 284 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. The nurse is conducting a smoking-cessation program. Which statement regarding drugs used in cigarette-smoking–cessation programs is true? a. Rapid chewing of the nicotine gum releases an immediate dose of nicotine. b. Quick relief from withdrawal symptoms is most easily achieved by using a transdermal patch. c. Compliance with treatment is higher with use of the gum rather than the transdermal patch. d. The nicotine gum can be used only up to six times per day. ANS: A Quick or acute relief from withdrawal symptoms is most easily achieved with the use of the gum because rapid chewing of the gum produces an immediate dose of nicotine. However, treatment compliance is higher with the use of the transdermal patch system. Nicotine gum can be used whenever the patient has a strong urge to smoke. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 285 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. A nurse is providing teaching for a patient who will be taking varenicline (Chantix) as part of a smoking-cessation program. Which teaching points are appropriate for a patient taking this medication? (Select all that apply.) a. This drug is available as a chewing gum that can be taken to reduce cravings. b. Use caution when driving because drowsiness may be a problem. c. There have been very few adverse effects reported for this drug. d. Notify the prescriber immediately if feelings of sadness or thoughts of suicide occur. e. Avoid caffeine while on this drug. ANS: B, D Patients taking varenicline have reported drowsiness, which has prompted the U.S. Food and Drug Administration (FDA) to recommend caution when driving and engaging in other potentially hazardous activities until the patient can determine how the drug affects his or her mental status. In addition, the FDA has warned about psychiatric symptoms including agitation, depression, and suicidality. Varenicline is an oral tablet, and common adverse effects include nausea, vomiting, headache, and insomnia. There are no cautions about taking caffeine while on this drug. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 285 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 2. A patient has been taking disulfiram (Antabuse) as part of his rehabilitation therapy. However, this evening, he attended a party and drank half a beer. As a result, he became ill and his friends took him to the emergency department. The nurse will look for which adverse effects associated with acetaldehyde syndrome? (Select all that apply.) a. Euphoria b. Severe vomiting c. Diarrhea d. Pulsating headache e. Difficulty breathing f. Sweating ANS: B, D, E, F Acetaldehyde syndrome results when alcohol is taken while on disulfiram (Antabuse) therapy. Adverse effects include CNS effects (pulsating headache, sweating, marked uneasiness, weakness, vertigo, others); GI effects (nausea, copious vomiting, thirst); and difficulty breathing. Cardiovascular effects also occur; see Table 17-2. Euphoria and diarrhea are not adverse effects associated with acetaldehyde syndrome. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 284 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is monitoring a patient who is experiencing severe ethanol withdrawal. Which are signs and symptoms of severe ethanol withdrawal? (Select all that apply.) a. Agitation b. Drowsiness c. Tremors d. Systolic blood pressure higher than 200 mm Hg e. Temperature over 100° F (37.7° C) f. Pulse rate 110 beats/min ANS: A, C, D Signs and symptoms of severe ethanol withdrawal (delirium tremens) include systolic blood pressure higher than 200 mm Hg, diastolic blood pressure higher than 140 mm Hg, pulse rate higher than 140 beats/min, temperature above 101° F (38.3° C), tremors, insomnia, and agitation. See Box 17-6 for all signs and symptoms of ethanol withdrawal. Chapter 18: Adrenergic Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is aware that adrenergic drugs produce effects similar to which of these nervous systems? a. Central nervous system b. Somatic nervous system c. Sympathetic nervous system d. Parasympathetic nervous system ANS: C Adrenergic drugs mimic the effects of the sympathetic nervous system. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 297 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. When an adrenergic drug stimulates beta1-adrenergic receptors, the result is an increased force of contraction, which is known as what type of effect? a. Positive inotropic b. Anti-adrenergic c. Negative dromotropic d. Positive chronotropic ANS: A An increased force of contraction is known as a positive inotropic effect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 299 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. When a patient is taking an adrenergic drug, the nurse expects to observe which effect? a. Increased heart rate b. Bronchial constriction c. Constricted pupils d. Increased intestinal peristalsis ANS: A Increased heart rate is one of the effects of adrenergic drugs. Sympathetic nervous system stimulation also results in bronchodilation, dilated pupils, and decreased gastrointestinal mobility, depending upon which receptors are stimulated. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 297 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. An adrenergic agonist is ordered for a patient in shock. The nurse will note that this drug has had its primary intended effect if which expected outcome occurs? a. Volume restoration b. Increased cardiac output c. Decreased urine output d. Reduced anxiety ANS: B For a patient in shock, a primary benefit of an adrenergic agonist drug is to increase cardiac output. A drug in this category should not be used in place of volume restoration, nor does it provide volume restoration (IV fluids do this). Adrenergic agonists may enhance urine output if cardiac output and perfusion to the kidneys increase. These drugs do not reduce anxiety. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 302 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. The nurse is administering a stat dose of epinephrine. Epinephrine is appropriate for which situation? a. Severe hypertension b. Angina c. Cardiac arrest d. Tachycardia ANS: C Treatment of cardiac arrest is an indication for the use of epinephrine. The other options are not indications for epinephrine. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 302 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 6. A patient is on a low-dose dobutamine drip for heart failure. She had been feeling better but now has a sense of tightness in her chest, palpitations, and a bit of anxiety. Her heart rate is up to 110 per minute, and her blood pressure is 150/98 mm Hg (increased from previous readings of 86 per minute and 120/80 mm Hg). What is the nurse’s immediate concern for this patient? a. She is experiencing normal adverse effects of dobutamine therapy. b. She may be experiencing an allergic reaction to the dobutamine. c. The medication may be causing a worsening of a pre-existing cardiac disorder. d. The dosage of the dobutamine needs to be increased to control the symptoms better. ANS: C Because dobutamine is a vasoactive adrenergic, it works by increasing the cardiac output in heart failure patients by increasing myocardial contractility and stroke volume. However, adrenergic drugs may worsen a pre-existing cardiac disorder, such as causing a myocardial infarction in a patient with coronary artery disease. The other options are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 300 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. A 14-year-old patient has been treated for asthma for almost 4 months. Two weeks ago, she was given salmeterol as part of her medication regimen. However, her mother has called the clinic to report that it does not seem to work when her daughter is having an asthma attack. Which response by the nurse is appropriate? a. “It takes time for a therapeutic response to develop.” b. “She is too young for this particular medication; it will be changed.” c. “She needs to take up to two puffs every 4 hours to ensure adequate blood levels.” d. “This medication is indicated for prevention of bronchospasms, not for relief of acute symptoms.” ANS: D Salmeterol is indicated for the prevention of bronchospasms, not treatment of acute symptoms. The dosage is usually two puffs twice daily, 12 hours apart, for maintenance effects in patients older than 12 years of age. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 306 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. A hospitalized patient is experiencing a severe anaphylactic reaction to a dose of intravenous penicillin. Which drug will the nurse expect to use to treat this condition? a. Ephedra b. Epinephrine c. Phenylephrine d. Pseudoephedrine ANS: B Epinephrine is the drug of choice for the treatment of anaphylaxis. The other drugs listed are incorrect choices. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 301 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The nurse recognizes that adrenergic drugs cause relaxation of the bronchi and bronchodilation by stimulating which type of receptors? a. Dopaminergic b. Beta1 adrenergic c. Beta2 adrenergic d. Alpha1 adrenergic ANS: C Stimulation of beta2-adrenergic receptors results in bronchodilation. The other choices are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 303 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. The nurse is preparing to administer dopamine. Which is the correct technique for administering dopamine? a. Orally b. Intravenous (IV) push injection c. Intermittent IV infusions (IV piggyback) d. Continuous IV infusion with an infusion pump ANS: D Dopamine is available only as an IV injectable drug and is given by continuous infusion, using an infusion pump. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: pp. 301-302 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is presenting information to a class of students about adrenergic drugs. Which are the effects of drugs that stimulate the sympathetic nervous system? (Select all that apply.) a. Dilation of bronchioles b. Constriction of bronchioles c. Decreased heart rate d. Increased heart rate e. Dilated pupils f. Constricted pupils g. Glycogenolysis ANS: A, D, E, G Stimulation of the sympathetic nervous system causes bronchodilation, increased heart rate, pupil dilation, and glycogenolysis as well as many other effects (see Table 18-1). The other responses are effects that occur as a result of the stimulation of the parasympathetic nervous system. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 297 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. The nurse is to administer epinephrine 0.3 mg subcutaneously. The ampule contains 1 mL of medication and is labeled “Epinephrine 1:1000.” Identify how many milliliters of epinephrine will the nurse give. _______ ANS: 0.3 mL Note that 1:1000 indicates 1 gram per 1000 mL or 1000 mg per 1000 mL, which is a concentration of 1 mg/mL. DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 19: Adrenergic-Blocking Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. During therapy with a beta blocker, the patient notices that she has swollen feet, has gained 3 pounds within 2 days, feels short of breath even when walking around the house, and has been dizzy. The nurse suspects that which of these is occurring? a. The patient is experiencing an allergic reaction. b. The patient may be developing heart failure. c. More time is needed for the patient to see a therapeutic response to the drug. d. The patient is experiencing expected adverse effects of the drug. ANS: B Even though some beta blockers may be used for the treatment of some types of heart failure, the patient needs to be assessed often for the development of heart failure, a potential adverse effect of the drugs. These symptoms do not indicate expected adverse effects, an allergic reaction, or a therapeutic response. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 318 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. A patient is going home with a new prescription for the beta-blocker atenolol (Tenormin). The nurse will include which content when teaching the patient about this drug? a. Never stop taking this medication abruptly. b. The medication will be stopped once symptoms subside. c. If adverse effects occur, stop taking the drug for 24 hours, and then resume. d. Be watchful for first-dose hypotension. ANS: A Patients need to be weaned off these medications slowly because rebound hypertension and chest pain are possible with abrupt withdrawal. The drugs should never be stopped abruptly nor doses skipped. First-dose hypotension occurs with alpha blockers. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 318 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 3. During initial rounds, the nurse notes that a dobutamine infusion has extravasated into the forearm of a patient. After stopping the infusion, the nurse follows standing orders and immediately injects phentolamine (Regitine) subcutaneously in a circular fashion around the extravasation site. What is the mechanism of action of the phentolamine in this situation? a. It neutralizes the extravasated dobutamine immediately. b. It causes arterial vasoconstriction and reduced pain and swelling at the site. c. It increases peripheral vascular resistance and reduces arterial pressure at the site. d. It increases blood flow to the ischemic site by vasodilation to prevent tissue damage. ANS: D Phentolamine is an alpha blocker that reduces peripheral vascular resistance when given systemically, but local subcutaneous injection around the site of extravasated vasoconstrictive drugs, such as dobutamine, causes an alpha-adrenergic receptor blockade and vasodilation. This allows for increased blood flow to the ischemic tissue and may prevent permanent tissue damage. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 312 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A 58-year-old man has had a myocardial infarction (MI), has begun rehabilitation, and is ready for discharge. He is given a prescription for metoprolol (Lopressor) and becomes upset after reading the patient education pamphlet. “I don’t have high blood pressure—why did my doctor give me this medicine?” Which explanation by the nurse is correct? a. “This medication will prevent blood clots that may lead to another heart attack.” b. “Beta blockers will improve blood flow to the kidneys.” c. “This drug is prescribed to prevent the high blood pressure that often occurs after a heart attack.” d. “Studies have shown that this medication has greatly increased survival rates in patients who have had a heart attack.” ANS: D Beta blockers are frequently given to patients after they have suffered an MI because of their cardioprotective properties. The other responses are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 313 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Psychosocial Integrity 5. The teaching for a patient who is taking tamsulosin (Flomax) to reduce urinary obstruction due to benign prostatic hyperplasia will include which of these? a. Fluids need to be restricted while on this medication. b. Take the medication with breakfast to promote the maximum effects of the drug. c. Get up slowly from a sitting or lying position. d. Blood pressure must be monitored because the medication may cause hypertension. ANS: C This medication is used to relieve impaired urinary flow in men with benign prostatic hyperplasia, but it also can cause orthostatic hypotension when changing positions from sitting or lying positions. Because of these effects, the blood pressure may become dramatically lowered, and lightheadedness may occur, increasing the risk of falling. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 317 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is screening a patient who will be taking a nonspecific/nonselective beta blocker. Which condition, if present, may cause serious problems if the patient takes this medication? a. Angina b. Hypertension c. Glaucoma d. Asthma ANS: D Nonspecific/nonselective beta-blocking drugs may precipitate bradycardia, hypotension, heart block, heart failure, bronchoconstriction, and/or increased airway resistance. Therefore, any pre-existing respiratory conditions such as asthma might be worsened by the concurrent use of any of these medications. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 317 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. A patient is experiencing diastolic heart failure. The nurse expects which beta blocker to be ordered for this patient? a. Atenolol (Tenormin) b. Carvedilol (Coreg) c. Acebutolol (Sectral) d. Esmolol (Brevibloc) ANS: B Not all beta blockers are used for the treatment of heart failure. Carvedilol and metoprolol are currently used in the treatment of heart failure. The other options are not indicated for the treatment of heart failure. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 315 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. During a teaching session about self-monitoring while taking a beta blocker at home, the nurse has taught the patient to take his apical pulse daily for 1 minute. If the pulse rate decreases to less than 60 beats/min, the nurse will instruct the patient to: a. notify his prescriber. b. reduce the dose of his beta blocker by half. c. continue the medication because this is an expected effect. d. skip the medication dose that day, and check his pulse again the next day. ANS: A Cardiac depression can occur with beta blockers; instruct the patient to contact his prescriber if his pulse rate decreases to less than 60 per minute. The medication dose may need to be changed, but it is not appropriate for the nurse to change the dosage. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 317 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. A 49-year-old patient is in the clinic for a follow-up visit 6 months after starting a beta blocker for treatment of hypertension. During this visit, his blood pressure is 169/98 mm Hg, and he eventually confesses that he stopped taking this medicine 2 months ago because of an “embarrassing problem.” What problem did the patient most likely experience with this medication that caused him to stop taking it? a. Urge incontinence b. Dizziness when standing up c. Excessive flatus d. Impotence ANS: D Impotence is a potential adverse effect of beta blockers and may cause patients to stop taking the medication. The other options are not adverse effects of beta blockers. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 314 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. A patient has a new prescription for tamsulosin (Flomax) as treatment for benign prostatic hyperplasia. The nurse is checking his current medication list and will contact the prescriber regarding a potential interaction if the patient is also taking which drug? a. Levothyroxine (Synthroid) for hypothyroidism b. Sildenafil (Viagra), an erectile dysfunction medication c. Omeprazole (Prilosec), a proton pump inhibitor d. Low-dose aspirin for stroke prevention ANS: B Drugs that interact with alpha blockers such as tamsulosin include erectile dysfunction drugs; additive hypotensive effects may occur. The other drugs do not interact with tamsulosin. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 313 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient is taking an alpha blocker as treatment for benign prostatic hyperplasia. The nurse will monitor for which potential drug effect? a. Orthostatic hypotension b. Increased blood pressure c. Decreased urine flow d. Discolored urine ANS: A Orthostatic hypotension can occur with any dose of an alpha blocker, and patients must be warned to get up slowly from a supine position. The other responses are not drug effects of alpha blockers. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 311 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. A beta blocker is prescribed for a patient with angina. The nurse reviews the orders for other drugs that may interact with the beta blocker. Which drugs or drug classes are known to have an interaction with a beta blocker? (Select all that apply.) a. Diuretics b. Anticholinergics c. Penicillins d. Oral hypoglycemics e. Alcohol f. Anticoagulants ANS: A, B, D, E When taken with beta blockers, diuretics and alcohol may cause additive hypotensive effects; oral hypoglycemic medications may cause the blood glucose to decrease; and anticholinergics may cause decreased beta-blocker effects. Penicillins and anticoagulants are not known to interact with beta blockers. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 314 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A patient has an order for carvedilol (Coreg) 6.25 mg twice a day PO. The tablets are 3.125 mg. Identify how many tablets will the nurse administer per dose. _______ ANS: 2 tablets DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 20: Cholinergic Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. When monitoring a patient who is taking a low-dose cholinergic drug, the nurse will watch for which cardiovascular effect? a. Bradycardia b. Tachycardia c. Vasoconstriction d. Palpitations ANS: A The cardiovascular effects of low doses of cholinergic drugs are decreased heart rate (not tachycardia) and vasodilation. Palpitations are not effects of cholinergic drugs. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 323 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. The nurse notes in a patient’s medication history that the patient is taking pilocarpine (Pilocar). Based on this finding, the nurse interprets that the patient has which disorder? a. Anticholinergic poisoning b. Glaucoma c. Bladder atony d. Myasthenia gravis ANS: B Pilocarpine is a direct-acting drug that is used topically to reduce intraocular pressure in patients with glaucoma. The other disorders are not indications for pilocarpine. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 323 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. A patient has had an overdose of an intravenous cholinergic drug. The nurse expects to administer which drug as an antidote? a. Atenolol (Tenormin) b. Bethanechol (Urecholine) c. Dobutamine d. Atropine sulfate ANS: D Prompt administration of atropine sulfate can reverse a toxic dose of cholinergic drugs. The other drugs listed are not antidotes to cholinergic toxicity. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 324 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A patient who has had abdominal surgery has been discharged on a cholinergic drug to assist in increasing gastrointestinal peristalsis. The nurse will teach this patient to look for which therapeutic effect? a. Decreased pulse rate b. Abdominal cramping c. Passage of flatus d. Decreased urge to void ANS: C In patients suffering a decrease in GI peristalsis postoperatively, taking a cholinergic drug should result in an increase in bowel sounds, the passage of flatus, and the occurrence of bowel movements that indicate increased GI peristalsis. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 328 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. A cholinergic drug is prescribed for a patient with a new diagnosis of myasthenia gravis, and the nurse provides instructions to the patient about the medication. What is important to include in the teaching? a. Take the medication with meals to avoid gastrointestinal distress. b. Give daytime doses close together for maximal therapeutic effect. c. Take the medication 30 minutes before eating to improve swallowing and chewing. d. Take the medication only if difficulty swallowing occurs during a meal. ANS: C Taking the medication 30 minutes before meals allows time for the onset of action and therapeutic effects during the meal. The doses should be spaced evenly apart to optimize the effects of the medication. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 327 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A factory worker has been admitted to the emergency department after an industrial accident involving organophosphate insecticides. The nurse will prepare to administer which drug? a. Pilocarpine (Salagen) b. Bethanechol (Urecholine) c. Physostigmine (Antilirium) d. Tacrine (Cognex) ANS: C Indirect-acting drugs such as physostigmine inhibit acetylcholinesterase, thus reversing the neuromuscular blockade produced by anticholinergic poisoning as well as poisoning by irreversible cholinesterase inhibitors such as the organophosphates and carbamates, common classes of insecticides. The other drugs listed are not appropriate antidotes. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 323 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. The nurse is providing teaching regarding drug therapy to the husband of a woman with Alzheimer’s disease. She was diagnosed 3 months ago, has mild memory loss, and will be receiving donepezil (Aricept). What is the drug’s expected action? a. Prevents memory loss in later stages b. Reverses the course of Alzheimer’s disease c. Provides sedation to prevent agitation and restlessness d. May help to improve the mood and decrease confusion ANS: D Donepezil is used to treat mild-to-moderate dementia occurring in Alzheimer’s disease and may improve the symptoms of the disease. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 323 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. A patient has been taking donepezil (Aricept) for 2 weeks as part of the treatment for early stages of Alzheimer’s disease. Her daughter calls the prescriber’s office and is upset because “Mother has not improved one bit!” Which response by the nurse is appropriate? a. “Increase the dosage to twice daily.” b. “It takes time for the cure to take effect.” c. “It may take up to 6 weeks to see an improvement.” d. “Take the medication on an empty stomach for improved absorption.” ANS: C Donepezil therapy is not a cure for Alzheimer’s disease, but it may help to improve symptoms in the early stages. It may take up to 6 weeks to see improvement. The family should be taught that the medication must be taken exactly as ordered and with meals, and the medication should not be abruptly stopped or the dosage increased without the physician’s approval because of the possibility of serious complications. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 328 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Psychosocial Integrity 9. A patient who has been diagnosed with Sjögren’s syndrome will be given cevimeline for the treatment of xerostomia. The nurse will monitor for what therapeutic effect? a. Reduction of salivation b. Stimulation of salivation c. Reduction of gastrointestinal peristalsis d. Improvement of fine-motor control ANS: B Cevimeline is a direct-acting cholinergic drug that is used to stimulate salivation in patients who have xerostomia (dry mouth), one of the manifestations of Sjögren’s syndrome. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 323 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. The nurse is reviewing the mechanism of action of cholinergic drugs. The undesired effects of cholinergic drugs come from the stimulation of which receptors? a. Muscarinic b. Nicotinic c. Cholinergic d. Ganglionic ANS: B Many of the undesirable adverse effects are due to nicotinic receptor stimulation. The desired effects come from muscarinic receptor stimulation. The other options are incorrect. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 323 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient calls the clinic to speak to the nurse about taking an herbal product that contains ginkgo (Ginkgo biloba) to “help my memory.” He states that he has read much information about the herbal product. Which statement by the patient indicates a need for further education? a. “I know the FDA has not approved this herbal product, but I’d like to try it to see if it helps my memory.” b. “I need to watch for possible side effects, such as headaches, or stomach or intestinal upset.” c. “I will take aspirin or ibuprofen (Motrin) if I have a headache.” d. “Ginkgo may cause increased bleeding, so I’ll have to be careful when doing yard work.” ANS: C Drug interactions may occur between the taking of aspirin and nonsteroidal anti-inflammatory drugs and the taking of ginkgo. The other options are incorrect. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 326 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 12. A patient is receiving a dose of edrophonium (Tensilon). The nurse recognizes that this drug is given to determine the diagnosis of which disease? a. Parkinson’s disease b. Multiple sclerosis c. Myasthenia gravis d. Alzheimer’s disease ANS: C Edrophonium, another indirect-acting cholinergic drug, is commonly used to diagnose myasthenia gravis. Edrophonium is not used in diagnosing Parkinson’s disease, multiple sclerosis, or Alzheimer’s disease. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 325 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. A cholinergic drug is prescribed for a patient. The nurse checks the patient’s medical history, knowing that this drug is contraindicated in which disorders? (Select all that apply.) a. Bladder atony b. Gastrointestinal obstruction c. Bradycardia d. Alzheimer’s disease e. Hypotension f. Chronic obstructive pulmonary disease ANS: B, C, E, F Contraindications to the use of cholinergic drugs include gastrointestinal or genitourinary obstruction, bradycardia, hypotension, and chronic obstructive pulmonary disease. The other options are possible indications for cholinergic drugs. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 324 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A patient is receiving memantine (Namenda) 10 mg PO daily. The patient is unable to swallow pills, so an oral solution that contains 2 mg/mL is ordered. Identify how much will the patient receive per dose. _______ ANS: 5 mL DIF: COGNITIVE LEVEL: Applying (Application) REF: N/A TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies Chapter 21: Cholinergic-Blocking Drugs Lilley: Pharmacology and the Nursing Process, 8th Edition MULTIPLE CHOICE 1. The nurse is about to administer a stat dose of intravenous atropine sulfate to a patient who is experiencing a symptomatic cardiac dysrhythmia. During administration of this drug, the nurse will monitor the patient closely for which adverse effect? a. Tachycardia b. Bradycardia c. Ectopic beats d. Cardiac standstill ANS: A Cardiovascular effects of cholinergic blockers include increased heart rate and dysrhythmias. One indication for use is the treatment of sinus bradycardia accompanied by hemodynamic compromise. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 333 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 2. A patient has a prescription for oxybutynin (Ditropan), an anticholinergic drug. When reviewing the patient’s medical history, which condition, if present, would be considered a contraindication to therapy with this drug? a. Diarrhea b. Hypertension c. Neurogenic bladder d. Uncontrolled angle-closure glaucoma ANS: D Contraindications include drug allergy, urinary or gastric retention, and uncontrolled angle-closure glaucoma. Neurogenic bladder is an indication for oxybutynin. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 334 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 3. The nurse is reviewing the use of anticholinergic drugs. Anticholinergic drugs block the effects of which nervous system? a. Central nervous system b. Somatic nervous system c. Sympathetic nervous system d. Parasympathetic nervous system ANS: D Anticholinergic drugs block or inhibit the actions of acetylcholine in the parasympathetic nervous system. The other options are incorrect. DIF: COGNITIVE LEVEL: Remembering (Knowledge) REF: p. 331 TOP: NURSING PROCESS: General MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 4. A patient has received an accidental overdose of intravenous atropine. Which drug will the nurse prepare to administer? a. Atenolol (Tenormin) b. Bethanechol (Urecholine) c. Dicyclomine (Bentyl) d. Physostigmine (Antilirium) ANS: D Physostigmine salicylate is the antidote to an atropine overdose in patients who show extreme delirium or agitation and could inflict injury to themselves. Its routine use as an antidote for cholinergic-blocker overdose is controversial, however. The other options are incorrect choices. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 333 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 5. A 72-year-old man has a new prescription for an anticholinergic drug. He is an active man and enjoys outdoor activities, such as golfing and doing his own yard work. What will the nurse emphasize to him during the teaching session about his drug therapy? a. Drowsiness may interfere with his outdoor activities. b. Increased salivation may occur during exercise and outside activities. c. Fluid volume deficits may occur as a result of an increased incidence of diarrhea. d. He will need to take measures to reduce the occurrence of heat stroke during his activities. ANS: D Elderly patients who take an anticholinergic drug need to be reminded that they are at a greater risk for suffering heat stroke because of decreased sweating and loss of normal heat-regulating mechanisms. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 337 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. The nurse will monitor for which adverse effect when administering an anticholinergic drug? a. Excessive urination b. Diaphoresis c. Dry mouth d. Pupillary constriction ANS: C Anticholinergic drugs commonly cause the adverse effects of dry mouth, blurred vision, constipation, and urinary retention. They also cause mydriasis (pupillary dilation). DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 333 TOP: NURSING PROCESS: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 7. The nurse is reviewing a patient’s medication history and notes that the patient is taking the cholinergic blocker tolterodine (Detrol). Which is an indication for this medication? a. Irritable bowel disease b. Induction of mydriasis c. Urge incontinence d. Reduction of secretions preoperatively ANS: C Tolterodine (Detrol) is used for urinary frequency, urgency, and urge incontinence caused by bladder (detrusor) overactivity. The conditions in the other options are not indications. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 335 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 8. A patient has been taking tolterodine (Detrol), but today her prescriber changed her to a newer drug, darifenacin (Enablex). What advantage does darifenacin have over the tolterodine? a. The newer cholinergic-blocker drugs are more effective. b. It helps reduce urinary retention. c. It can be used in patients with narrow-angle glaucoma. d. The incidence of dry mouth is much lower with darifenacin. ANS: D The incidence of dry mouth is much lower with use of the newer cholinergic-blocker drugs, such as darifenacin, because the actions of these drugs are more specific for the bladder as opposed to the salivary glands. These drugs are contraindicated if narrow-angle glaucoma or urinary retention is present. The newer cholinergic-blocker drugs are not necessarily more effective. DIF: COGNITIVE LEVEL: Understanding (Comprehension) REF: p. 335 TOP: NURSING PROCESS: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 9. The nurse working in a preoperative admitting unit administers an anticholinergic medication to a patient before surgery. What is the purpose of this drug in the preoperative setting? a. Control the heart rate b. Relax the patient c. Reduce urinary frequency d. Reduce oral and gastrointestinal secretions ANS: D Anticholinergic drugs are given preoperatively to control oral and gastrointestinal secretions during surgery. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 333 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 10. In preparation for eye surgery, the nurse monitors for which desired drug effect in a patient who is receiving a cholinergic-blocking eyedrop medication? a. Miosis b. Mydriasis c. Increased intraocular fluid production d. Enhanced tear production ANS: B Cholinergic-blocking eyedrops cause dilation of the pupil (mydriasis) and paralysis of the ocular lens (cycloplegia), both of which are important for eye surgery. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 332 TOP: NURSING PROCESS: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. A patient has a new prescription for the transdermal form of scopolamine. The nurse knows that this form of scopolamine is used for which condition? a. Angina b. Chronic pain c. Hypertension d. Motion sickness ANS: D Transdermal scopolamine (Transderm-Scop) is a patch that can be applied just behind the ear 4 to 5 hours before travel for the prevention of motion sickness. The other options are incorrect. DIF: COGNITIVE LEVEL: Applying (Application) REF: p. 335 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 1. The nurse is reviewing the indications for atropine sulfate. Atropine is appropriate for which of these patients? (Select all that apply.) a. A patient who has suddenly developed symptomatic bradycardia with a heart rate of 32 beats/min b. A patient who has suddenly developed symptomatic tachycardia with a heart rate of 180 beats/min c. A patient with severe narrow-angle glaucoma d. A patient who is about to have surgery e. A patient newly diagnosed with myasthenia gravis f. A patient with anticholinesterase inhibitor poisoning ANS: A, D, F Anticholinergic drugs are used for symptomatic bradycardia and certain other cardiac conditions. It is given preoperatively to control secretions during surgery and is used as an antidote for anticholinesterase inhibitor poisoning. The other options are contraindications to the use of atropine. DIF: COGNITIVE LEVEL: Analyzing (Analysis) REF: p. 334 TOP: NURSING PROCESS: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 1. A patient is to receive glycopyrrolate (Robinul) 4 mcg/kg IM 30 minutes before a procedure. The patient weighs 110 pounds; the medication is available in a strength of 0.2 mg/mL. Identify how many milliliters of medication will the nurse draw up into the syringe. _______ ANS: 1 mL To calculate mcg/kg, multiply The patient will receive 200 mcg, or 0.2 mg. The medication is available in a strength of 0.2 mg/mL; therefore, the patient will receive 1 mL. Ch.1 questions 1. 1.ID: 10242258563 In which step of the nursing process does the nurse determine the suitability of a pharmacotherapeutic regimen? • Planning • Evaluation Correct • Assessment • Implementation Evaluation is the part of the nursing process that includes monitoring whether patient goals and outcome criteria related to the nursing diagnoses are met. Monitoring includes observing for therapeutic effects of drug treatment as well as for adverse effects and toxicity. Awarded 1.0 points out of 1.0 possible points. 2. 2.ID: 10242258561 Which statement is an example of objective data? (Select all that apply.) • The patient states that she has a headache. • The patient has clear urine. Correct • The patient says that she feels like someone is touching her arm. • The patient has had a fever for 5 days. Correct • The patient says that she has felt tired for almost a week. Subjective data includes information shared through spoken word by any reliable source, such as the patient, spouse, family member, significant other, and/or caregiver. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242258559 What things should the nurse check when reviewing a prescription with a patient? (Select all that apply.) • The patient's home address • The route of administration Correct • The age of the patient • The signature of the prescriber Correct • The patient's emergency contact Once assessment of the patient and the drug has been completed, the specific prescription or medication order from any prescriber must be checked for the following six elements: (1) patient's name, (2) date the drug order was written, (3) name of drug(s), (4) drug dosage amount and frequency, (5) route of administration, and (6) prescriber's signature. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242258567 What information should the nurse chart when documenting medication administration? (Select all that apply.) • The time of administration Correct • Information about an "incident report" in the patient's chart • The patient's age • The route of administration Correct • The dosage of medication administered Correct Documentation of administration should include the other five rights, as well as patient response, teaching related to the medication, if the medication is not given, refusal of medication, and reason for refusal. Medication errors should be noted on an incident report, but should not be documented as an incident report in the patient's chart. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242258565 The nurse plans care for a male patient who is 80 years old. The nursing diagnosis is noncompliance with the medication regimen related to living alone, as evidenced by uncontrolled blood pressure. What should the nurse do next? • Enlist the help of a home care nurse for pharmacotherapy Correct • Examine the results of nursing help with the medications • Collaborate with the provider on a new medication regimen • Assess the impact of home self-management of medications After establishing the nursing diagnosis, the nurse plans care by determining the nursing goals and outcome criteria. As a means of working toward blood pressure control, the nurse chooses to set up nursing assistance for the patient in the home. The home care nurse can help the patient adhere to the therapeutic regimen by making a medication schedule and dispensing medication into a pill box, among other strategies. The nurse assesses the patient before establishing the nursing diagnosis and evaluates care after implementing the plan. Collaboration on a new medication regimen is not indicated. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-cq1k-eziumpxi!reviewSubmittedAssessmentAttempt?attempt=17651315648> Ch.2 questions • 1.ID: 10242192647 Which aspect of pharmacology does the nurse use in understanding a medication's mechanism of action? • Pharmaceutics • Pharmacokinetics • Pharmacodynamics Correct • Pharmacotherapeutics Pharmacodynamics is the study of the biochemical and physiologic interactions of drugs at their sites of activity. It examines the physiochemical properties of drugs and their pharmacologic interactions with body receptors. Pharmaceutics is the science of preparing and dispensing drugs, including dosage form design. Pharmacokinetics is the study of what happens to a drug from the time it is put into the body until the parent drug and all metabolites have left the body. Pharmacotherapeutics is the treatment of pathologic conditions through the use of drugs. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242192633 Which aspects of the pharmacotherapeutics of a medication does the nurse use in planning care? (Select all that apply.) • Goals of treatment Correct • Distribution of drug • Condition of patient • Mechanism of action Correct • Route of metabolism • Indication for therapy Correct Pharmacotherapeutics involves the use of medication in the clinical setting for treatment of disease. One aspect of pharmacotherapeutics is the establishment of treatment goals and outcome criteria with which to evaluate the effect of therapy. These goals and outcome criteria are not the same as the nursing goals and outcome criteria. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242192685 Which factor is a major determinant of how a medication is absorbed? • First-pass effect of the liver • Elimination by the intestines • Rate of distribution to tissues • Formulation of the medication Correct One major factor in the determination of medication absorption is the formulation of the medication, because to exert its therapeutic effect the drug must reach the site of the drug's action. The formulation determines the route taken by a medication to get to that site. For example, an extended-release capsule should be swallowed whole because the formulation is designed to release the medication into the gastrointestinal tract. As the drug molecules release the active ingredient slowly over time, the active ingredient is absorbed gradually by the small intestine. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242192668 Which drug name is likely to have the most variations for a single compound? • Trade Correct • Generic • Prodrug • Chemical Drugs may be marketed under many different trade (brand) names because different companies, which compound the same combination of chemicals, may market that chemical under names they choose; for example, acetaminophen (generic name) has more than 20 trade names. In addition, the same chemical may be found in many different formulations and in combination with other drugs, all of which have different brand names. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242192631 The nurse is ordered to administer an enteral medication. What is the correct route of administration? • Oral Correct • Buccal • Intravenous • Subcutaneous Enteral drug administration requires drug absorption into the systemic circulation by way of the gastric mucosa or the intestines. Buccal administration allows drug absorption into the circulation by way of the vascular bed under the tongue. Parenteral administration involves any route outside of the gastrointestinal tract, but it usually involves administration of the drug by means of injection. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242192655 A patient is admitted for acute alcohol withdrawal, and the nurse checks the site of metabolism for each medication on the patient's medication record. Medications metabolized at which site are of greatest concern for the nurse? • Liver Correct • Lungs • Muscle • Kidney The nurse notes medications subject to hepatic metabolism, because the patient with acute alcohol withdrawal is likely to have impaired liver function. If such medications are administered, the patient will be less able to transform the medication into inactive metabolites. This can result in the circulation of a higher-than-normal concentration of the active metabolite for a longer period, compared with metabolism of the drug in an individual with normal liver function. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242195402 Trace the route of an orally administered medication by ranking these events in order of occurrence: Correct 13. Absorption from the intestines 14. Transportation to liver 15. Metabolism by enzymes 16. Passage into the circulation After oral administration, suitable formulations of the medication are absorbed through the intestines and taken to the liver, where hepatic enzymes transform the active metabolite into an inactive metabolite. The active metabolite is passed into the circulation, and the inactive metabolite is excreted. Awarded 1.0 points out of 1.0 possible points. 17. 8.ID: 10242192637 The term first-pass effect refers to the rapid inactivation of some oral drugs as they pass through what? • Liver Correct • Stomach • Small intestine • Portal circulation The term first-pass effect refers to the rapid inactivation of certain oral drugs as they pass through the liver, which renders their bioavailability less than 100%. Drugs absorbed from the gastrointestinal tract are carried directly to the liver by way of the hepatic portal circulation. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242192698 Which route of administration supplies the highest bioavailability? • Enteral • Transdermal • Subcutaneous • Intramuscular Correct Medications administered by means of intramuscular (IM) injection have a higher bioavailability than enterally, transdermally, or subcutaneously administered medications, because IM injections bypass the first-pass effect of the liver and have the fewest obstacles to absorption of the medication. Subcutaneous injections have the next highest bioavailability, followed by the enteral and transdermal routes of administration. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242192643 Which analgesic would be most effective: morphine (an agonist) or pentazocine (a partial agonist)? • An agonist Correct • An antagonist • A partial agonist • A partial antagonist A partial agonist is an agonist with moderate intrinsic activity. The maximum potential effect of a partial agonist is lower than that of a full agonist, such as morphine sulfate. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242192690 Which medication information helps the nurse maintain a serum drug level within the therapeutic index? (Select all that apply.) • Toxic effects Correct • Patient illnesses • Nutritional status • Serum drug level Correct • Site of metabolism Correct • Route of excretion Correct The therapeutic index, a measure of a drug's safety, is defined as the ratio of a drug's toxic level to the serum level that produces a therapeutic effect. A large therapeutic index indicates that a drug is relatively safe, and a small therapeutic index indicates that a drug is relatively unsafe. The nurse uses information about toxic effects and the serum drug level for patient monitoring. The site of metabolism and route of excretion provide the nurse direction in regard to which laboratory data to monitor and potential drug-drug interaction from other substances taken by the patient that are metabolized or excreted in the same manner. Patient illnesses and nutritional status are patient data but not medication information. Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242192694 When would it be safe to administer morphine sulfate with another medication that has an additive effect with morphine sulfate? • When the metabolism of morphine is increased • When a lower dose of each medication may be given Correct • When the risk of allergic reactions is reduced • When the therapeutic effect of morphine is increased Using an additive effect to administer morphine sulfate with another medication is a safer method for achieving a therapeutic effect, because a lower dosage of each medication can be used. This is important when morphine sulfate is being administered because adverse effects of therapy with this drug include respiratory depression; a lower dose of morphine is less likely to cause respiratory depression. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242195400 When administered intravenously, phenytoin (Dilantin) must be infused in 0.9% NaCl solution because phenytoin precipitates when given in a glucose solution. Which term describes the relationship between phenytoin and glucose? • Synergistic • Incompatible Correct • Antagonistic • Idiosyncratic Phenytoin and glucose solutions are incompatible because when they are mixed together the phenytoin precipitates out into the solution. The precipitate cannot and should not be administered to the patient. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242192696 The health care provider prescribes one dose of epinephrine (Adrenaline) 0.1 mg during cardiopulmonary resuscitation. What is the best route of administration for this medication? • Buccal • Intravenous Correct • Transdermal • Subcutaneous The best route of administration for this medication is intravenous because the patient is in circulatory collapse, meaning that drug distribution and absorption are severely compromised. The patient needs medication to be administered directly into the circulation to bypass the absorption and distribution delays inherent in the topical and subcutaneous routes. Medication administered under the tongue (buccal route) is absorbed rapidly but not as quickly as medication administered intravenously. Awarded 1.0 points out of 1.0 possible points. • 15.ID: 10242192641 The nurse administers two medications, A and B. B prolongs the peak plasma level of A without altering its chemical composition. B inhibits which phase of the pharmacokinetics of A to achieve this effect? • Excretion Correct • Absorption • Metabolism • Distribution B inhibits the excretion of A to increase and prolong the peak plasma level of A. Decreased metabolism of a drug can increase and prolong peak drug levels, too; however, metabolism alters the chemical composition of the drug. Awarded 1.0 points out of 1.0 possible points. • 16.ID: 10242192645 Which condition is likely to alter absorption of a medication? (Select all that apply.) • Hypoalbuminemia • Increased gastric pH Correct • Poor tissue perfusion • Hepatic insufficiency • Drug-drug interaction Correct • Binding site competition Drug absorption is altered by any factor that affects the movement of the drug from the administration site into the bloodstream, where it is distributed. Absorption can be altered through drug-drug interactions that enhance or impair the movement and through changes in gastric pH that increase or decrease the capacity of the drug to cross the intestinal membranes. Competition for binding sites, hypoalbuminemia, and poor tissue perfusion are examples of altered distribution. Impaired liver function is likely to impair a drug's metabolism. Awarded 1.0 points out of 1.0 possible points. • 17.ID: 10242195413 The nurse monitors the patient for which action when food increases the rate of absorption of a medication? • Altered metabolism • Enhanced peak effect Correct • Low therapeutic effect • Short duration of action When food increases the rate of absorption of a drug, onset of action is shorter and peak effects are heightened because the increased rate of absorption increases the concentration of the drug at the site of action. The drug is metabolized in the same manner, regardless of the rate of absorption; the therapeutic effect is likely to be heightened; and the duration of action will remain constant. Awarded 1.0 points out of 1.0 possible points. • 18.ID: 10242192639 In completing a health history of a patient, which fruit juice would the nurse be most concerned about in regard to the risk for a food-drug interaction? • Apple • Orange • Cranberry • Grapefruit Correct Grapefruit juice can inhibit the metabolism of certain drugs, possibly leading to increased blood levels of these drugs. The clinical consequences of taking drugs with grapefruit juice may be good or bad; for this reason, it is recommended that grapefruit be avoided with all medications. Awarded 1.0 points out of 1.0 possible points. • 19.ID: 10242192635 The nurse is monitoring patients for adverse drug reactions. Which of these patients is nurse's priority? • A 72-year-old taking codeine for lumbar muscle pain • A 22-year-old who takes two allergy drugs for hay fever • A 12-month-old who has been given acetaminophen for fever • A 68-year-old with a severe infection who receives three antibiotics Correct The patient at the highest risk of an adverse drug reaction is the individual taking three antibiotics for a severe infection. Multiple medications increase risk, and antibiotics can cause renal dysfunction. So, in a patient taking three antibiotics, the risk for renal dysfunction is high. The 12-month-old and 72-year-old patients are in high-risk groups for adverse drug effects and are the nurse's next highest priority. The 22-year-old has a lower risk than the other patients for adverse drug effects. Awarded 1.0 points out of 1.0 possible points. • 20.ID: 10242195408 Which drug should the nurse avoid administering to a patient with a deficiency in glucose-6-phosphate dehydrogenase (G6PD)? • Venlafaxine (Effexor) • Metoprolol (Lopressor) • Amoxicillin (Amoxil) • Aspirin (Bayer Aspirin) Correct The nurse avoids administering aspirin and aspirin products to a patient with a G6PD deficiency because the patient lacks an important enzyme for the metabolism of aspirin and, therefore, is at risk for drug-induced hemolysis. Awarded 1.0 points out of 1.0 possible points. • 21.ID: 10242192651 The nurse recognizes that gastric irritation associated with aspirin administration is what? • A medication error • An idiosyncratic effect • An adverse drug effect Correct • A sign of drug toxicity Adverse effects of medication (adverse drug reactions, or ADRs) are unexpected and undesirable, and they occur at therapeutic drug levels. Many ADRs are common, they may or may not be preventable, and mild ADRs do not require a change in the patient's therapeutic regimen. Other ADRs are life threatening and quite dangerous. ADRs can be caused by medication errors. Gastric irritation is an ADR associated with aspirin, so the reaction is not idiosyncratic. Aspirin toxicity can occur without gastric irritation. Awarded 1.0 points out of 1.0 possible points. • 22.ID: 10242192692 A patient with renal failure is taking a medication that is eliminated by the kidneys. Which action would the nurse expect to be taken based on the level of kidney function? • Increased bioavailability • Decreased dosage ordered Correct • Lower rate of drug toxicity • Increased dosing frequency The dosage of medication eliminated by the kidney must be reduced in the patient with renal failure to prevent drug accumulation and toxicity. Bioavailability will not be altered in this patient because the problem involves drug elimination, not absorption. Impaired drug elimination is more likely to necessitate fewer doses and a higher rate of toxicity because the drug remains in the bloodstream longer. Awarded 1.0 points out of 1.0 possible points. • 23.ID: 10242192649 The nurse administers two medications that use cytochrome P-450 enzymes; however, one of these drugs is an enzyme inhibitor. Which aspect of pharmacokinetics is most likely to be affected by the enzyme inhibitor? • Absorption • Metabolism Correct • Distribution • Elimination The liver can metabolize a wide range of medications because of the cytochrome P-450 enzymes. These enzymes play a large role in drug-drug interactions. When one drug is an enzyme inhibitor, it inhibits the P-450 enzyme of another, resulting in a higher circulating drug level, prolongation of the drug's effect, and increased risk of toxicity. Awarded 1.0 points out of 1.0 possible points. • 24.ID: 10242192673 Which medication is most likely to demonstrate variation in its bioavailability? • Morphine sulfate 10 mg IV • Hydrochlorothiazide tablets Correct • Rectal suppositories for nausea • Nitroglycerin transdermal patches Hydrochlorothiazide tablets are most likely to exhibit variations in their pharmacokinetics because oral medications are subject to factors that can delay or enhance absorption. In addition, these drugs are subject to first-pass metabolism, in which the drug is processed into active and inactive metabolites before being passed into the bloodstream. Awarded 1.0 points out of 1.0 possible points. • 25.ID: 10242192653 A patient with which condition is most likely to experience increased drug absorption? • Dumping syndrome • Loose, watery stools • Stomach after a meal • Slow intestinal motility Correct Slow intestinal motility can enhance absorption of medication by prolonging the time available for absorption. Dumping syndrome and loose stools are conditions with increased intestinal motility and, therefore, decreased time for intestinal absorption. The presence of food in the stomach slows the absorption of most drugs without reducing the total amount absorbed. Awarded 1.0 points out of 1.0 possible points. • 26.ID: 10242192663 The nurse prepares to administer pain medication to a patient who underwent abdominal surgery 30 minutes ago and who has a temperature of 97.2° F. Which routes of medication administration will the nurse avoid using because of the patient's temperature? (Select all that apply.) • Oral • Rectal • Intrathecal • Intravenous • Intramuscular Correct • Subcutaneous Correct The nurse avoids subcutaneous and intramuscular administration of medication because the patient is hypothermic and vasoconstricted with a poor blood supply. If the nurse injects medication into the poorly perfused tissue while the patient is cold, the medication will not be absorbed, and the therapeutic effect will not be realized. In addition, when the patient warms up, any medication injected into cold tissue will be absorbed, possibly resulting in an overdose of pain medication if other medication has been administered in the meantime. The nurse avoids administering oral medication because oral intake in the immediate postoperative phase is usually contraindicated; however, this is unrelated to the patient's temperature. Rectal administration of pain medication is theoretically suitable, but most pain medications are not formulated for rectal administration. In the immediate postoperative phase, intrathecal and intravenous administration are the preferred routes for pain medication. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-7w2t-o4jumpxi!reviewSubmittedAssessmentAttempt?attempt=17651482582> Ch.3 questions • 1.ID: 10242258511 The nurse wants to minimize fetal exposure to drugs in a patient who is 26 weeks' pregnant. Which type of medication warrants nursing verification of adequate maternal renal and kidney function? • A medication that binds to protein in serum • A medication that has 100% renal clearance • A medication that crosses the blood-brain barrier • A medication that diffuses across the placenta Correct To minimize fetal exposure to drugs, the nurse checks the medication list for substances that cross the placenta, which increases fetal exposure. With adequate maternal liver and kidney function, medication is metabolized and eliminated properly, thereby minimizing fetal exposure to that substance. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242258527 At which gestational age does an embryo or fetus have the highest risk for drug-induced developmental defects as a result of teratogenic exposure? • 4 weeks' gestation Correct • 16 weeks' gestation • 29 weeks' gestation • 38 weeks' gestation Drug-induced developmental defects are most likely during the embryonic period, the first trimester of pregnancy. During the first 13 weeks, the basic shapes of internal organs and other structures are being established. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242258525 Which type of drug, according to the Drug Risk Category system set forth by the U.S. Food and Drug Administration, is the most dangerous for a fetus? • A • B • D • X Correct Drugs in Category X are the most dangerous to the developing embryo or fetus. Category X drugs are known to cause human fetal harm, and their risk to the fetus outweighs any possible therapeutic benefit. Drugs in Category A expose the fetus to no risk; drugs in Categories B, C, and D are progressively more dangerous than those in Category A but less dangerous than drugs in Category X. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242258509 The nurse prepares medication for a 24-year-old patient who is 30 weeks' pregnant and has hypoalbuminemia. Which factor related to drug safety in pregnancy is the nurse's priority to reduce the risk of excessive drug exposure to the fetus when planning care for this patient? • Age of the patient • Distribution of the drug Correct • Gestational age of the fetus • Serum sodium of the patient For a pregnant patient with a low serum albumin level, the nurse's priority is the distribution of the drug in the patient. If a patient with inadequate serum protein takes a drug that is highly protein bound, more of the active ingredient of the drug will circulate in the pregnant patient because the blood lacks protein to which the drug normally binds; thus, the fetus is exposed to a higher-than-normal serum level of that drug. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242258523 Which factor related to normal infant physiology is most likely to affect the onset of action for an oral medication absorbed in the intestines of a 4-month-old infant? • Low glomerular filtration • Slow, irregular peristalsis Correct • Liver enzyme inadequacy • Decreased protein binding Peristalsis can be slow and irregular in an infant younger than 6 to 8 months; for drugs that are absorbed primarily from the intestine, absorption is delayed and, therefore, the onset of action is also delayed. A low glomerular filtration impairs renal clearance of drugs, inadequate liver enzymes impair drug metabolism, and decreased protein binding increases the serum drug level and prolongs the infant's exposure to the drug. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242258507 Which characteristics of an infant does the nurse assess to control drug absorption as a means of helping prevent adverse drug effects? (Select all that apply.) • Skin integrity Correct • Liver enzymes • Serum albumin • Drug properties Correct • Peristaltic action Correct • Serum creatinine The nurse assesses characteristics of the infant because delayed or accelerated drug absorption can affect the onset of drug action and the infant's exposure to the drug's effects. The nurse assesses the skin because an infant's skin is thinner than an adult's and can absorb topical medication more readily. Drug properties, including the drug's chemistry or concurrently administered drugs, can affect drug absorption as well. Peristaltic action is assessed because slow peristalsis can increase absorption if the drug is absorbed in the stomach or the intestines. Liver enzymes affect biotransformation, serum albumin affects distribution, and renal function affects drug elimination. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242258521 The nurse checks the dosage calculation of a medication that acts on the central nervous system (CNS) for accuracy before administering the drug to an infant. Why does the nurse check the calculation? • Infants have slower drug metabolic rates. • Infants have adequate serum protein levels. • Infants have wide fluctuations in their weight. • Infants have immature blood-brain barriers. Correct The blood-brain barrier is not fully developed at birth; because of this, drugs enter the CNS more easily, thereby rendering the infant especially sensitive to drugs that affect CNS functions such as respiration. Because the nurse bases dosages on infant weight, the nurse calculates the dosage at regular intervals to ensure the proper dosage of a given medication for the infant's current weight. The metabolic rate of an infant is affected by many factors, and it is not necessarily inadequate. Because of immature hepatic function, the levels of plasma proteins produced by the liver are likely to be lower than they are in an adult. Finally, an infant's weight may vary, and such variation can necessitate a significant change in dosage; however, the weight variation is more likely to be a small one. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242258531 Which information does the nurse use to calculate a pediatric drug dose on the basis of the patient's weight? (Select all that apply.) • Patient's weight in kilograms Correct • Amount to be administered per day • Drug order from the prescriber Correct • Minimum daily dose for the patient • Guidelines from the drug formulary Correct • Usual 24-hour dose range Correct The nurse uses the patient's weight in kilograms to calculate a pediatric dose because weight-based dosage calculations are given in milligrams per kilogram of body weight. The nurse also uses the drug order from the prescriber as a critical variable in the equation because the order establishes the amount of the drug per kilogram of the patient's weight that should be administered. After calculating the 24-hour dose, the nurse compares it to the dose range from the formulary to ensure that the prescribed dose falls within the recommended range. The minimum daily dose is a part of the 24-hour dose range. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242258533 Which knowledge about older adult patients in relation to younger ones does the nurse apply before administering a medication? (Select all that apply.) • Superior drug therapy adherence • Less prescription drug sensitivity • Higher incidence of self-medication errors Correct • Higher incidence of adverse drug reactions Correct • Lower risk of drug-drug interactions • Altered pharmacokinetic processes Correct Because older adult patients are more likely to have complex drug regimens and to be subject to polypharmacy, they are more likely to commit self-medication errors and are at a higher risk for adverse drug effects. This is especially true of an older adult with impaired sensory, cognitive, or motor function. Older adults are likely to have altered pharmacokinetics and altered sensitivity to drugs as a result of declining organ function and drug-drug interactions. Older adults do not necessarily adhere to therapy regimens better than younger adults do, and they are at higher risk for drug-drug interactions because older adults tend to take more medication than younger adults do. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242258513 The nurse prepares to administer a drug that is absorbed in the stomach to an older adult patient. Drug absorption in this patient is likely to be what? • Increased as a result of diminished peristalsis Correct • Increased by altered portal blood flow • Slowed as a result of excessive gastric acidity • Slowed as a result of delayed gastric emptying Many factors can alter the absorption of drugs in older adults. The delayed gastric emptying associated with diminished peristaltic action can increase absorption of a drug that is absorbed in the stomach because the delay exposes the gastric mucosa to the drug for a longer period. Altered portal blood flow affects drug distribution, and older adults tend to have less gastric acid secretion. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242258515 A malnourished older adult patient experiences drug toxicity. Which factor does the nurse assess to rule out drug distribution as a cause of the patient's toxicity? • Drug dosage • Drug half-life • Gastric acidity • Plasma proteins Correct A malnourished older adult is likely to have a smaller percentage of lean muscle and lower levels of circulating plasma proteins. The result is fewer protein-binding sites, increased serum drug levels, and intensified drug effects. An error in drug dosage is a prescribing error, the half-life is an issue of metabolism, and gastric acidity involves drug absorption. Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242258529 To evaluate renal function accurately and reliably in an older patient, the nurse examines what? • The patient's blood urea nitrogen • The patient's creatinine clearance Correct • The patient's conjugated bilirubin • The patient's urine specific gravity Creatinine clearance is a sensitive and specific test of renal function because it is an indication of glomerular filtration and is less affected by confounding factors such as percentage of lean muscle mass or nutritional status. Although urine specific gravity is an indicator of the kidney's ability to concentrate urine, it and the blood urea nitrogen concentration are nonspecific indicators of renal function. Bilirubin is an indicator of liver function. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242258519 Which factors contribute to a higher incidence of adverse drug reactions in older adult patients? (Select all that apply.) • Increased incidence of falling • Increased fibrosis of liver • Decline in organ function Correct • Complexity of therapy Correct • Slower filtration in kidneys Correct • Higher drug levels in serum Adverse drug interactions are more common in older adult patients than in younger ones because organ function declines slowly with age, drug therapy for older adults tends to be more complex, and glomerular filtration in the kidneys is slower. Adverse drug reactions contribute to an increased incidence of falls, liver fibrosis is not common in older adults, and the older adult is at risk for higher circulating drug levels if the patient is hypoalbuminemic. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242258517 The nurse plans care for an older adult male patient with a complex drug regimen. Which action should the nurse implement to decrease the risk of patient nonadherence to therapy? • Instructing the patient to call for information about the drug therapy • Providing the patient with written instructions for all drugs prescribed Correct • Encouraging the use of multiple alarms for drug reminders • Suggesting home remedies to counteract adverse effects To decrease the risk of patient nonadherence to a complicated drug regimen, the nurse provides written instructions for all drugs that the patient takes and tries to simplify the regimen. Written instructions provide the patient with a reliable reference and a reminder for self-administration at home, and the regimen is simplified when the nurse compiles the information into a single medication schedule. The nurse breaches the duty owed to the patient by delegating proper instructions to the patient; telephone-based support or source of reference is suitable once drug therapy instructions have been delivered properly by the nurse. The use of multiple alarms increases the complexity, as well as the potential cost, of an already complex situation. The nurse instructs the patient to avoid home remedies and over-the-counter medications without the prior approval of the prescriber. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-2r2l-hajumpxi!reviewSubmittedAssessmentAttempt?attempt=17659571123> Ch.4 • 1.ID: 10242205080 Which strategies should the nurse implement to provide culturally competent nursing care? (Select all that apply.) • Performing a comprehensive cultural assessment of every patient Correct • Incorporating the patient's cultural beliefs into the plan of care Correct • Assessing the patient for nonpharmacologic and pharmacologic therapies Correct • Updating the nurse's basic knowledge of the nursing process Correct • Matching the ethnicity and culture of the patient to the patient's assigned nurse • Promoting personal health beliefs and practices that benefit the patient As a means of delivering culturally competent nursing care to an ethnically diverse population, the nurse provides holistic and individualized care based on the patient's cultural assessment; this assessment includes cultural practices and pharmacologic and nonpharmacologic therapies. In addition, the nurse provides nursing care based on the framework of the nursing process. The nurse avoids imposing personal beliefs on the patient and assigns nursing staff to the patient on the basis of the patient's needs. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242205076 A patient is experiencing an unusual response to a medication, and the nurse suspects nonadherence to the therapeutic regimen. Which cultural factor is the most likely to influence a patient's adherence to prescribed therapy? • Citizenship • Family expectations Correct • Financial difficulties • Acetylator deficiency Family expectations of therapy are a potential source of cultural influence on the patient's compliance with therapy. When the patient does not receive support or positive feedback from the family, the risk of noncompliance increases. Lack of acetylators is a genetic influence; financial issues are an environmental influence. The patient's citizenship is not related to nonadherence unless it is associated with a certain health practice or belief. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242205082 The U.S. Food and Drug Administration (FDA) has the least amount of influence over which substances? • Opioid analgesics • Vitamins and herbs Correct • Experimental drugs • Electrolytic solutions Because they are designed and marketed as dietary supplements rather than as drugs, vitamins and herbs are a group of substances over which the FDA has had little regulatory authority. However, since 1994, manufacturers of vitamins and herbs have been required to ensure the safety of their products. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242205078 Which population groups may use heat, cold, and herbal remedies? (Select all that apply.) • Asians Correct • Hispanics Correct • African Americans • Native Americans • European Americans Some Asian and Hispanic individuals may use heat, cold, and herbs as remedies. Some African Americans may practice folk medicine and may use oils and roots as health remedies. Some Native Americans may believe in harmony with nature and ill spirits causing disease. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242205074 Which ethnic group has the least effective response to beta-blockers? • Whites • African Americans Correct • Asians • Hispanics African Americans respond better to diuretics than to beta-blockers and angiotensin-converting enzyme inhibitors. Beta-blockers are much less effective in this population than they are in other populations. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-4b5f-ngjumpxi!reviewSubmittedAssessmentAttempt?attempt=17660322622> Ch.5 questions • 1.ID: 10242224847 Which property of a drug is most likely to reduce the risk of medication errors? • Low dosage • Economical forms • Once-a-day dosing Correct • Oral administration Drugs administered once a day are more likely to have a lower incidence of medication errors because fewer doses are involved. Once-a-day dosing also increases the likelihood of patient adherence to therapy. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242224849 Which factor is the primary reason for medication errors in acute care facilities? • Individual error • System weakness Correct • Complex therapy • Prescription error The main reason for medication errors is a system weakness, such as the creation of a punitive health care culture for the reporting of medication errors, ineffective procedures, and lack of education. Individual errors, complex therapies, and prescription errors are also potential causes of medication errors; however, the potential for error is smaller than that with system weaknesses. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242224845 Which health care professional is least likely to detect medication errors in a hospital setting personally? • Medication prescriber Correct • Pharmacy technician • Hospital pharmacist • Registered nurse Medication orders are processed by several health care professionals before the drugs are administered to the patient. The process begins when the prescriber writes the order. Once the order has been written, the prescriber delegates responsibility for medication administration to the pharmacist and the nurse. Because the prescriber is not involved in the process thereafter, this person is unlikely to detect a medication error after writing an order. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-kk9u-xmjumpxi!reviewSubmittedAssessmentAttempt?attempt=17660340762> Ch.6 questions • 1.ID: 10242217157 The nurse prepares to teach self-administration of insulin to a patient with a history of uncontrolled diabetes mellitus. Because of the peripheral complications of diabetes, what should the nurse remember while conducting the teaching? • To speak in front of the patient directly • To increase the time allotted for return demonstrations Correct • To keep all materials within the patient's visual field • To use high-contrast materials (e.g., black and white) A patient with uncontrolled diabetes is likely to have peripheral neuropathies, including an impaired sense of touch. As a result, the nurse would allow more time for return demonstrations because the patient is likely to have difficulty executing psychomotor skills. The nurse lowers the pitch of the voice when speaking to a patient who is hearing impaired, keeps printed materials within the patient's visual field when the patient has impaired peripheral vision (e.g., glaucoma), and uses high-contrast materials for patients who have difficulty discriminating colors. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242217155 The nursing diagnosis for a patient is ineffective therapeutic regimen maintenance. Which is the most important nursing intervention for the plan of care? • Providing medications for inspection • Determining the inclination for learning Correct • Completing a medication dosing calendar • Including family members when appropriate The main goal for the patient's learning is to improve patient adherence to therapy. After determining that the patient is not complying with the therapeutic regimen, the nurse must assess the patient's readiness for learning because patient teaching is likely to be ineffective if the patient is not motivated or ready to learn. Once the patient is inclined to learn, the nurse individualizes teaching to include inspecting the medications to develop familiarity, developing a dosing calendar, and including family members when suitable or necessary. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-c3a8-ltjumpxi!reviewSubmittedAssessmentAttempt?attempt=17660360758> Ch. 7 • 1.ID: 10242250581 Which descriptions apply to the market for medicinal herbs in the United States? (Select all that apply.) • Growing in numbers of users Correct • Used with traditional therapies Correct • Less than $1 million in sales annually • Used by less than 10% of the population • Viewed with growing skepticism • Heavily regulated by federal law The market for herbal remedies is growing, with over-the-counter (OTC) medications now accounting for about 60% of all medications used in the United States. Herbal remedies may be used in traditional therapies. It is a largely unregulated market, generating billions of dollars in sales annually. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242250579 What is the best description of the consumer safety precautions for herbal supplements? • Reliable data on product efficacy is scarce. Correct • Herbs in tamper-resistant containers are safe. • Medicinal herbs are under strict U.S. Food and Drug Administration control. • The package labeling clearly states product safety. Some herbal preparations are effective; many are not. A few can cause harmful or lethal effects. Herbal products are exempt from meaningful regulation. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242250593 Which entity regulates medicinal herbs? • FDA • AMA • DSHEA Correct • USDA Medicinal herbs are regulated under the Dietary Supplement Health and Education Act of 1994 (DSHEA), a piece of legislation created to define dietary supplements and regulations for their sale. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242250587 A patient with atrial fibrillation requests a cup of chamomile tea. The nurse denies the patient's request because of the medication the patient is taking. What is the medication? • Cardiac glycoside • Unfractionated heparin Correct • Beta-adrenergic blocker • Calcium channel blocker The nurse denies the patient's request for chamomile tea because chamomile can increase the risk of bleeding in a patient taking anticoagulants. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242252206 A male patient who abuses alcohol tells the nurse that he is treating himself with kava. Which instruction should the nurse include in patient teaching? • Use another herb beside the kava. • Use either the kava or the alcohol. • Avoid using the kava with alcohol. • Stop taking the kava now. Correct The nurse should instruct the patient to stop taking kava now because kava can enhance the effects of alcohol, a depressant, possibly resulting in respiratory arrest. This is a nursing priority because it involves an immediate, potentially life-threatening issue. The nurse would avoid suggesting the use of a substance that the patient abuses, and so in this case would avoid a recommendation to use the kava or the alcohol. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242250598 A patient who takes ginseng to improve memory takes many prescription drugs as well. Which laboratory parameter should the nurse check before administering medication as a means of assessing the pharmacokinetic effect of ginseng in this patient? • Mental status • Liver enzymes Correct • Urine bilirubin • Serum creatinine Ginseng can alter drug metabolism and, as a result, drug distribution and elimination. To evaluate the potential for altered pharmacokinetics of the patient's prescription drugs, the nurse checks the liver enzymes as an indicator of liver function because the liver is the main site of drug metabolism in the body. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-80vi-d1kumpxi!reviewSubmittedAssessmentAttempt?attempt=17660371532> Ch. 8 questions • 1.ID: 10242223881 A patient with a cancerous tumor undergoes gene therapy. What is the goal of gene therapy in this patient? • Suppression of the immunologic response to cancer cells • Use of a systemic viral vector to eradicate the tumor • Enhanced antitumor response of the immune system Correct • Exogenous method of tumor destruction The general goal of gene therapy is to use exogenous gene material to induce a change in the response of the patient to endogenous genetic function in response to a given disease. The goal of gene therapy in this patient is to change the patient's immunologic response to the tumor by providing a new genetic code that will strengthen the patient's antitumor response capacity. Gene therapy is being used to enhance the immunologic response to the tumor through the use of the human immunologic system's antitumor activity. The use of a viral vector is one type of gene therapy. Exogenous methods of tumor destruction include chemotherapy and radiation therapy. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242223874 A patient undergoes gene therapy involving the use of a viral vector for the gene transfer process. What is one risk of gene therapy in this patient? • Development of viral disease Correct • Synthesis of disease-fighting proteins • Enhancement of killer T lymphocytes • Permanent change in protein synthesis One risk for the patient undergoing gene therapy involving the use of a viral vector is viral disease. This is a potentially life-threatening complication of gene therapy in a patient who is immunocompromised, because the patient's capacity to fight the viral disease is impaired. Successful gene therapy results in the synthesis of specific proteins that fight the disease. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242223888 A male African-American patient has refractory hypertension. Which genetic technique is most likely to help control the patient's blood pressure? • Selection of therapy on the basis of race Correct • Genotyping for sodium channels • Selection of therapy on the basis of sex • Genotyping for adrenergic receptors In race-based drug selection, the provider chooses medications that are more likely to be effective for a patient of a certain race. In this case, genetic variations in African-American subjects should prompt the provider to include isosorbide dinitrate with hydralazine (BiDil) in the therapy for hypertension. Genotyping for sodium channels helps refine the selection of antihypertensive agents associated with rennin-angiotensin receptors and adrenal gland receptors. The selection of drug therapy on the basis of a patient's sex is unlikely to help in this case because such determinations have not been established. Genotyping for beta-adrenergic receptors is used to determine which asthma patients are likely to benefit from beta-agonist therapy. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242223895 A 26-year-old female patient who takes ethinyl estradiol and norgestimate (Ortho Tri-Cyclen) has pulmonary emboli. The patient has consented to genetic testing to detect which gene? • HER2 • Factor V Correct • BRCA-1 • Mutated If a woman has the factor V gene, her risk for a thromboembolic event (e.g., a pulmonary embolus) when she takes an oral contraceptive is 7 to 100 times greater than that of a woman without the gene. HER2 is an oncogene, normally active in a fetus, used to identify patients with breast cancer who are suitable candidates for traztuzumab (Herceptin) therapy. BRCA-1 is a gene that increases the risk of breast cancer. The patient's genotype is not the result of a mutation. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-156l-d6kumpxi!reviewSubmittedAssessmentAttempt?attempt=17660395623> Ch. 10 1. 1.ID: 10242205096 What is the primary indication for the administration of morphine? • To diminish feelings of anxiety • To relieve acute and chronic pain Correct • To induce a state of unconsciousness • To increase cardiac filling pressures The principal indication for morphine is the relief of moderate to severe pain, including postoperative pain and cancer pain. In addition, morphine is used during acute myocardial infarction to relieve pain, anxiety, and dypsnea and to promote relaxation of vascular smooth muscle. Morphine may also be administered before surgery for sedation. Awarded 1.0 points out of 1.0 possible points. 2. 2.ID: 10242207800 The nurse prepares to administer morphine sulfate 5 mg IV to a patient who underwent surgery 30 minutes earlier. What is the most important reason for the nurse to record baseline vital signs before administering this drug? • Morphine sulfate causes release of histamine. • Morphine sulfate reduces the level of consciousness. • Morphine sulfate dilates vascular smooth muscle. • Morphine sulfate depresses the respiratory center. Correct Respiratory depression is the most important reason that the nurse records baseline vital signs before administering morphine IV: Opioid analgesics can cause respiratory depression and death when administered in standard dosages and in an overdose, respectively. Because this patient is in the immediate postoperative period and is likely to experience residual effects of anesthesia, including inability to maintain an airway and respiratory depression, the risk for respiratory depression is high. The patient is also at risk because the route of administration is IV. IV administration of an opioid means that the onset of action occurs quickly, the peak drug level occurs more quickly, and the risk of respiratory depression increases as a result of a generally high plasma drug level. The nurse records baseline data for comparison to vital signs taken 15 minutes after IV administration of morphine to determine whether the patient is experiencing adverse effects of therapy. Morphine dilates vascular smooth muscle, releases histamine, and causes sedation; however, airway and breathing issues are more important. Death following overdose is almost always a result of respiratory arrest. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242205090 The nurse administers oxycodone 5 mg with acetaminophen 500 mg (Percocet) to a patient for postoperative pain. Which patient teaching about the analgesic agent is the nurse's priority before the nurse leaves the patient's room? • The patient may chew ice chips to relieve dry mouth. • The patient should call for help before getting up. Correct • The patient should report any nausea or vomiting. • The patient may feel flushed or diaphoretic. The nurse instructs the patient to call for help before getting up because oxycodone is an opioid that can cause relaxation of vascular smooth muscle through the release of histamine, thereby blunting the baroreceptor reflex. Because the baroreceptors are less responsive, orthostatic hypotension may result from the pooling of blood in the dilated blood vessels as the system's compensatory mechanism for position changes is impaired. The available blood volume that the cardiovascular system can shunt to the brain when the patient stands is reduced; as a result, the blood pressure falls transiently when the patient stands, increasing the risk of falls and injury. Nausea, constipation, dry mouth, and flushing are common adverse effects of oxycodone; however, they are secondary in importance because the risk of patient injury is a more immediate and serious consequence of therapy. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242205094 The nurse prepares morphine sulfate IV for a patient but decides to consult with the pharmacist before administering the medication. Which condition is the most likely reason the nurse has decided to consult the pharmacist? • Cancer • Asthma Correct • Diarrhea • Anorexia Morphine should be used with caution in patients with asthma because naturally occurring opioids cause the release of histamine; a release of histamine in a patient with asthma can trigger bronchoconstriction. Because morphine is bound to protein 20% to 35%, the patient's cancer and anorexia are causes for concern because both conditions can result in hypoproteinemia and a lack of protein-binding sites for morphine and, therefore, altered pharmacokinetics of the medication. The administration of morphine can help diminish diarrhea. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242205086 A patient's admission vital signs are temperature 37.6° C, heart rate 96 beats/min, respirations 22 breaths/min, and blood pressure 140/90 mm Hg. Later, the patient requests pain medication, and the nurse records vital signs before administering codeine 15 mg with acetaminophen 300 mg (Tylenol 2) two tablets by mouth. Before administering the medication, which patient assessment is the nurse's priority? • Heart rate 110 • Respiratory rate 10 Correct • Temperature 38.0°Celsius • Blood pressure 160/86 mm Hg The priority patient assessment is the respiratory rate because it has decreased by more than 50%. Opioids can cause respiratory depression, and breathing is more important than circulation issues. To prevent respiratory failure, the nurse withholds the analgesic and plans follow-up nursing interventions. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242205098 For which type of pain is a fentanyl (Duragesic) transdermal patch best suited? • Pain after abdominal surgery • Acute treatment of a migraine headache • Lower back pain related to lumbar strain • Severe pain resulting from cancer metastasis Correct Transdermal fentanyl (Duragesic) is indicated only for persistent severe pain in patients who are already opioid tolerant because fentanyl can cause fatal respiratory depression in patients who are opioid naive. For this reason, the patch is not indicated for acute pain such as postoperative pain, intermittent pain, or pain that responds to a less powerful analgesic. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242205088 The patient has been taking morphine for postoperative pain. Before discharge, what patient teaching should be provided to prevent constipation? (Select all that apply.) • Increase fluid intake throughout the day Correct • Increase rest periods • Take a stool softener Correct • Decrease the medication dosage with constipation • Eat more animal protein and dairy Constipation may be managed with increased intake of fluids, use of stool softeners such as docusate sodium, or use of stimulants such as bisacodyl or senna. Agents such as lactulose, sorbitol, and polyethylene glycol (Miralax) have been proven effective. Less commonly used are bulk-forming laxatives such as psyllium, for which increased fluid intake is especially important to avoid fecal impactions or bowel obstructions. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242205092 The nurse in the postanesthesia care unit (PACU) notes that a patient has a respiratory rate of 6 breaths/min 30 minutes after surgery. Which action should the nurse implement next? • Check the timing of the last opioid Correct • Initiate resuscitative measures • Give flumazenil (Romazicon) • Prepare naloxone (Narcan) IV To complete the patient assessment for the planning of suitable nursing care, the PACU nurse checks the anesthesia record to determine the time and dosage of opioid analgesics and other anesthetics used in the operating room (OR). This is because many of the anesthetic agents used in the OR can induce respiratory depression. The patient's respiratory depression may be due to the residual effects of a muscle relaxant, an opioid (for which naloxone is the antidote), a benzodiazepine (for which flumazenil is the antidote), a barbiturate, or an anesthetic gas. The nurse needs to know which agent or agents are most likely causing the respiratory depression to complete the assessment. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-ndna-ocnumpxi!reviewSubmittedAssessmentAttempt?attempt=17679025490> Ch. 11 • The nurse conducts preoperative teaching with a patient who will undergo a laparotomy. Which statement should the nurse make to the patient to describe a suitable indication for the use of pancuronium during surgery? • "The medication will maintain a stable blood pressure." • "The medication will reduce upper respiratory secretions." • "The medication will keep your heartbeat slow and regular." • "The medication will relax your abdominal muscles for the surgery." Correct Pancuronium (Pavulon) is a neuromuscular-blocking agent that is used during surgery to relax muscles for exposure of the surgical site and for intubation and mechanical ventilation. Pancuronium acts by blocking the action of acetylcholine. The nurse avoids describing the muscle relaxation as paralysis, which could cause unnecessary fear in the patient. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242199512 A patient receives a nondepolarizing neuromuscular-blocking drug (NMBD) during surgery. This type of drug works by preventing the action potential in the motor neuron because it binds to the receptors in place of what? • Serotonin • Dopamine • Acetylcholine Correct • Norepinephrine A nondepolarizing NMBD acts like the neurotransmitter acetylcholine. It binds to the terminal of a motor neuron to prevent motor function. At first the muscles fasciculate, but after a period of depolarization they become unresponsive to acetylcholine and fail to depolarize. Succinylcholine is a nondepolarizing NMBD that is deactivated rapidly by cholinesterase, affording this drug a short duration of action. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242199520 Which are the first muscles to be paralyzed after the administration of pancuronium? (Select all that apply.) • Eyes Correct • Neck • Limbs • Fingers Correct • Diaphragm • Intercostals The first muscles affected by the action of pancuronium, a nondepolarizing neuromuscular-blocking drug, are the muscles of the eyes and fingers. Next are the muscles of the limbs, neck, and trunk. Finally, the intercostal muscles and the diaphragm are paralyzed temporarily. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242199518 The nurse anesthetist plans to administer vecuronium to a patient during surgery. Which laboratory finding indicates an increased risk of toxic effects from this medication? • Serum calcium 9 mg/dL • Serum sodium 140 mEq/L • Serum potassium 3.2 mEq/L Correct • Serum magnesium 1.5 mg/dL Hypokalemia increases a patient's risk of toxicity from vecuronium, a nondepolarizing neuromuscular-blocking drug, by prolonging the effects of the drug. This patient's calcium, sodium, and magnesium levels are within normal limits. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242199522 A patient receives succinylcholine during surgery. Which adverse effect of succinylcholine is the nurse's priority in the postoperative period? • Malignant hyperthermia Correct • Skeletal muscle pain • Serum potassium 4.8 mEq/L • Blood pressure 90/62 mm Hg Malignant hyperthermia is a rare and potentially fatal condition that can be triggered by succinylcholine, a depolarizing neuromuscular-blocking drug. Clinical indicators of malignant hyperthermia, including high temperature, tachycardia, and muscle rigidity, should trigger immediate treatment because the condition can be fatal. The patient's blood pressure is adequate, even though succinylcholine can cause alterations in blood pressure. Postoperative muscle pain is a common adverse effect of succinylcholine; however, the drug continues to be used because of its rapid onset and short duration of action. Succinylcholine promotes release of potassium but rarely causes severe hyperkalemia. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242199510 A patient about to undergo surgery states that a family member has a history of difficulty with surgery. Which subjective information about a family member contraindicates the use of succinylcholine in this patient? • Loop diuretic use • Essential hypertension • Malignant hyperthermia Correct • Decreased serum sodium Succinylcholine is contraindicated in patients with a personal or familial history of malignant hyperthermia or conditions that can lead to hyperkalemia, including denervation of skeletal muscle and upper motor neuron disease or a personal history of major burns or multiple trauma. None of the remaining family information represents a high risk in connection with the use of succinylcholine. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242199516 For a procedure that should last 30 minutes, which nondepolarizing neuromuscular-blocking agent (NMBD) is the best choice to prevent prolonged muscle relaxation? • Pancuronium (Pavulon) • Doxacurium (Nuromax) • Vecuronium (Norcuron) Correct • Succinylcholine (Anectine) Vecuronium is the best nondepolarizing NMBD because its duration of action is 25 to 40 minutes; only one injection of vecuronium should be required to complete the procedure. Pancuronium and doxacurium are not good choices because of their prolonged durations of action. Succinylcholine is not a good choice because it is a depolarizing NMBD. In addition, succinylcholine would require multiple injections to maintain muscle relaxation because its duration of action is just 4 to 6 minutes. Awarded 1.0 points out of 1.0 possible points Ch. 12 • 1.ID: 10242186353 A patient has received an excessive dose of baclofen (Lioresal). Which action does the nurse implement next? • Comfort measures • Seizure precautions • Airway maintenance Correct • Antidote preparation An overdose of baclofen can cause respiratory depression as a result of excessive central nervous system depression, so the nurse prepares to maintain the patient's airway and breathing with the use of an airway, oxygen, and a bag for ventilation. General supportive therapy, including cardiac monitoring, gastric lavage, and fluid therapy, is instituted to maintain vital functions until the depressant effects of baclofen wear off. An antidote to baclofen does not exist. Although comfort measures are usually appropriate, the nurse's priority is the maintenance of vital functions. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242186345 Which drug is the only muscle relaxant that acts directly on skeletal muscle? • Baclofen (Lioresal) • Diazepam (Valium) • Dantrolene (Dantrium) Correct • Cyclobenzaprine (Flexeril) Dantrolene works directly on skeletal muscle by suppressing the release of calcium from the sarcoplasmic reticulum to ease contractions. The remaining medications are centrally acting muscle relaxants that work by means of central nervous system depression. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242186357 Dantrolene (Dantrium) acts on the sarcoplasmic reticulum in the treatment of malignant hyperthermia by blocking the release of what? • Sodium • Glucose • Calcium Correct • Potassium The heat in malignant hyperthermia results from the contraction of muscles, the product of a massive release of calcium from the sarcoplasmic reticulum. By acting at the sarcoplasmic reticulum to block the release of calcium, dantrolene relaxes skeletal muscle and helps reduce the patient's temperature. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242186341 A patient has been prescribed eszopiclone (Lunesta), and the nurse provides patient teaching so the patient may take the medication safely. Which instruction should the nurse include in patient teaching? • Allow at least 8 hours for sleep. Correct • Take the medication with food or milk. • Expect and prepare for a daytime hangover. • Report palpitations to the prescribing provider. The nurse instructs the patient to take eszopiclone only when 8 hours can be allotted for sleep because the drug induces sleep lasting 8 hours. A patient who takes eszopiclone and gets up before 8 hours have passed is at risk for lethargy and for injury while driving a car, navigating stairs, or performing other activities. The nurse may recommend that the patient take eszopiclone with food, which may mask the unpleasant taste associated with the drug. Palpitations and hangover are uncommon adverse effects of eszopiclone. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242186355 The nurse prepares to administer cyclobenzaprine (Flexeril) to a patient who has been in a motor vehicle accident (MVA). Which piece of preadministration assessment data is the nurse's priority in the evaluation of adverse effects of therapy? • Amount of bleeding • Indicators of infection • Spasms of the muscles • Level of consciousness Correct The nurse compares the patient's level of consciousness after the administration of cyclobenzaprine to the findings of the preadministration neurologic assessment to evaluate the adverse effects of the drug, which can cause significant sedation. However, because the patient was in an MVA, a significant reduction in the level of consciousness or unresponsiveness in the patient warrants further investigation by the nurse to rule out increased intracranial pressure. The nurse assesses muscle spasms to evaluate the effectiveness of therapy, as less muscle spasticity is expected after the administration of cyclobenzaprine. Cyclobenzaprine should have no effect on infection; as long as the spastic muscles are not bleeding, it should have no direct effect on bleeding. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242186351 A patient asks the nurse whether she may take diazepam (Valium) to help her sleep at night. Which information should the nurse include in patient teaching to help prevent adverse effects of diazepam? • Avoid using this drug to induce sleep. Correct • Use the lowest effective dosage. • Take the drug 30 minutes before sleeping. • Drink coffee or tea in the morning. Diazepam, a benzodiazepine, is a poor choice for a hypnotic because it can cause a morning hangover, is addictive with long-term use, and can cause rebound insomnia with abrupt withdrawal. For these reasons, the nurse instructs the patient to avoid using diazepam for the purpose of inducing sleep. Some benzodiazepines are hypnotics, but these agents have been replaced on the market by newer nonbenzodiazepine hypnotic agents. The nurse avoids instructing the patient to use the lowest effective dosage; these instructions are beyond the nurse's scope of practice. Drinking coffee or tea in the morning can help combat a hangover, but because diazepam is a poor choice of hypnotic, the nurse avoids instructing the patient to do this or to take the drug 30 minutes before sleep is desired. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242186343 Which benzodiazepine has rapid onset, is short acting, and is used to relieve anxiety and provide sedation before and during procedures? • Diazepam (Valium) • Midazolam (Versed) Correct • Tamazepam (Restoril) • Flurazepam (Dalmane) Midazolam is used in the perioperative period to relieve anxiety, provide sedation, and help induce general anesthesia. Its rapid onset and brief duration of action provide the nurse with a higher degree of control over the effects of the drug. Diazepam is an old benzodiazepine used to relieve anxiety, induce muscle relaxation, and control seizure activity. Tamazepam and flurazepam, also older benzodiazepines, are indicated for insomnia; both have been supplanted by newer drugs. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242186349 Which nonbenzodiazepine hypnotic agents are recommended for the relief of nighttime awakening? (Select all that apply.) • Zaleplon (Sonata) Correct • Zolpidem (Ambien) • Carisoprodol (Soma) • Ramelteon (Rozerem) Correct • Eszopiclone (Lunesta) • Zolpidem (Ambien CR) Zaleplon and ramelteon are recommended for patients who awaken during the night because of their short durations of action. Zolpidem (Ambien and Ambien CR) and eszopiclone have longer durations of action and are therefore unsuitable as hypnotics when less than 8 hours of sleep is desired. Ambien CR is a dual-release formulation of zolpidem. Carisoprodol is a muscle relaxant. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242186347 Which characteristics are shared by diazepam (Valium) and phenobarbital (Luminal)? (Select all that apply.) • Potential for hangover Correct • Induction of anesthesia • Potential for abuse Correct • Use for seizure control Correct • Deprivation of rapid eye movement (REM) sleep • Relief of muscle spasticity Both benzodiazepines (diazepam) and barbiturates (phenobarbital) are sedative-hypnotic agents, have the potential to cause a hangover from therapy, and are effective in seizure control; however, these medications also carry a high risk of addiction and abuse. Neither medication is used to induce general anesthesia. Barbiturates deprive patients of REM sleep; benzodiazepines do so to a lesser extent. Barbiturates are not used to relieve muscle spasms, but diazepam is effective in this regard. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-8jlu-aonumpxi!reviewSubmittedAssessmentAttempt?attempt=17679831009> Ch. 13 • 1.ID: 10242254304 What is the mechanism of action for an amphetamine? • Promotes the release of norepinephrine Correct • Binds directly with adrenergic receptors • Promotes the reuptake of norepinephrine • Acts as a norepinephrine receptor antagonist Noradrenergic agonists, such as amphetamines, are sympathomimetic agents that act on terminals of sympathetic nerves to promote the release of norepinephrine and inhibit its reuptake. Because contact between norepinephrine and its receptors is maintained for a longer period, the effects of norepinephrine—including euphoria, capacity for work, and mental alertness resulting from stimulation of the cerebral cortex and thalamus—are prolonged. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242254320 Which drugs are indicated as abortive therapy for migraine headaches? (Select all that apply.) • Diazepam (Valium) • Zolmitriptan (Zomig) Correct • Naratriptan (Amerge) Correct • Ergotamine (Ergostat) • Sibutramine (Meridia) • Atomoxetine (Strattera) Selective serotonin receptor agonists (SSRAs) are the medications most commonly used as abortive therapy for migraine headaches. The SSRAs include the triptans zolmitriptan and naratriptan. Ergot alkaloids such as ergotamine are rarely used as abortive therapy. Diazepam, a benzodiazepine, is used to ease anxiety, induce muscle relaxation, and relieve seizures; sibutramine is an anorexiant; and atomoxetine is used for ADHD. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242254310 The nurse is teaching a 10-year-old patient and the patient's parents about drug holidays. What statement by the patient indicates that more education is needed? • "I can skip taking my medication on the weekend." • "During a week-long drug holiday I should skip my meds 1 day a week." • "I should maintain my regular activities." • "I should avoid chocolate while on a drug holiday." Correct Specialists sometimes recommend periodic "drug holidays" (e.g., 1 day per week) without medication to diminish the addictive tendencies of the stimulant drugs. School-aged children often do not take these drugs on weekends and school vacations. No other changes to an individual's routine are required. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242254314 A patient receives a prescription for sumatriptan (Imitrex). Which information in the patient's history is a contraindication to the use of this drug? • Type 2 diabetes mellitus • Coronary artery disease Correct • Obstructive lung disease • Gastroesophageal reflux Sumatriptan is generally well tolerated, and most side effects are transient and mild. However, because it can cause coronary vasospasm, sumatriptan is contraindicated in patients with a history of ischemic heart disease, myocardial infarction, uncontrolled hypertension, or other cardiovascular disease. The nurse assesses patients with diabetes mellitus extra carefully before administering sumatriptan because these patients are at high risk for cardiovascular disease. Patients with obstructive lung disease or gastroesophageal reflux should be able to take sumatriptan. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242254316 Which characteristic of amphetamines is the most likely reason that these drugs are abused? • They induce euphoria. Correct • They increase energy. • They induce wakefulness. • They promote industriousness. The effect of amphetamines that makes them targets for abuse is euphoria, which includes a sense of joy, elation, and excitement. Amphetamines can also increase an individual's energy level, degree and duration of wakefulness, and capacity for work; they are used for all of these purposes. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242254302 How does caffeine work to ease neonatal apnea? (Select all that apply.) • Promotes constriction of the bronchi • Relaxes the bronchial smooth muscle Correct • Increases the production of surfactant • Increases sensitivity to carbon dioxide Correct • Supports a regular pattern of breathing Correct • Blocks the action of cerebral adenosine Correct By inhibiting phosphodiesterase, caffeine relaxes bronchial smooth muscle, promotes a regular pattern of breathing by decreasing the work of breathing, and blocks the action of adenosine to stimulate the area of the brain that senses carbon dioxide. Caffeine neither increases surfactant production nor constricts the vessels in the bronchi. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242254306 In which individual(s) is the use of analeptics contraindicated? (Select all that apply.) • An individual with hypertension Correct • An individual with peptic ulcer disease Correct • An individual taking oral contraceptives • An individual taking sildenafil Correct • An individual with hypotension Contraindications to the use of analeptics include drug allergy, peptic ulcer disease (especially for caffeine), and serious cardiovascular conditions. Concurrent use of other phosphodiesterase-inhibiting drugs such as sildenafil and similar drugs is also not recommended. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242254300 A 6-year-old boy is being evaluated for attention deficit–hyperactivity disorder (ADHD). Which characteristics must be identified in the child's behavior before central nervous system stimulants are indicated? (Select all that apply.) • Short attention span for his age Correct • Acting out during school or in the home • Lack of ability to control impulses Correct • Learning disability and depression • Symptoms lasting at least 6 months Correct • Onset after the age 7 years Clinical indicators of ADHD that must be present for at least 6 months and in two different settings include a short attention span for the child's age. ADHD usually begins before age 7 years. Learning disabilities, mental illness, and familial tendencies are commonly associated with ADHD, but the diagnosis does not depend on the presence of these factors. Stimulants are the primary pharmacotherapy for ADHD. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242254312 A patient taking orlistat (Xenical) reports that he is losing weight slowly but says that he wants to discontinue taking the drug because of the adverse effects. What instruction should the nurse include in patient teaching to make it easier for the patient to continue taking the drug? • Request an antidiarrheal agent. • Decrease intake of dietary fats. Correct • Increase intake of dietary fiber. • Take vitamins A, D, and E daily. By reducing the daily dietary intake of fat to 30% or less, the patient may be able to minimize the risk of adverse effects of orlistat therapy, which include oily fecal spotting, flatulence, and uncontrollable fecal incontinence. These adverse effects occur because orlistat reduces fat absorption in the intestines, leaving more fat in the intestines for elimination. If the patient consumes less fat, there is less fat left in the intestines for elimination. Antidiarrheal agents are ineffective therapy for these adverse effects because they reduce intestinal motility and do nothing to alter the fat content of stool. Increased fiber intake is usually a suitable recommendation; however, evidence supporting its use to decrease the adverse effects of orlistat is lacking. Fat-soluble vitamin supplements are recommended to replenish concentrations of vitamins lost as a result of the drug's effect. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242254318 A college student tells the nurse that she uses guarana to help her study at least one night a week. Which subjective information should the nurse ask the student about as a means of helping prevent unwanted drug interactions? (Select all that apply.) • Use of oral contraceptives Correct • Seasonal allergies • Use of sympathomimetics Correct • Use of tobacco products Correct • Currency of immunizations • Weight loss over the past year The nurse gathers data about the student's history to help prevent unwanted drug interactions because guarana interacts with several medications to increase, decrease, or alter the effects of those medications. Guarana can alter the effectiveness of oral contraceptives, increasing the likelihood of an unplanned pregnancy. Because guarana is a central nervous system (CNS) stimulant, taking it with other CNS stimulants can lead to toxic effects such as severe hypertension and convulsions. Sympathomimetic agents, phenylephrine, and nicotine are all CNS stimulants. Seasonal allergies could be important if the student takes phenylephrine to clear nasal passages, but her immunization history is probably not a matter for concern. Guarana can cause weight loss and inadequate nutrition by suppressing appetite; however, appetite suppression is not related to drug interactions. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242254308 Which CNS stimulant is not addictive? • Ergotamine (Ergostat) • Sumatriptan (Imitrex) • Phentermine (Ionamin) • Atomoxetine (Strattera) Correct Atomoxetine, a norepinephrine reuptake inhibitor, is a newer agent approved for use in ADHD; its advantage over amphetamines and phenidates is that is not addictive. Sumatriptan was released before ergotamine and phentermine but after atomoxetine. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-6y0e-nunumpxi!reviewSubmittedAssessmentAttempt?attempt=17683849156> Ch. 14 • 1.ID: 10242264722 The nurse finds a patient on the floor who is unresponsive but exhibiting spasms of the trunk and flexion of the arm alternating with periods of relaxation. Which finding should the nurse include in the nursing documentation? • Patient on floor as a result of loss of consciousness • Patient fallen to floor, exhibiting tonic convulsions • Patient exhibiting arm flexion with trunk spasms Correct • Patient fallen to floor as a result of tonic-clonic seizure The nurse documents an objective description of the event by stating that the patient is exhibiting arm flexion and trunk spasms and, therefore, that the patient is experiencing a type of generalized seizure involving tonic-clonic convulsive activity. The nurse does not know how the patient got to the floor; however, the facts that the patient was found on the floor and is unresponsive should be documented. The nurse avoids documenting that the patient fell, fell because of the convulsions, or first lost consciousness, because the nurse did not witness the sequence of events. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242264708 The patient is receiving intravenous (IV) antiepileptic therapy. Which parenteral antiepileptic drug is effective against all types of generalized seizures? • Phenytoin • Fosphenytoin • Phenobarbital • Valproic acid Correct Valproic acid is indicated in all forms for generalized seizures, including tonic-clonic, absence, and myoclonic seizures. Phenytoin, fosphenytoin, and phenobarbital are parenteral antiepileptic medications, effective in the treatment of partial seizures and, secondarily, generalized tonic-clonic seizures. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242264716 What is the best diagnostic study with which to determine the type of seizure activity while the patient is experiencing the seizure? • Electroencephalogram (EEG) Correct • Computed tomography (CT) • Magnetic resonance imaging (MRI) • Positron emission tomography (PET) The EEG is the best diagnostic study with which to determine the type of seizure a patient is having while experiencing the seizure because an EEG detects electrical discharges in the brain and records them as waves on a tracing. Electrical activity associated with seizures is excessive and disorganized, but the waves are correlated with different neurologic conditions. CT, MRI, and PET do not detect electrical activity in the brain. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242264724 The nurse needs to administer phenytoin (Dilantin) 300 mg IV bolus to a patient. At a minimum, over how many minutes should the nurse administer this dose? • 3 minutes • 5 minutes • 6 minutes Correct • 10 minutes The nurse administers IV phenytoin no faster than 50 mg/min to reduce the risk of cardiovascular collapse. Calculation: (1 min/50 mg) × 300 mg = 300 ÷ 50 = 6 minutes. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242264712 The nurse prepares to administer carbamazepine to a patient. Which liquid should be avoided when taking this medication? • Orange juice • Apple juice • Grapefruit juice Correct • Milk Carbamazepine is not to be given with grapefruit or grapefruit juice because this leads to increased toxicity of the antiepileptic drug. The other liquids do not cause an increased level of the antiepileptic drug and may be used when administering this medication. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242264706 A patient who needs an antiepileptic medication for tonic-clonic seizures is unresponsive. Which antiepileptic medication(s) should the nurse avoid administering to this patient? (Select all that apply.) • Tiagabine Correct • Phenytoin • Topiramate Correct • Gabapentin Correct • Ethosuximide Correct • Phenobarbital Because the patient is unresponsive, the nurse avoids administering medications by mouth; doing so exposes the patient to an increased risk of aspiration. Until the level of consciousness improves and the patient can swallow, the nurse should not administer tiagabine, topiramate, gabapentin, or ethosuximide, which are available for oral administration only. In addition, tiagabine, gabapentin, and ethosuximide are not indicated therapy for tonic-clonic seizures. Topiramate, phenytoin, and phenobarbital are suitable for tonic-clonic seizures, but only phenytoin and phenobarbital, which may be administered IV, are indicated for an unresponsive patient. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242264710 The nurse prepares for discharge a female patient who has been started on phenobarbital and also takes an oral contraceptive. Which intervention is the nurse's highest priority before discharge? • Planning for regular exercise in a safe setting • Making a medication reminder sign for the home • Instructing the patient to get help before climbing stairs Correct • Helping the patient plan another form of birth control Because phenobarbital can cause lethargy, drowsiness, and dizziness, the nurse instructs the patient to get help when climbing stairs to help prevent injury. The nurse instructs the patient to continue precautions to maintain safety until the full effects of the drug are known. Of secondary importance, the nurse instructs the patient to use an alternative form of birth control because the effect of the oral contraceptive is blunted with concomitant administration of phenobarbital. The nurse instructs the patient to plan exercise because the lethargy from this medication can contribute to deconditioning. The nurse also instructs the patient to post a sign as a reminder to take phenobarbital once a day to maintain adherence to therapy. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242264718 A patient receives phenytoin for partial seizures. Which medication requires a higher-than-normal dosage when taken by the patient during this therapy? • Tiagabine • Lamotrigine Correct • Gabapentin • Phenobarbital A normal dosage of lamotrigine is unlikely to be effective against partial seizures when administered with phenytoin because these medications are metabolized by the same hepatic enzymes, resulting in decreased effectiveness of the lamotrigine. For the lamotrigine to be therapeutically effective, the dosage must be increased when the drug is administered concurrently with phenytoin. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242264720 A patient's pharmacotherapy includes valproic acid, and the prescriber wants to add carbamazepine. After the new medication is added, which phenomenon is the nurse most likely to observe in the patient? • Less amnesia after a convulsion • Increased number of convulsions Correct • Changes in nature of convulsions • Improved level of consciousness Administration of carbamazepine with valproic acid is likely to decrease the effectiveness of valproic acid; therefore, the patient is more likely to experience more convulsions because carbamazepine increases the metabolism of valproic acid. Because patients are more likely to experience additional adverse drug effects with combination therapy, the patient is unlikely to experience less amnesia, which can be caused by a seizure. For the same reason, the patient is likely to be more lethargic. Antiepileptic medications should not alter the characteristics of the convulsions. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242264714 What information should the nurse provide to a patient who will self-administer an antiepileptic agent for the first time at home? • Report any vision or hearing problems with levetiracetam. • Stir phenobarbital elixir into a cold carbonated beverage. • Have a complete blood count monthly while taking carbamazepine. Correct • Administer pregabalin in one morning dose on an empty stomach. The nurse instructs the patient taking carbamazepine to have complete blood counts as directed, usually every month at first, because iminostilbenes can cause bone marrow suppression. Patients taking levetiracetam are told to report changes in mood or behavior or motor difficulties. Patients taking phenobarbital are instructed to mix the elixir with fruit juice, milk, or water but not a carbonated beverage. The nurse instructs the patient taking pregabalin to take the medication in two or three doses and to avoid sudden withdrawal of the medication. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-8fh7-a1oumpxi!reviewSubmittedAssessmentAttempt?attempt=17683887551> Ch.15 • 1.ID: 10242217169 A lack of which substance, resulting in an imbalance between it and acetylcholine, is the basic origin of Parkinson's disease? • Serotonin • Dopamine Correct • Epinephrine • Norepinephrine The underlying cause of Parkinson's disease is loss of dopaminergic neurons in the substantia nigra, resulting in a deficiency of dopamine and an imbalance between dopamine and acetylcholine. Because dopamine is an inhibitory neurotransmitter and acetylcholine is an excitatory neurotransmitter, the imbalance results in the effects of acetylcholine dominating the patient's motor activity. These pathologic features include akinesia, bradykinesia, postural instability, rigidity, and tremors. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242217171 A female patient receives a diagnosis of Parkinson's disease. Which treatment for the disease should the nurse implement first? • Encouraging physical activity • Instituting pharmacotherapy • Teaching about assistive devices • Explaining the disease's characteristics Correct When Parkinson's disease is diagnosed, the nurse provides patient and family teaching about the disease, including its pathophysiology and treatment options, to help them learn to manage this chronic, progressive neurodegenerative disorder. After patient teaching, the patient and family are better equipped to understand the disease's progression, the related pharmacotherapy, the need for physical activity, and the role of assistive devices. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242217165 A male patient with Parkinson's disease takes carbidopa-levodopa (Sinemet) but experiences disabling tremors. Which adjunct medications are suitable therapies for alleviation of the patient's tremors? (Select all that apply.) • Trihexyphenidyl Correct • Ropinirole (Requip) • Selegiline (Eldepryl) • Benztropine (Cogentin) Correct • Pramipexole (Mirapex) • Amantadine (Symmetrel) To help diminish the patient's tremors, the nurse plans to administer an anticholinergic agent to oppose the effects of acetylcholine; these agents include trihexyphenidyl and benztropine (Cogentin). This is necessary because the tremors and other abnormal movements associated with Parkinson's disease are the result of an imbalance between acetylcholine and dopamine wherein the dopamine is deficient. Ropinirole and pramipexole are nonergot dopaminergic agents used to activate production of more dopamine. Selegiline is a monoamine oxidase B inhibitor used in combination with carbidopa-levodopa to inhibit the breakdown of dopamine and reduce the dosage of levodopa needed. Amantadine is the only presynaptic dopamine release enhancer used to increase the release of dopamine from terminal vesicles. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242217179 Why is levodopa the mainstay of treatment for a patient with Parkinson's disease? • It enhances dopamine release. • It promotes dopamine synthesis. • It impairs dopamine breakdown. • It provides a dopamine precursor. Correct Levodopa is a biologic precursor of dopamine that must be combined with carbidopa so that the brain can use it to synthesize dopamine; it is the only agent that acts in this manner. Other dopaminergic agents increase the brain's dopamine by stimulating its release, directly and indirectly; stimulating its synthesis; and inhibiting enzymes that degrade it. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242217161 What happens in the progression of Parkinson's disease that necessitates the use of different medications at different stages of the disease? • Buildup of plaque and beta-amyloid deposits • Loss of the myelin sheath along motor nerves • Progressive destruction of acetylcholine receptors • Destruction of the dopamine-producing vesicles Correct Parkinson's disease is characterized by the progressive destruction of dopamine-producing vesicles, which leads to an imbalance between acetylcholine and dopamine. The deficiency in dopamine production allows the effects of acetylcholine to predominate and thus promote the abnormal motor activity associated with Parkinson's disease, including dyskinesias and tremors. Plaques and amyloid deposits are characteristic of Alzheimer's disease; loss of the myelin sheath is characteristic of multiple sclerosis; and destruction of acetylcholine receptors is characteristic of myasthenia gravis. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242217167 The patient is taking an anticholinergic medication along with an antiparkinson medication. Which statement by the patient indicates more teaching is required? • "If it makes me nauseated I can take the medication with crackers." • "I can take this medication at bedtime as it makes me sleepy." • "No matter what, I cannot take this medication with food." Correct • "I can use hard candy to decrease any mouth dryness." With anticholinergic drugs, patients need to take the medication as prescribed, after meals or at bedtime and not at the same time as other medications. Because of the risk of stomach upset (nausea, vomiting), it is recommended that these drugs be taken with a snack, such as ginger ale and crackers. These medications are generally taken at night because of their sedating properties. Measures to help prevent and treat dry mouth are encouraged, such as increasing fluids and sucking on sugar-free hard candies. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242217181 Which medication is contraindicated in a patient receiving selegiline (Eldepryl) for Parkinson's disease? • Lisinopril (Zestril) • Ranitidine (Zantac) • Meperidine (Demerol) Correct • Aspirin (Bayer Aspirin) Concomitant administration of a monoamine oxidase-B inhibitor such as selegiline with meperidine (Demerol) is contraindicated because it can cause serotonin syndrome as a result of enhanced serotonin activity in the brain. Administration of lisinopril, ranitidine, or aspirin is not contraindicated. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242217175 The patient is taking bromocriptine. Which medication, if prescribed, should be questioned by the nurse? • Erythromycin Correct • Tramadol • Carbamazepine • Maalox Erythromycin should not be given with bromocriptine as both use the cytochrome P-450 pathway. This competition leads to increased bromocriptine effects with risk of toxicity. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242217163 A patient with Parkinson's disease needs an anticholinergic agent to help relieve dyskinesias. Which organ systems are priority nursing assessments before the administration of an anticholinergic agent to this patient? (Select all that apply.) • Auditory • Endocrine • Respiratory • Genitourinary Correct • Cardiovascular Correct • Gastrointestinal Correct The genitourinary, cardiovascular, and gastrointestinal systems are the nurse's priority assessments before the administration of an anticholinergic medication to a patient with Parkinson's disease because these are the systems affected most by the disease and because these systems are often affected by anticholinergic medications. Related adverse effects of anticholinergic agents include palpitations, urine retention, and constipation. The auditory, endocrine, and respiratory systems are rarely affected by the disease or therapy. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242217173 The nursing diagnosis for a patient is imbalanced nutrition, less than body requirements, related to the progress of Parkinson's disease and the adverse effects of pharmacotherapy. What is the best nursing intervention to include in the plan of care? • Offering cheese and crackers as snacks • Offering whole grains and vegetables Correct • Offering cereals fortified with vitamin B6 • Offering regular coffee or tea in the morning The nurse provides the patient with Parkinson's disease with nutrient-dense foods containing fiber, including vegetables and whole-grain breads and cereals, as part of a balanced diet. These foods have two benefits. First, nutrient-dense foods are more nutritious than other foods and help maintain the patient's nutritional status more efficiently as the disease progresses and the risks for inability to self-feed and swallow increase. Second, the dietary fiber these foods provide is important because patients with Parkinson's disease often complain of constipation. The nurse avoids offering cheese containing tyramine or caffeine to the patient as a way to reduce the risk of adverse effects of therapy. Although fortified cereals are more nutrient dense than nonfortified cereals, they are not as nutritious as whole grains and vegetables. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242217177 The patient is prescribed entacapone. What information should be included in a teaching plan? (Select all that apply.) • This medication may darken your urine, but it is a harmless side effect. Correct • This medication should be taken with meals to decrease GI upset. Correct • You must monitor your blood pressure once a week. • Report any back pain or jaundice as this may indicate liver dysfunction. Correct • You should not take this medication with any food or drink. Inform the patient that urine color may darken if taking entacapone and that this adverse effect is harmless. COMT inhibitors, entacapone and tolcapone, need to be taken with food to minimize GI upset. Other instructions include the reporting of any signs and symptoms of possible liver dysfunction, such as jaundice and back or abdominal pain, with the use of entacapone. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-6zje-j8oumpxi!reviewSubmittedAssessmentAttempt?attempt=17683897304> Ch.16 • 1.ID: 10242221442 Which phenomena does the nurse recognize as positive symptoms of schizophrenia? (Select all that apply.) • Hallucinations Correct • Muscle rigidity • Restless activity • Chaotic thinking Correct • Defective insight Correct • Social withdrawal Positive symptoms of schizophrenia include psychotic behaviors such as hallucinations. They also include conceptual disorganization such as chaotic thinking and poor insight. Negative symptoms include social withdrawal and catatonia characterized by agitation and muscle rigidity. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242221457 A patient with schizophrenia does not adhere to the pharmacotherapy regimen. Which potential cause of nonadherence is the nurse's priority because it is the most difficult to improve? • High incidence of adverse side effects • Inability to realize the need for therapy Correct • Need for multiple doses every 24 hours • Lack of money to pay for medication The nurse's priority is the promotion of continued pharmacotherapy. Because a cure does not exist, a patient with schizophrenia is likely to have altered thought processes that impair his or her ability to recognize the need for therapy. Effective treatment can make the patient believe that the disease has been cured and that there is no further need for the medication. Adverse side effects, multiple doses, and financial issues are problems that often have effective solutions. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242221465 What is the main receptor in the central nervous sytem (CNS) to be blocked by conventional antipsychotic drugs? • Serotonin • Dopamine Correct • Acetylcholine • Norepinephrine Conventional antipsychotic agents block dopamine receptors, primarily in the CNS. The blockade of dopamine receptors is responsible for the therapeutic and toxic effects of these medications. Atypical antipsychotic agents block dopamine-2 receptors and serotonin receptors, offering improved therapeutic effectiveness and a more favorable side effect profile. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242223853 A male patient asks the nurse how long it will take for escitalopram (Lexapro) to be completely effective for him. Which time frame should the nurse include in patient teaching? • 1 week • 2 or 3 days • 2 or 3 months • Several weeks Correct The nurse instructs the patient to adhere to therapy for several weeks to determine whether escitalopram will be an effective antidepressant for him. Escitalopram is a selective serotonin reuptake inhibitor (SSRIs), and a delay in therapeutic effectiveness is characteristic of SSRIs. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242223802 A patient receives a prescription for quetiapine (Seroquel). Which instruction should the nurse include in patient teaching about self-administration of this medication? • Report abnormal movements. Correct • Take the medication as needed for agitation. • Avoid cheese and cured meats. • Stop taking the medication if dizziness occurs. The nurse instructs the patient to report abnormal movements, which may indicate serious adverse effects of antipsychotic medications, including neuroleptic malignant syndrome, extrapyramidal symptoms, and tardive dyskinesia. Atypical antipsychotic agents are rarely prescribed on an as-needed basis; besides, a patient in a psychotic state is the least likely person to recognize the need for treatment. Patients taking atypical antipsychotic agents such as quetiapine do not need to avoid foods containing tyramine. Dizziness is a common adverse effect of therapy; rather than tell the patient to stop taking the medication, the nurse instructs the patient to report dizziness. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242223822 What is the most important benefit of taking a parenteral formulation of an antipsychotic medication? • Fewer doses needed for effective therapy • Increased likelihood of adherence to therapy Correct • Better chance of effectiveness • Can be injected as a long-acting agent The primary benefit of administering an injectable form of an antipsychotic agent is that patient adherence to therapy improves because fewer doses are required to achieve therapeutic effectiveness. Parenteral antipsychotic agents are long-acting medications. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242221411 Which piece of objective data is contraindication to the use of clozapine (Clozaril)? • Allergy to phenothiazines • Self-destructive behaviors • Failed antipsychotic therapy • Acute lymphocytic leukemia Correct Clozapine is contraindicated in patients with a history of myeloproliferative disorders such as leukemia because this medication can cause fatal agranulocytosis. For this reason, weekly monitoring of the white blood cell (WBC) count is mandatory. If the total WBC count falls below 3000/mm3, treatment should be interrupted. Clozapine is indicated for patients with a high risk for suicide and failed antipsychotic therapy involving the use of other medications. Because clozapine is not a phenothiazine, an allergy to those medications poses no obstacle to its use. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242221415 A patient taking risperidone (Risperdal) has a necrotic foot ulcer that started as a minor scratch. Which patient data should the nurse check to help prevent complications of the pharmacotherapy? • Leukocyte count • Liver function studies • Fasting blood glucose Correct • Kidney function studies Atypical antipsychotics can cause diabetes mellitus because they tend to impair glucose metabolism. Therefore, the nurse checks the fasting blood glucose level in a patient who presents with a deteriorating wound because diabetes impairs wound healing. This patient's glucose is likely to be poorly controlled as a result of the psychosis and the risperidone. Monitoring of liver and kidney function parameters is a reasonable strategy when patients are taking medication; however, the poorly healing ulcer, a common complication of diabetes, and the risperidone therapy indicate the need to check the blood sugar. A WBC count is a reasonable choice of test to determine the presence of infection but would not be needed if the ulcer were not present. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242221417 A patient who is taking an atypical antipsychotic agent for schizophrenia presents with a poorly healing leg ulcer and hyperglycemia. Which atypical antipsychotic agent is the best medication for the nurse to administer? • Olanzapine (Zyprexa) • Quetiapine (Seroquel) • Ziprasidone (Geodon) Correct • Risperidone (Risperdal) The best atypical antipsychotic agent for the nurse to administer in this case is ziprasidone, which has the least significant impact on patient weight and therefore on glucose metabolism. Olanzapine carries one of the highest risks for diabetes among the atypical antipsychotic agents. Quetiapine and risperidone affect patient weight more than ziprasidone does but less than olanzapine does. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242221429 The nurse administers amitriptyline hydrochloride to a patient with chronic depression. For which potential effects of the medication should the nurse monitor the patient? (Select all that apply.) • Constipation Correct • Hypotension Correct • Hyperpyrexia • Hyperglycemia • Improved sleep Correct • Urine retention Correct Amitriptyline is a tricyclic antidepressant that can induce such anticholinergic effects as constipation and urine retention. It can also cause dopaminergic- and adrenergic-blocker effects such as hypotension. Histamine blockade generally causes sedation and improves sleep. Tricyclic antidepressants should not cause hyperpyrexia or hyperglycemia. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242223838 The nurse prepares a patient who is taking sertraline (Zoloft) for discharge. Which instruction should the nurse include in patient teaching? • Take sertraline at same time each day. Correct • Expect to feel better in 4 to 6 days. • Avoid overheating and direct sun. • Report any increase in mania. Sertraline is a selective serotonin reuptake inhibitor, and the patient is most likely to experience therapeutic effectiveness if the medication is taken at the same time every day. The nurse instructs the patient to adhere to therapy for 4 to 6 weeks to determine the medication's effectiveness. Hyperpyrexia is an adverse effect of antipsychotic agents; lithium is used to treat bipolar disorder, of which mania is a characteristic. Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242221407 Which benefits are desired effects of instructing a patient with depression to take the daily dose of clomipramine (Anafranil) at bedtime? (Select all that apply.) • Helps the patient adhere to therapy Correct • Promotes sleep through significant sedation Correct • Reduces the rate of drug interactions • Eases anticholinergic effects • Diminishes sexual side effects • Reduces the risk of dysrhythmias The advantages of taking a tricyclic antidepressant (TCA) at bedtime are twofold: (1) It is easier for the patient to remember to take the medication, facilitating adherence and (2) it promotes sleep by causing maximal sedation at night. Bedtime administration should not improve the adverse effect profile of a TCA and therefore does not reduce the potential for drug interactions, anticholinergic effects, sexual side effects, or dysrhythmias. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242221419 A male patient tells the nurse that he wants to stop taking citalopram (Celexa) because of the sexual side effects. Which instruction should the nurse provide in patient teaching to help relieve the patient's sexual dysfunction? (Select all that apply.) • Discontinue the medication. • Take infrequent "drug holidays." Correct • Decrease the regular dosage. Correct • Report complaints to the psychiatrist. Correct • Maintain the current pharmacotherapy. Correct • Avoid alcoholic beverages. Correct Sexual dysfunction is managed in several ways, including reduction in the regular dosage, "drug holidays," addition of a medication for erectile dysfunction, change of antidepressant, and avoidance of alcohol. The nurse encourages the patient to continue taking an SSRI such as citalopram because the adverse effects of therapy often diminish in intensity and frequency over time; this strategy helps prevent disruptions in therapy. After providing this information the nurse encourages the patient to voice complaints to the psychiatrist who prescribes the antidepressant, but the nurse does not depend on the patient to ensure that the psychiatrist is notified of the complaint. The nurse avoids instructing the patient to discontinue therapy or to alter the dosage because these actions are not within the scope of nursing practice. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242223809 A male patient taking a monoamine oxidase inhibitor (MAOI) calls the nurse and reports headaches, tachycardia, nausea, and vomiting. Which patient teaching should the nurse implement? • Tell the patient to start drinking water. • Instruct the patient to lie down and rest. • Ask whether the patient has an antiemetic agent. • Have the patient call for emergency help. Correct Because the patient may be experiencing a hypertensive crisis related to the administration of the MAOI, the nurse instructs the patient to call 911 for emergency medical assistance. The nurse also instructs the patient not to drive himself to the hospital because if a hypertensive crisis is in progress, seizures or circulatory collapse is likely and the patient could be endangering his life and the safety of others by driving. Because the nurse cannot know with certainty that the patient is experiencing a hypertensive crisis, the nurse avoids suggesting that the patient lie down and rest because rest is ineffective therapy for this situation; instead, the nurse instructs the patient to seek emergency help. The nurse also avoids interviewing the patient further or instructing him to drink fluids in response to the vomiting because such actions waste time and endanger the patient, who may require emergency treatment. Awarded 1.0 points out of 1.0 possible points. • 15.ID: 10242221479 A female patient who has been taking lithium carbonate (Lithobid) for 1 week tells the nurse that she is experiencing dizziness. What is the best nursing intervention to implement in this situation? • Tell the patient to continue therapy. • Direct the patient to change positions slowly. Correct • Check the serum drug level of lithium. • Ask the patient about her sodium and fluid intake. As a means of maintaining the patient's safety, the most important nursing intervention is instructing the patient to change positions slowly to prevent dizziness. Once action has been taken to maintain patient safety, the nurse gathers additional patient data by investigating possible causes of the dizziness, such as a high lithium level or altered levels of fluids and electrolytes. Unless the nurse has patient data to support the discontinuation of therapy, the nurse instructs the patient to continue taking lithium to prevent disruption of therapy. Awarded 1.0 points out of 1.0 possible points. • 16.ID: 10242221436 The serum lithium level of a patient who takes lithium carbonate (Lithobid) is 1.8 mEq/L. The nurse assesses the patient for which clinical indicators consistent with this concentration of the drug? (Select all that apply.) • Frequent diarrhea Correct • Minor weight loss • Muscle irritability Correct • Fine hand tremors • Adherence to the therapeutic regimen Correct • Irregular heartbeat Correct The therapeutic drug level for lithium is 1 to1.5 mEq/L. This patient's lithium level is above normal, so the nurse expects to observe clinical indicators of lithium toxicity, including diarrhea, muscle irritability, adherence to the therapeutic regimen, and an irregular heartbeat. The adverse effects of lithium therapy are proportionate to the serum level, so the patient's assessment findings are abnormal but not severe. The nurse concludes that the patient has been compliant with the therapeutic regimen because it is unlikely that a toxic drug level could occur with missed doses. A toxic level of lithium is more likely to increase weight, a result of sodium retention; coarse tremors are associated with toxicity. Awarded 1.0 points out of 1.0 possible points. • 17.ID: 10242221409 A patient is detoxifying from alcohol abuse. Which type of medication is indicated to help the patient through withdrawal? • Dibenzapine • Benzisoxazole • Phenothiazine • Benzodiazepine Correct A benzodiazepine is indicated in the management of the clinical manifestations of alcohol withdrawal because of their wide range of therapeutic effects. Dibenzapines, benzisoxazoles, and phenothiazines are antipsychotic agents and are not indicated for alcohol withdrawal. Awarded 1.0 points out of 1.0 possible points. • 18.ID: 10242221451 A female patient who takes lorazepam (Ativan) for anxiety tells the nurse that she plans to become pregnant. What is the best instruction for the nurse to give the patient? • Visit a women's healthcare provider. • Taper off the drug before conception. Correct • Form another plan to manage anxiety. • Eat a well-balanced diet that includes milk. The best instruction for the nurse to provide includes health promotion for the patient and the fetus, so the nurse instructs the patient to taper off therapy as a means of avoiding the adverse effects of withdrawal and to prevent fetal harm. Therapy must be stopped before conception because benzodiazepines are lipid soluble and cross the placenta, increasing the risk of fetal harm. To promote fetal development, the nurse instructs the patient to visit a provider for folic acid and prenatal vitamin prescriptions and to eat a well-balanced diet. To help prevent a crisis, the nurse instructs the patient to develop an alternative plan for managing anxiety with the assistance of a health care provider. Awarded 1.0 points out of 1.0 possible points. • 19.ID: 10242223845 A patient who has been taking alprazolam (Xanax) and has been compliant with the therapeutic regimen for 6 weeks is now complaining of adverse effects of the medication. Which substances does the nurse instruct the patient to avoid to help prevent intensification of this medication's adverse effects? (Select all that apply.) • Alcohol Correct • Opioids Correct • Tobacco • Antihistamines Correct • Muscle relaxants Correct • Caffeinated drinks Because they are also central nervous system (CNS) depressants, the nurse instructs the patient to avoid alcohol, opioids, antihistamines, and muscle relaxants because when taken together with alprazolam they can cause significant CNS depression, including respiratory depression. Tobacco use is likely to be harmful, but it is unlikely to intensify the adverse effects of a benzodiazepine. Caffeine, a xanthine stimulant, is likely to ameliorate CNS depression associated with benzodiazepines. Awarded 1.0 points out of 1.0 possible points. • 20.ID: 10242221427 A male patient taking lorazepam (Ativan) reports lethargy and confusion. Which action should the nurse implement next? • Tell the patient that the symptoms will dissipate gradually. • Plan nursing care to manage a benzodiazepine overdose. • Ask the patient how many doses he has taken in the past 8 hours. Correct • Instruct the patient to rest at home until he is thinking clearly again. The nurse's next intervention is to investigate the patient's complaint completely before planning or implementing nursing care because nursing care is based on patient assessment data. The nurse assesses the patient's condition by asking how much of the medication he has taken recently. In doing so, the nurse can plan nursing care more accurately. The nurse avoids planning care for an overdose because this has not been determined. Instructing the patient to rest at home is a reasonable nursing response to prevent patient injury and may be indicated once a complete assessment has been performed. Once an overdose has been ruled out, the nurse can help the patient understand that the adverse effects of therapy often disappear over time. Awarded 1.0 points out of 1.0 possible points. • 21.ID: 10242223816 A 75-year-old patient is experiencing insomnia. What is the most important reason that the nurse avoids administering a benzodiazepine as a hypnotic agent to this patient? • This will increase the risk of drug interactions. • Benzodiazepines can offer short-term sleepiness only. • Benzodiazepines are addictive when used as a hypnotic agents. • Older adults are sensitive to sedating effects. Correct Older adults tend to be more sensitive than younger people to the sedating effects of benzodiazepines, and because older adults tend to take more medications than a younger adult, the likelihood that the sedative properties will be potentiated by the benzodiazepine is much higher, increasing the risk of patient injury unnecessarily. The risk for addiction is higher with the use of a benzodiazepine rather than another agent to induce sleep, another reason that benzodiazepines are a poor choice of hypnotic agent in older adults; however, the addictive properties are present regardless of the indication for the drug's use. Long-acting benzodiazepines that do not interact adversely with most medications are available. Awarded 1.0 points out of 1.0 possible points. • 22.ID: 10242221494 A male surgical patient in the postanesthesia care unit who was given a benzodiazepine is not breathing. What is the nurse's priority after administering the antidote for this medication to the patient? • Monitoring for dysrhythmias • Taking seizure precautions • Providing pain management • Maintaining oxygen saturation Correct The nurse's priority is to support the patient's airway and breathing for adequate oxygenation because reversing the effects of a benzodiazepine does not guarantee the return of breathing. The administration of flumazenil (Romazicon) is indicated to reverse the effects of a benzodiazepine; however, this medication puts the patient at risk for seizures and dysrhythmias. The patient is likely to need analgesic medication because he is in the immediate postoperative period; however, his pain is unrelated to the airway, breathing, or use of the antidote for a benzodiazepine. That said, the apnea could be the result of the intraoperative administration of an opioid, over which flumazenil would have no effect. None of these issues is more important than maintaining the airway and breathing because these are a patient's most basic needs. Awarded 1.0 points out of 1.0 possible points. • 23.ID: 10242221421 Which patient is a poor candidate for therapy with diazepam (Valium) to treat generalized anxiety disorder? • One who had convulsions as a child • One with a history of alcoholism Correct • One who has had a myocardial infarction • One with type 2 diabetes mellitus The patient with a history of alcoholism is a poor candidate for therapy with diazepam because of the potential for substance abuse and the adverse effects of therapy. The patient has an addictive personality, meaning that the patient has resorted to habitual use of a substance to manage anxiety; as a means of preventing additional substance abuse, benzodiazepines will be withheld from this patient. Moreover, benzodiazepines can cause respiratory depression. If the patient takes the benzodiazepine with alcohol, the combination could result in respiratory failure. Diazepam may be indicated for a patient with a history of convulsions because diazepam has antiseizure properties. The use of diazepam in a patient who has had a myocardial infarction or who has diabetes is potentially suitable. Awarded 1.0 points out of 1.0 possible points. • 24.ID: 10242223832 After benzodiazepine treatment fails, the nurse administers buspirone (BuSpar) to a patient with an anxiety disorder. What patient teaching should the nurse provide to help the patient realize the full benefit of buspirone therapy? • Avoid taking serotonergic agents. • Stand up slowly to help minimize any dizziness. • Take the medication with food to help prevent nausea. • Self-administer buspirone on a consistent basis. Correct The nurse instructs the patient to take buspirone daily and to adhere to the dosing schedule to realize the full benefit of therapy because consistent dosing is important in achieving the full therapeutic effect. Although unrelated to achieving the therapeutic effect, instructing the patient to avoid serotonergic agents, as a means of preventing serotonin syndrome, is a reasonable nursing intervention for a patient taking buspirone. The nurse instructs the patient to change positions slowly if dizziness occurs. Nausea is an unusual effect of buspirone. Awarded 1.0 points out of 1.0 possible points. • 25.ID: 10242221425 A patient with a history of abusing opioid analgesics needs an antianxiety agent. Which medication should the nurse expect to administer? • Diazepam (Valium) • Buspirone (BuSpar) Correct • Venlafaxine (Effexor) • Escitalopram (Lexapro) Because the potential for abuse is low, buspirone is a suitable antianxiety agent for this patient. Diazepam is contraindicated because benzodiazepines are highly addictive. Venlafaxine is a serotonin-norepinephrine reuptake inhibitor and escitalopram is a selective serotonin reuptake inhibitor; both medications have a low potential for abuse and are first-line antidepressant therapies. The nurse does not know whether the patient has depression along with the anxiety, so these drugs are not indicated. Awarded 1.0 points out of 1.0 possible points. • 26.ID: 10242221472 Which medication is used as first-line therapy? • Sertraline (Zoloft) Correct • Haloperidol (Haldol) • Meprobamate (Miltown) • Chlorpromazine (Thorazine) Sertraline, a selective serotonin reuptake inhibitor, is a first-line therapy for depression. Haloperidol and chlorpromazine are conventional antipsychotic agents but not first-line therapies for psychosis. Meprobamate is an anxiolytic agent but not a first-line therapy for anxiety. Awarded 1.0 points out of 1.0 possible points. • 27.ID: 10242221423 A patient who is has taken fluoxetine (Prozac) for 2 weeks to treat an anxiety disorder complains that he is not satisfied with the therapy. What is the best information for the nurse to include in patient teaching to promote adherence to the therapeutic regimen? • The adverse effects can be managed well. • This medication usually requires titration. • Relaxation exercises can offer some relief. • A therapeutic effect is expected 2 to 4 weeks after the start of therapy. Correct The full therapeutic effects of selective serotonin reuptake inhibitor (SSRI) therapy may take 4 to 6 weeks to appear, so this patient can anticipate experiencing a therapeutic effect in 2 to 4 more weeks. Knowing the timeframe offers the patient realistic hope and provides a justification for adherence to therapy. Adverse effects can usually be managed, and relaxation exercises may provide some relief from anxiety. The patient must fulfill these tasks to get the full therapeutic effect of the medication, but it can be difficult for a patient with depression to do so. SSRIs can require considerable titration, but, because of the nature of the patient's illness, this information is unlikely to promote adherence to therapy. Awarded 1.0 points out of 1.0 possible points. • 28.ID: 10242221413 A female patient with psychosis is experiencing adverse effects of conventional antipsychotic pharmacotherapy, including dystonia, akathisia, and abnormal limb movements. The nurse collaborates with the psychiatrist to enact a change in therapy. Which medication is best suited to this patient? • Molindone (Moban) • Haloperidol (Haldol) • Risperidone (Risperdal) Correct • Chlorpromazine (Thorazine) Risperidone is the best medication for this patient; she is experiencing dopamine receptor-related adverse effects of a conventional antipsychotic agent, and risperidone has strong antidopaminergic properties as well as antiadrenergic, antiserotonergic, and antihistaminic activity. Molindone, haloperidol, and chlorpromazine, all conventional antipsychotic agents, could aggravate the adverse effects experienced by the patient. Awarded 1.0 points out of 1.0 possible points. • 29.ID: 10242221487 A patient who takes benztropine (Cogentin) needs an antidepressant. Which medication should the nurse avoid administering to prevent anticholinergic syndrome? • Selegiline (Emsam) • Duloxetine (Cymbalta) • Protriptyline (Vivactil) Correct • Buproprion (Wellbutrin) Benztropine is an anticholinergic agent used in the treatment of Parkinson's disease. Tricyclic antidepressants like protriptyline (Vivactil) can cause anticholinergic syndrome when combined with benztropine because they block cholinergic receptors. Selegiline is a reasonable choice of antidepressant for a patient with Parkinson's disease because it inhibits monoamine oxidase selectively. Duloxetine and buproprion are not indicated for this patient. Awarded 1.0 points out of 1.0 possible points. • 30.ID: 10242223861 A patient takes sertraline (Zoloft) for depression related to chronic pain. The nurse avoids administering which analgesic agent to help prevent serotonin syndrome? • Tramadol (Ultram) Correct • Ibuprofen (Motrin) • Fentanyl (Duragesic) • Oxycodone (OxyContin) The nurse avoids administering tramadol to a patient who takes a selective serotonin reuptake inhibitor because it increases the risk for serotonin syndrome. This is because tramadol exerts its analgesia by blocking the reuptake of norepinephrine and serotonin. Ibuprofen is unlikely to provide relief to a patient with chronic pain unless the pain has developed an inflammatory aspect. Fentanyl and oxycodone are reasonable choices of analgesics for this patient, but both agents require careful monitoring of the patient. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-k7oh-2goumpxi!reviewSubmittedAssessmentAttempt?attempt=17683944068> Ch.17 • 1.ID: 10242195424 The nurse knows that which statement is true about the individual experiencing drug tolerance? • The individual is dependent on another drug because of effects of the primary drug. • The individual seeks compulsive dose escalation with subsequent drug doses. Correct • The individual experiences indicators of withdrawal when the drug is stopped. • The individual feels an intense subjective need or craving for a particular drug. Tolerance, which results from regular drug use, can be defined as a state in which a particular dose of drug elicits a smaller response than it did with initial use. As tolerance increases, higher and higher doses are needed to elicit the desired effect. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242197320 Which protein in the central nervous system (CNS) interacts with alcohol and elicits acute effects in an individual who has been drinking? • Gamma-aminobutyric acid Correct • Albumin • Serotonin • Gamma-hydroxybutyric acid The protein of particular importance in the CNS that interacts with alcohol is gamma-aminobutyric acid, commonly known as GABA. Albumin is a serum protein produced by the liver; serotonin is a neurotransmitter; and gamma-hydroxybutyric acid, or GHB (often known as the "date-rape drug"), inhibits GABA. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242195464 What effects of marijuana might a nurse assess in a patient who has committed long-term marijuana abuse? (Select all that apply.) • Frequent headaches • Effects similar to those of long-term smoking Correct • Memory and attention deficits Correct • Dry mouth and nausea • Agitation Long-term use of marijuana may result in chronic respiratory symptoms (similar to those of tobacco abuse) and memory and attention deficit problems. A chronic depressive "amotivational" syndrome has also been observed, especially among younger users. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242195456 A person becomes dizzy on standing up after drinking a glass of wine. What is the most likely reason for the dizziness? • Alcohol decreases the heart rate. • Alcohol causes vasoconstriction. • Alcohol increases blood pressure. • Alcohol dilates the blood vessels. Correct Alcohol causes blood vessels to dilate, resulting in the pooling of blood in the periphery. When the vessels dilate, they hold a disproportionate amount of blood in the periphery; the person experiences dizziness on trying to stand because the body lacks the vascular muscle tone to compensate quickly, constrict peripheral blood vessels, increase the blood pressure, and deliver enough blood to the brain to prevent dizziness. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242197302 A snow-skiing instructor tells students to avoid drinking alcohol before and during skiing, for safety's sake. About which adverse effect of alcohol is the instructor most likely warning the skiers? • Diuresis • Accidents • Diaphoresis • Hypothermia Correct Alcohol dilates blood vessels, allowing blood to pool in the periphery and causing heat to be lost more rapidly, which increases the risk of hypothermia. Although alpine skiers are less likely to experience alcohol-induced diaphoresis because of the cold temperatures associated with snow skiing, diaphoresis in a cold environment can contribute to heat loss, thereby causing hypothermia indirectly. Alcohol does cause diuresis, but this should not pose a significant risk for skiers. Although accidents are not a direct adverse effect of alcohol use, alcohol is contraindicated for skiers because alcohol impairs coordination, increasing the risk of accidents. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242197311 Alcohol promotes diuresis by doing what? • Increasing release of aldosterone • Decreasing release of aldosterone • Increasing release of antidiuretic hormone • Decreasing release of antidiuretic hormone Correct Alcohol exerts a diuretic effect by inhibiting the release of antidiuretic hormone (ADH) the water-conserving hormone, from the pituitary. This impairs reabsorption of water by the kidneys, thereby increasing urine output. Aldosterone is the sodium-conserving hormone. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242195484 The nurse wants to help prevent liver failure in a patient who drinks alcohol frequently. Which drug should the nurse instruct the patient to avoid? • Acetaminophen Correct • An antihypertensive drug • An antianxiety agent • Methamphetamine Taking acetaminophen when a serum alcohol level is present causes alterations in the metabolism of these substances, leading to the formation of toxic byproducts, as well as decreased drug clearance and an increased risk of serious liver damage and death. Although antianxiety agents do not cause liver failure when taken with alcohol, the nurse should instruct the patient who drinks alcohol frequently to avoid antianxiety agents as a means of preventing enhancement of the central nervous system depression that is characteristic of both agents. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242195449 A patient is taking disulfiram (Antabuse) and wants to know what will occur if she continues to drink alcohol. What is the nurse's best response? • You will experience lethargy, so you shouldn't drive. • You will experience nausea, weakness, and blurred vision. Correct • You will have severe lower back, leg, and abdominal pain. • You will have increased blood pressure and experience hyperactivity. Disulfiram is used as aversion therapy in the treatment of alcoholism. The use of alcohol with disulfiram can result in nausea, severe vomiting, weakness, blurred vision, and hypotension. In fact, the patient may experience profound hypotension. This reaction, which may last anywhere from 30 minutes to several hours, may be brought on by the consumption of as little as 7 mL of alcohol. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242195492 Which medication is approved to help reduce an individual's craving for alcohol? • Naltrexone (ReVia) Correct • Disulfiram (Antabuse) • Acamprosate (Campral) • Methadone (Methadose) Naltrexone is a pure opioid antagonist that reduces the craving for alcohol and blocks its pleasurable effects. Disulfiram is used to prevent alcohol consumption; acamprosate is used to maintain alcohol abstinence; and methadone is used to help reduce dependence on opioids. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242195422 Which approved medication will ease the unpleasant feelings brought on by abstinence from alcohol? • Naltrexone (ReVia) • Disulfiram (Antabuse) • Acamprosate (Campral) Correct • Methadone (Methadose) Acamprosate is indicated for the maintenance of abstinence in patients with alcohol dependence after detoxification. Benefits are derived from a reduction in the unpleasant feelings brought on by abstinence. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242197327 A patient presents to the emergency department with respiratory depression, lethargy, and pinpoint pupils. These findings are consistent with clinical indicators of an overdose of which agent? • Opioid Correct • Alcohol • Ecstasy • Marijuana Opioid overdose produces a classic triad of symptoms: respiratory depression, depressed level of consciousness, and pinpoint pupils. The effects of this overdose can be reversed with the use of naloxone (Narcan). Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242195436 Which manifestations are seen in a person who smokes marijuana? (Select all that apply.) • Anorexia • Tachycardia Correct • Hypersomnia • Unsteady gait Correct • Mild euphoria Correct • Hallucinations Correct The effects of marijuana use include tachycardia resulting from sympathetic stimulation, unsteadiness, euphoria, and hallucinations caused by stimulation of cannabinoid receptors. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242195474 Which abused drug is commonly taken by mouth, inhalation, or injection? • Heroin • Ecstasy Correct • Cocaine • Nicotine Ecstasy may be taken by mouth, inhaled, or injected. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242197334 Nicotine is contraindicated in patients with cardiovascular disease because of which effect? (Select all that apply.) • Impairs lipid metabolism • Increases gastric motility • Accelerates heart rate Correct • Increases blood pressure Correct • Promotes vasoconstriction Correct • Depresses chest expansion A patient with cardiovascular disease may be unable to meet the increased tissue oxygen demand created by nicotine because it imparts an excessive workload on a weakened or inadequate cardiovascular system. Nicotine acts by stimulating nicotinic receptors in the sympathetic ganglia and the adrenal medulla to promote vasoconstriction, acceleration of the heart rate, increased force of ventricular contractions, and increased blood pressure. The increased myocardial oxygen consumption required may be something the patient's cardiovascular system is unable to provide. Awarded 1.0 points out of 1.0 possible points. • 15.ID: 10242195428 The nurse prepares to assess a 74-year-old male patient who abuses alcohol. Which assessment tool is the best choice for this patient? • SASSI • POSIT • MAST-G Correct • CAGE-AID MAST-G is the Michigan Alcoholism Screening Test Geriatric version, a substance abuse assessment tool with proven validity and reliability. POSIT (the Problem-Oriented Screening Instrument for Teenagers) is an assessment tool for use in teenagers; SASSI (Substance Abuse Subtle Screening Inventory) and CAGE-AID (CAGE Questions Adapted to Include Drugs) are assessment tools suitable for use in adults. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-egaz-cpoumpxi!reviewSubmittedAssessmentAttempt?attempt=17684023487> Chapter 18 1. .ID: 10242262186 To relax vascular smooth muscle, the nurse administers an adrenergic agent that acts as an agonist on which receptors of the sympathetic nervous system? • Beta1 • Beta2 Correct • Alpha1 • Alpha2 Stimulation of beta2 receptors relaxes smooth muscle in the vasculature as well as smooth muscle in the uterus, bronchioles, and gastrointestinal tract. Stimulation of beta1 receptors results in positive inotropic, dromotropic, and chronotropic action. Stimulation of alpha1 receptors induces vasoconstriction and constriction of sphincter muscles and the uterus. Stimulation of alpha2 receptors reverses sympathetic action insignificantly. Awarded 1.0 points out of 1.0 possible points. 2. 2.ID: 10242262196 Which physiologic component of the "fight-or-flight" response is a result of the stimulation of beta1 receptors? • Relaxation of uterine smooth muscle • Increased contractility of myocardium Correct • Relaxation of bronchial smooth muscle • Increased resistance of peripheral vessels Stimulation of beta1 receptors in the "fight-or-flight" response results in stronger ventricular contraction because this response includes increases in heart rate and blood pressure, shunting of blood away from the skin and viscera, dilation of bronchi to improve oxygenation, dilation of pupils to increase visual acuity, and mobilization of stored energy. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242262178 The nurse administers midodrine (ProAmatine) to a patient. Which parameter should the nurse assess to evaluate the therapeutic effect of this medication? • Pulse rate • Temperature • Blood pressure Correct • Respiratory rate Midodrine, an alpha1 agonist, is used mainly in the treatment of symptomatic orthostatic hypotension, so the nurse measures the patient's blood pressure before and after the patient stands as a means of evaluating the therapeutic effectiveness of the drug. Midodrine acts by means of vasoconstriction, so if the drug is effective, the nurse expects the patient's blood pressure to remain relatively stable when the patient stands from a lying or sitting position. Measuring the patient's blood pressure in this manner helps the nurse determine the strength of the patient's baroreceptor reflex, an important compensatory mechanism of the autonomic nervous system. If the reflex is intact, the blood pressure should not fall when the patient stands, indicating that the vasculature is compensating as the patient stands by constricting to maintain the blood pressure and, more important, blood flow to the brain. If the reflex is not strong, the patient will become dizzy or faint on standing. Midodrine should not affect the patient's heart rate, temperature, or respiratory rate. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242262190 The nurse is administering an alpha1 agonist. What should the nurse assess to evaluate the therapeutic effectiveness of the medication? (Select all that apply.) • Motility of the gastrointestinal tract • Ventilation of the lungs • Muscle tone of the uterus Correct • Constriction of the pupils • Coolness of the skin at the periphery Correct • Level of consciousness Alpha1 receptors are located in the eyes, blood vessels, male sex organs, and bladder. Activation of these receptors results in mydriasis (dilation of pupils), vasoconstriction, ejaculation, and bladder and uterine contractions. The patient's skin should feel cool as a result of vasoconstriction. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242262198 Which adrenergic receptors do selective beta-adrenergic blockers antagonize? • Beta1 Correct • Beta2 • Alpha1 • Alpha2 Beta1 receptors are located in the heart, kidney, and bronchioles. By blocking the effects of beta1 receptors, selective beta-adrenergic blockers decrease myocardial contractility, heart rate, and atrioventricular conduction, and dilate bronchioles. Blockade of beta2 receptors does the opposite. Alpha1 stimulation induces vasoconstriction and alpha2 stimulation–induced vasodilation. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242262176 Adrenergic agonists are also known as what? • Sympathetic antagonists • Sympathomimetic agents Correct • Parasympathetic antagonists • Parasympathomimetic agents Adrenergic agonists produce their effects by activating adrenergic receptors. Because the sympathetic nervous system acts through the same receptors, responses to adrenergic agonists mimic stimulation of the sympathetic system. For this reason, adrenergic agonists are often referred to as sympathomimetic agents. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242264702 What is the goal of therapy when an alpha1-receptor agonist is administered? • Tachycardia • Bradycardia • Vasodilation • Vasoconstriction Correct Activation of alpha1 receptors causes vasoconstriction and mydriasis. Alpha1-receptor agonists are used to induce hemostasis and nasal decongestion, to increase blood pressure, and are also employed as adjuncts to local anesthesia. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242262194 A patient has mitral valve regurgitation, and the nurse's goal is to prevent aggravation of the regurgitation. What is the most important adrenergic medication for the nurse to avoid administering to this patient? • Dobutamine (Dobutrex) • Fenoldopam (Corlopam) • Epinephrine (Adrenalin) • Phenylephrine (Neo-Synephrine) Correct The nurse avoids administration of phenylephrine to this patient because it is an alpha1-receptor agonist that causes vasoconstriction. Vasoconstriction aggravates mitral valve regurgitation by increasing preload and impeding the forward flow of blood. These factors can cause the heart to fail because the heart becomes an ineffective pump. Dobutamine is a positive inotrope; fenoldopam is a peripheral dopamine agonist that causes blood pressure to drop; and epinephrine, although it can stimulate alpha1 receptors at high dosages, acts to increase the heart rate and myocardial contractility, in addition to dilating the bronchioles. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242262182 Which positive effect does the nurse administering a beta1 agonist to a patient with heart failure hope to achieve? • Positive inotropic action Correct • Positive chronotropic action • Increased ventricular filling • Increased ventricular relaxation Heart failure renders the heart an ineffective pump characterized by weak myocardial contractility; administration of a beta1 agonist, a positive inotropic agent, increases the strength of each contraction and increases the pumping efficiency of the heart. A positive chronotropic effect increases the heart rate, which can be a devastating stressor on a failing heart. Ventricular filling and relaxation might be affected by improved myocardial contractility, but a beta1 agonist is more likely to impair these aspects of the cardiac cycle. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242264700 The nurse is delivering a high-dose IV infusion of epinephrine (Adrenalin) to a patient. Which pieces of patient assessment data indicate adverse effects of this medication? (Select all that apply.) • Heart rate 120 beats/min Correct • Blood sugar 100 mg/dL • Breath sounds clear • Bowel sounds present • Prolonged QTc interval • Blood pressure 168/102 mm Hg Correct Administered at high dosages, epinephrine causes tachycardia, release of glucose from the liver, decreased gastrointestinal motility, bronchodilation, and increased blood pressure resulting from vasoconstriction due to alpha1 stimulation. Epinephrine should not affect the QTc interval. Clear breath sounds and audible bowel sounds are normal findings and, thus, are not adverse effects of therapy. The blood sugar is normal. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242262184 What effect of low-dose epinephrine makes it useful during cardiopulmonary resuscitation (CPR)? (Select all that apply.) • Increases the heart rate Correct • Increases serum glucose • Improves vital organ perfusion Correct • Facilitates pulmonary ventilation Correct • Increases myocardial contractility Correct • Cause faster peristaltic action Epinephrine is an important medication during CPR because, in low doses, it helps restore vital functions, including heart rate, organ perfusion, ventilation, and efficient myocardial contraction. Low-dose epinephrine accomplishes these actions by stimulating beta1 receptors but loses these attributes when the dosage is increased, because it then stimulates alpha1 receptors, causing vasoconstriction. Epinephrine also increases the serum glucose, but this is not necessarily beneficial in CPR and can cause harm if the serum glucose becomes too high. Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242262192 For which adverse effects should the nurse monitor the patient receiving epinephrine? (Select all that apply.) • Slowed heart rate • Hypertensive crisis Correct • Increased blood sugar Correct • Chest pain Correct • Dysrhythmias Correct • Increased gastrointestinal motility Adverse effects from epinephrine include angina caused by an increased heart rate or increased myocardial contractility, both of which increase myocardial oxygen consumption. Epinephrine can also cause dysrhythmias resulting from increased myocardial stimulation and increased myocardial oxygen consumption, hypertensive crisis caused by vasoconstriction, and hyperglycemia resulting from hepatic release of glucose. Epinephrine is more likely to cause tachycardia and decreased gastrointestinal motility. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242262180 A male patient with an ischemic cardiomyopathy receives dobutamine (Dobutrex). Which patient assessment finding does the nurse make a priority to prevent? • Normal sinus rhythm • Urine output 30 mL/hr • Cool, pale extremities Correct • Blood sugar 85 mg/dL Cool, pale extremities indicate increased peripheral vascular resistance resulting from alpha1-receptor stimulation and may indicate that the dobutamine dosage is too high. The benefits of dobutamine infusion include improved myocardial contractility without appreciable increases in heart rate, blood pressure, peripheral vascular resistance, or myocardial oxygen consumption. These are vital benefits in a patient with ischemic heart disease because the heart's ability to supply adequate oxygen to the myocardium is impaired. The cardiac rhythm, urine output, and blood glucose reading listed here are all normal and desirable for a patient receiving dobutamine. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242262188 Patients return from coronary artery bypass surgery (CABG) in a hypothermic state. Which adrenergic agonist should the nurse prepare to administer to help prevent increased myocardial oxygen consumption? • Dobutamine (Dobutrex) • Epinephrine (Adrenalin) • Fenoldopam (Corlopam) Correct • Midodrine (ProAmatine) Fenoldopam is a dopamine1 agonist that works on the vascular smooth muscle to induce vasodilation and decrease blood pressure. Fenoldopam is indicated after CABG in the intensive care unit as the patient is warming, to relieve the vasoconstriction characteristic of hypothermia, to decrease peripheral vascular resistance, and to decrease the myocardial workload and thus myocardial oxygen consumption. Usually, fenoldopam can be discontinued as soon as the patient's temperature returns to normal. Dobutamine is not indicated to relieve vasoconstriction. Epinephrine and midodrine are contraindicated for this patient, unless the cardiopulmonary arrest occurs, because they are likely to increase peripheral vascular resistance. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-663n-kqpumpxi!reviewSubmittedAssessmentAttempt?attempt=17738620712> Chapter 19 • 1.ID: 10242227189 For which conditions are alpha1-adrenergic blockers indicated? (Select all that apply.) • Heart block • Acrocyanosis Correct • Hypertension Correct • Extravasation Correct • Dysrhythmias • Fluid overload Alpha1-adrenergic antagonists, which induce vasodilation by blocking alpha1 receptors, are used primarily for the treatment of hypertension. It is these characteristics that make alpha1 blockers useful in the treatment of acrocyanosis and tissue extravasation. Alpha1 blockers are not indicated in the treatment of hypervolemia, heart block, or dysrhythmias. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242227191 An 83-year-old patient is having difficulty taking prazosin (Minipres) for hypertension. Which problems are adverse effects of prazosin that make the drug a poor choice for this patient? (Select all that apply.) • Muscle spasms • Hyperglycemia • Seizure activity • Reflex tachycardia Correct • Urinary incontinence Correct • Orthostatic hypotension Correct Adverse effects of alpha1-adrenergic agonists include orthostatic hypotension, reflex tachycardia, and urinary incontinence. By blocking alpha1 receptors, these medications displace norepinephrine from the receptor and remove the related sympathetic stimulation of norepinephrine. Prazosin is a poor choice of antihypertensive for an older adult patient because orthostatic hypotension increases the risk of patient injury and reflex tachycardia increases myocardial oxygen consumption. Urinary incontinence caused by the relaxation of the urinary sphincter also makes prazosin a poor choice for this patient because older adults are already at increased risk for incontinence. Hyperglycemia, spasms, and seizures are not associated with the administration of alpha1 blockers. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242227193 A patient who has coronary artery disease (CAD) receives a prescription for metoprolol (Toprol). Which baseline reading should the nurse record during the preadministration patient assessment to facilitate evaluation of the drug's therapeutic effectiveness? • Angina description Correct • Fluid volume status • Peripheral circulation • Bilateral breath sounds The nurse assesses the patient's angina before administering metoprolol to aid evaluation of the drug's therapeutic effectiveness because one indication for a cardioselective beta blocker is angina. These medications are indicated for angina in CAD because they decrease myocardial oxygen consumption by slowing conduction through the myocardium and by decreasing the heart rate and myocardial contractility. A cardioselective beta blocker is not indicated for the treatment of hypervolemia, improvement of peripheral circulation, or improvement of ventilation. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242227195 Beta2-blocking agents are contraindicated in patients with which health concern? • Wheezing Correct • Chest pain • Hypertension • Dysrhythmias Blockage of beta2 receptors in the lung can cause constriction in the bronchi. In patients with asthma, an increase in airway resistance can be life threatening. Therefore, drugs that block beta2 receptors are contraindicated in patients with asthma. A patient with asthma who needs a beta blocker should receive a beta2-selective drug. Beta2 blockers are indicated in the treatment of angina, hypertension, and dysrhythmias. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242227187 A patient with heart failure receives carvedilol (Coreg). What mechanism causes cardiac output (CO) to remain stable or to improve after the administration of this medication? • Increased preload • Increased heart rate (HR) • Increased stroke volume (SV) Correct • Increased vascular resistance Carvedilol is a nonselective beta blocker used in the treatment of heart failure to preserve or increase cardiac output. CO equals the stroke volume times the HR (CO = SV * HR), so for a stable CO to be maintained, the HR, SV, or both must increase. The goal of therapy in this patient is to avoid increasing the heart rate, which would increase myocardial oxygen consumption. For this reason, the stroke volume must be increased to maintain the CO; this is accomplished by administering a medication such as carvedilol because the slower HR and decreased myocardial contractility allow the ventricles to fill and empty more efficiently, thereby increasing the SV to maintain CO. Preload and vascular resistance will not increase with the administration of carvedilol, a vasodilator, because it allows blood to pool in the periphery. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-x0sq-hvpumpxi!reviewSubmittedAssessmentAttempt?attempt=17738686771> Chapter 20 • 1.ID: 10242199572 What is a clinical indicator of parasympathetic nervous system stimulation? • Dilation of the pupils • Retention of urine • Dilation of the bronchi • Slowing of the heart rate Correct The parasympathetic nervous system performs seven regulatory functions: slowing the heart rate, increasing gastric secretions, emptying the bladder, emptying the bowel, focusing the eye for near vision, constricting the pupil, and contracting bronchial smooth muscle. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242199576 Which clinical indicators should the nurse monitor as a means of observing the activation of muscarinic receptors? • Urinary retention • Increased heart rate • Decreased gastric secretion • Increased bronchial secretion Correct Muscarinic receptor activation causes an increase in secretions from the pulmonary system. Muscarinic stimulation causes contraction of smooth muscle in the bronchi, increases bladder tone (but relaxes urinary sphincters), and slows the heart rate. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242199578 What is another name for a muscarinic agonist? • Sympatholytic agent • Sympathomimetic agent • Parasympatholytic agent • Parasympathomimetic agent Correct Muscarinic agents are associated with the parasympathetic nervous system and mimic agents produced by stimulation of the parasympathetic nerves. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242199574 A patient with Alzheimer's disease wants to try donepezil (Aricept). Which co-morbidity is a contraindication to the use of donepezil to improve memory and learning? • Heart block Correct • Constipation • Hypertension • Urine retention Muscarinic agonists, which act on the heart to slow the heart rate, are contraindicated in a patient with heart block because they may hasten deterioration of the conduction defect. Donepezil is more likely to increase gastrointestinal motility, facilitate bladder emptying, and reduce blood pressure. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242199562 The nurse administers pilocarpine (Pilocar) ophthalmic drops to a patient. For which clinical indicator should the nurse monitor the patient as a means of evaluating the therapeutic effectiveness of the ophthalmic treatment? • Dilated pupils • Dull, dry eyes • Farsightedness • Constricted pupils Correct A parasympathomimetic agent such as pilocarpine causes activation of muscarinic receptors in the eye, producing miosis, or pupillary constriction, and contraction of the ciliary muscle, which results in accommodation for near vision. Administration of a cholinergic agonist is more likely to cause lacrimation and myopia than dry eyes and hyperopia (farsightedness). Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242199570 The nurse administers bethanechol (Urecholine) to a patient. Which piece of equipment should the nurse use to evaluate the therapeutic effectiveness of pharmacotherapy? • Pain scale • Stethoscope • Thermometer • Bladder ultrasound Correct Bethanechol is indicated in the treatment of urine retention, so the nurse uses an ultrasound device to scan the patient's bladder as a means of evaluating the drug's effect on bladder emptying. Bethanechol works by relaxing sphincter muscles and increasing muscle tone to increase voiding pressure. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242199566 The nurse prepares to administer bethanechol (Urecholine) to a patient who underwent surgery 1 day earlier. Which piece of subjective patient assessment data is a contraindication to the use of this drug? • History of asthma Correct • Bilateral wheezing • Blood pressure 140/83 mm Hg • Use of an antihypertensive drug Bethanechol is contraindicated in patients with active or latent asthma because it activates muscarinic receptors in the lungs, causing bronchoconstriction. Bethanechol can cause hypotension as a result of vasodilation, so hypertension is not a contraindication to its use. A finding of bilateral wheezing and blood pressure readings are examples of objective data. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242199556 A patient takes more than one cholinergic agonist that stimulates muscarinic receptors. Which parameter does the nurse make a priority of monitoring to help prevent serious adverse effects of therapy? • Lacrimation • Bowel pattern • Blood pressure Correct • Urinary pattern The clinical indicators of excessive doses of muscarinic agents are exaggerations of normal muscarinic stimulation. Serious adverse effects of cholinergic therapy that stimulates muscarinic receptors include orthostatic hypotension, so the nurse monitors the blood pressure for early detection of hypotension. Although muscarinic poisoning is likely to cause increased lacrimal secretion, diarrhea, and urinary frequency, these problems are less important than hemodynamic changes. Awarded 1.0 points out of 1.0 possible points. • 9.ID: 10242199584 A 75-year-old patient experiences severe vomiting and diarrhea after receiving tacrine (Cognex). Which action should the nurse implement next? • Maintaining the patient in NPO status • Offering an antiemetic injection • Preparing to empty the patient's stomach • Preparing to administer atropine Correct The patient is exhibiting clinical indicators of muscarinic poisoning, and management of muscarinic poisoning requires the administration of atropine, a selective muscarinic blocking agent (anticholinergic agent). By blocking access of muscarinic agonists to their receptors, atropine can reverse most signs of toxicity or poisoning. Keeping the patient in nothing-by-mouth status and emptying the stomach are reasonable responses; with vomiting it is usually necessary to empty the stomach, allow the gastrointestinal system to become less irritable, and then allow the patient to take oral fluids again slowly. An antiemetic may be indicated for symptomatic relief; however, this may be unnecessary if the antidote, atropine, reverses the toxicity and stops the vomiting. Awarded 1.0 points out of 1.0 possible points. • 10.ID: 10242199580 Which drug is indicated in the treatment of myasthenia gravis? • Pilocarpine (Salagen) • Rivastigmine (Exelon) • Neostigmine (Prostigmin) Correct • Succinylcholine (Anectine) Neostigmine is a reversible anticholinesterase agent, and its principal use is the treatment of myasthenia gravis. Neostigmine works by preventing the inactivation of acetylcholine at the neuromuscular junction, leading to increased nerve transmission and skeletal muscle activation. Pilocarpine inhibits cholinesterase to allow acetylcholine accumulation; however, it is indicated in the treatment of glaucoma and is administered as ophthalmic drops. Rivastigmine is a cholinesterase inhibitor indicated for use in Alzheimer's dementia. Succinylcholine is a direct-acting cholinergic neuromuscular-blocking agent. Awarded 1.0 points out of 1.0 possible points. • 11.ID: 10242199558 Which uses are clinical indications for a cholinesterase inhibitor such as physostigmine (Antilirium)? (Select all that apply.) • As an antidote in biochemical warfare Correct • To relieve severe constriction of the bronchioles • Treatment for a patient with a prolonged history of difficulty with sleep • To diagnose and treatment myasthenia gravis Correct • As an antidote to tricyclic antidepressant toxicity Correct When used therapeutically, cholinesterase inhibitors, such as physostigmine, affect the muscarinic receptors and nicotinic receptors of the neuromuscular junction, thereby helping restore acetylcholine to the level needed for nerve impulse transmission. Because patients with myasthenia gravis lack sufficient release of acetylcholine at the neuromuscular junction, administration of physostigmine helps improve muscle strength by decreasing the destruction of acetylcholine. Because of its capacity to restore the acetylcholine level, this medication is useful as an antidote to biochemical warfare involving anticholinergic agents as well as in tricyclic antidepressant toxicity. Physostigmine therapy is contraindicated in patients with insomnia and bronchoconstriction. Awarded 1.0 points out of 1.0 possible points. • 12.ID: 10242199564 A patient takes pyridostigmine (Mestinon), and the nurse provides patient teaching. Which information should the nurse provide to help prevent a cholinergic crisis? • Seek medical help for nausea and vomiting. Correct • Ask for help to change positions or to stand. • Take the medication 30 minutes before eating. • Take the medication promptly for drooping eyelids. Cholinergic crisis may occur with an overdose of anticholinesterase therapy. Early clinical indicators of cholinesterase inhibitor overdose include nausea, vomiting, flushing, and abdominal cramps. Dizziness may occur with standard therapy, and hypotension occurs with an overdose. The nurse instructs the patient to take the medication before eating to strengthen the muscles involved in chewing and swallowing and to help prevent aspiration or choking. The nurse instructs the patient to take the medication at the first sign of muscle weakness, and an early sign of impending muscle weakness in larger muscle groups is drooping eyelids. Awarded 1.0 points out of 1.0 possible points. • 13.ID: 10242199554 A patient takes rivastigmine (Exelon) and experiences complete heart block, indicated by flushing and increased salivation. Which medication should the nurse administer to most directly improve the patient's condition? • Atropine (Atropine) Correct • Dopamine (Intropin) • Epinephrine (Adrenalin) • Lidocaine (Lidocaine) The nurse should administer atropine intravenously to treat the muscarinic effects of cholinesterase because atropine is an anticholinergic agent used in the treatment of excessive anticholinesterase therapy. The patient may also require cardiopulmonary resuscitation or other emergency treatment. Awarded 1.0 points out of 1.0 possible points. • 14.ID: 10242199568 Patients with a history of which disorders should not receive a medication such as galantamine (Razadyne)? (Select all that apply.) • Emphysema Correct • Osteoporosis • Crohn's disease Correct • Atrial fibrillation Correct • Bladder infections • Poor attention span Patients with emphysema, Crohn's disease, and atrial fibrillation should not receive galantamine, an anticholinesterase medication. A patient with obstructive lung disease should not receive this medication because it can cause bronchospasm. A patient with Crohn's disease should not receive galantamine because of the potential for bowel perforation that is characteristic of Crohn's disease. Finally, patients with atrial fibrillation should not receive galanfamine because it can slow the heart rate. A slower heart rate is a potential problem for a patient with atrial fibrillation if the cholinesterase inhibitor decreases the ventricular rate to a level insufficient to maintain a normal blood pressure. Galantamine may be indicated for patients with osteoporosis and poor attention span, and it may be of help to a patient with frequent bladder infections resulting from urine retention. Awarded 1.0 points out of 1.0 possible points. • 15.ID: 10242199582 A patient undergoing maintenance therapy with which cholinergic agonist medication is receiving the proper dose? • Donepezil (Aricept) 10 mg twice a day by mouth • Memantine (Namenda) 10 mg twice a day by mouth Correct • Bethanechol (Urecholine) 5 mg three times a day by mouth • Physostigmine (Antilirium) 2 mg every 20 minutes by mouth The dosage range for memantine is initial dose is 5 mg/day; titrate by 5 mg/wk up to a target dose of 10 mg/bid (20 mg/day). Maximum dose in renal impairment is 10 mg/day. Donepezil 10 mg twice a day is an excessive dose. Bethanechol 5 mg three times a day is a subtherapeutic dose. Physostigmine is administered by means of injection. Awarded 1.0 points out of 1.0 possible points. • 16.ID: 10242199560 A patient with Alzheimer's disease is prescribed a cholinesterase inhibitor to improve memory and learning. Which physiologic trait is required for the patient to benefit from the medication? • Sensitivity to anticholinergic agents • Endogenously released acetylcholine Correct • Functioning neuromuscular junctions • Alertness and orientation to surroundings To benefit from cholinergic agonist therapy, the patient with Alzheimer's must have neurons that release acetylcholine. This is because these medications act by inhibiting acetylcholinesterase, the enzyme that breaks down Ach, thereby increasing the level of acetylcholine in the brain. Sensitivity to anticholinergic agents is unrelated; neuromuscular junctions are not involved because the medications for Alzheimer's work on the acetylcholine level in the brain. Patients receive these medications to approach individual orientation to surroundings. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-h8oz-q0qumpxi!reviewSubmittedAssessmentAttempt?attempt=17738795783> Chapter 21 • 1.ID: 10242236811 Which finding is a therapeutic effect of atropine? • Miosis • Lethargy • Hypertension • Sinus rhythm Correct Atropine, a muscarinic antagonist, works primarily on the heart, exocrine glands, smooth muscle, and eyes and produces an increased heart rate. The nurse does not anticipate sinus tachycardia because this medication is indicated for the use of bradycardia. Because there is no parasympathetic innervation to muscarinic receptors in blood vessels, atropine has no effect on vascular smooth muscle tone and therefore no effect on blood pressure. Atropine is likely to cause mydriasis. Awarded 1.0 points out of 1.0 possible points. • 2.ID: 10242236809 The nurse is educating a patient who is taking an anticholinergic medication. What should the patient do to decrease the effects of dry mouth? (Select all that apply.) • Floss and brush teeth twice a day Correct • Use artificial saliva drops Correct • Chew on ice chips • Maintain regular dental visits Correct • Use sugarless candy or gum Correct Anticholinergics may cause dry mouth. Regular and thorough oral hygiene is required, including brushing teeth and flossing twice daily. Dry mouth may be minimized by use of artificial saliva drops, sugarless gum, or sugarless hard candy, as needed. Encourage regularly scheduled dental visits because of the risk of dental caries and gum disease with dry mouth. Awarded 1.0 points out of 1.0 possible points. • 3.ID: 10242236828 The nurse administers atropine 0.5 mg IV push to a patient with sinus bradycardia. Which instruction should the nurse include in patient teaching? • Use ice chips to relieve dry mouth. Correct • Report blurred vision immediately. • Expect minor urinary incontinence. • Anticipate lethargy and sleepiness. Blockade of muscarinic receptors in salivary glands can inhibit salivation, leading to xerostomia (dry mouth). Ice chips are one means of managing dry mouth. The nurse instructs the patient to take ice chips rather than chewing gum or hard candy because the patient's heart rate has slowed enough to warrant the administration of atropine; until the patient's condition is stable, ice chips are a reasonable method of managing xerostomia. Blurred vision is an adverse effect of atropine; however, it does not necessitate immediate attention because its effect is usually mild. Atropine is likely to cause urinary retention and CNS excitation. Awarded 1.0 points out of 1.0 possible points. • 4.ID: 10242236807 A patient receives a prescription for oxybutynin (Ditropan) for the treatment of overactive bladder. Which instruction should the nurse include in patient teaching to help prevent adverse effects of therapy? • Manage increased salivation by drinking less. • Empty your bladder at least every 3 hours. • Treat diarrhea with diphenoxylate and atropine. • Avoid antihistamines without provider approval. Correct Oxybutynin is an anticholinergic agent that acts in a manner similar to that of atropine. For this reason, the nurse instructs the patient to avoid other medications, such as antihistamines, that exert anticholinergic effects. Oxybutynin is likely to cause constipation and xerostomia, so treatment for diarrhea is not necessary. Scheduled bladder emptying is unnecessary. Awarded 1.0 points out of 1.0 possible points. • 5.ID: 10242236823 A patient wants scopolamine (TransdermScop) for an upcoming vacation. Which additional medication taken by this patient makes scopolamine a poor choice for the suppression of motion sickness? • Alprazolam (Xanax) • Phenytoin (Dilantin) • Imipramine (Tofranil) Correct • Amantadine (Symmetrel) If the patient also takes imipramine, a tricyclic antidepressant, scopolamine is a poor choice, even though it is effective. This is because imipramine exerts a significant anticholinergic effect on muscarinic receptors; taking both medications concomitantly increases the risk of adverse effects of therapy. Phenytoin, alprazolam, and amantadine do not exert anticholinergic effects. Awarded 1.0 points out of 1.0 possible points. • 6.ID: 10242236815 The patient is taking an anticholinergic agent. What statement by the patient indicates that more education is needed? (Select all that apply.) • "I will need to increase my daily fiber intake." Correct • "I will need to increase the amount of water I drink." Correct • "I should decrease the amount of fruits and vegetables that I eat." • "I can take a fiber supplement to make sure I get enough fiber." Correct • "This drug has no adverse effects so I won't need to make any changes." Patients can maintain normal bowel patterns and avoid constipation by increasing fluid intake up to 8 glasses (preferably of water) a day; eating foods high in fiber, such as generous amounts of vegetables, fruits, and legumes; and taking a natural fiber supplement, if not contraindicated, such as a psyllium-based fiber product. Awarded 1.0 points out of 1.0 possible points. • 7.ID: 10242236817 After a patient takes an anticholinergic agent along with an atypical antipsychotic drug, the nurse must work to prevent life-threatening adverse effects. Which action is the nurse's priority in providing patient teaching to prevent this adverse effect? • Expectorate oral secretions. • Avoid sun and warm rooms. Correct • Avoid caffeinated beverages. • Drink additional fluids each day. The nurse instructs the patient to avoid the sun and warm environments because antipsychotic agents increase the risk of hyperthermia, and anticholinergic agents inhibit the ability to cool oneself through evaporative heat loss because they impair sweating. Either agent exposes the patient to a greater risk of hyperthermia and potentially life-threatening organ damage as a result of high body temperatures. Instructing the patient to drink fluids and limit caffeine are reasonable instructions; however, these measures are inadequate to overcome the heightened effect of the two drugs together. This patient is unlikely to have copious oral secretions. Awarded 1.0 points out of 1.0 possible points. • 8.ID: 10242236813 Which medication should be given as an antidote for atropine? • Dicyclomine • Physostigmine Correct • Narcan • Glycopyrrolate Overdose of atropine (usually from taking excessive Lomotil) is associated with flushing, dry skin and mucous membranes, mydriasis, altered mental status, and fever. Other serious effects include sinus tachycardia, urinary retention, hypertension, hallucinations, and cardiovascular collapse. The reversible anticholinesterase inhibitor physostigmine is the antidote for atropine overdose. Awarded 1.0 points out of 1.0 possible points. From <https://evolve.elsevier.com/Courses/155700_amiller946_1003/C-v5kn/CI-iw4d-m6qumpxi!reviewSubmittedAssessmentAttempt?attempt=17738928401> [Show More]
Last updated: 1 year ago
Preview 1 out of 171 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 07, 2019
Number of pages
171
Written in
Additional information
This document has been written for:
Uploaded
Oct 07, 2019
Downloads
0
Views
252