*NURSING > STUDY GUIDE > NURSING MISC MIDTERM study guide (All)
NURSING MISC MIDTERM study guide
Document Content and Description Below
NURSING MISC MIDTERM study guide MIDTERM STUDY GUIDE: PART-1 TOPICS Covered o Chalazions o Blepharitis o Conjunctivitis o Hand-foot-mouth syndrome o Strep pharyngitis o Kawasaki disease o Rhe... umatic fever o Milia o Port-wine stain/Nevus flammeus o Salmon patch o Café-au lait spot o Impetigo o Molluscum Contagiosum o Verruca Vulgaris o Herpetic Whitlow o Hemanginoma o Otitis media o Otitis Externa CHALAZIONS – Benign, chronic lipogranulomatous inflammation of the eyelid Causes – blockage of the meibomian cyst Risk – hordeolum or any condition which may impede flow through the meibomian gland. Also mite species that reside in lash follicles Assessment – PAINLESS, NOT INVOLVING LASHES Lid edema, or palpable mass Red or grey mass on the inner aspect of lid margin Prevention – good eye hygiene Treatment – warm, moist compresses 3x per day Antibiotics not indicated because chalazion is granulomatous condition, if secondarily infected consider SULFACETAMIDE, ERYTHROMYCIN Follow up – 2-4 weeks, if still present after 6 weeks follow up with ophthalmologistBLEPHARITIS – Inflamation/infection of the lid margins (chronic problem) 2 types – seborrheic (non ulcerative) : irritants (smoke, make up, chemicals) s&s – chronic inflammation of the eyelid, erythema, greasy scaling of anterior eyelid, loss of eyelashes, seborrhea dermatitis of eyebrows and scalp Ulcerative- infection with staphylococcus or streptococcus s&s – itching, tearing, recurrent styes, chalazia, photophobia, small ulceration at eyelid margin, broken or absent eyelashes ● the most frequent complaint is ongoing eye irritation and conjunctiva redness Treatment – clean with baby shampoo 2-4 times a day, warm compresses, lid massage (right after warm compress) For infected eyelids – antistaphyloccocal antibiotics BACITRACIN, ERYTHROMYCIN 0.05% for 1 week AND QUIONOLONE OINTMENTS For infection resistant to topical – TETRACYCLINE 250 MG PO X4 DOXYCYCLINE 100 MG PO X2 CONJUCTIVITIS – inflammation or irritation of conjuctiva Bacterial (PINK EYE) – in peds bacteria is the mosts common cause, contact lens, rubbing eyes, trauma, S&S – purulent exudate, initially unilateral, then bilateral Sensation of having foreign body in the eye is common Key findings – redness, yellow green, puru,ent discharge, crust and matted eyelids in am Self limiting 5-7 days. Eye drops – polytrim, erythromycin, tobramycin or cipro Improvement 2-4 days Most common organism H. influenza <7 Viral – adenovirus, coxsackie virus, herpes, molluscum S&S – profuse tearing, mucous discharge, burning, concurrent URI, enlarged or tender preauricular nose Antihistamines/decongestant Improvement, self limiting, 7-14 daysChlamydial – chlamydia trachomatis S&S – profuse exudate, associated with genitourinary symptoms, 1-2 weeks after birth Gonococcal – 2-4 days after birth, most concern can cause blidness PO azithromycin, doxycycline (tetracyclines increase photosensitivity, don’t use in pregnancy) Improvement 2-3 weeks Allergic – IgE mast cell reaction, environmental, cosmetics S&S – marked conjuctival edema, severe itching, tearing, sneezing Topical antihistamine or topical steroids Improvement 2-3 days Chemical –thimerosal, erythromycin, silver nitrate S&S conjuctival erythema, 30 minutes afer prophylactic antibiotics drops Avoid contact Can consider steroids Conjunctivitis never accompany vision changes Diagnostic studies: swap and scraping must be done, gram and Giemsa staining, ELISA, PCR testing, newborn < 2 weeks needs to be tested for gonorrhea Non –pharm – clean towels, change pillows, warm compress, no contacts, no eye make up – mascara Gonococcal conjunctivitis: newborn – give Ceftriaaxone IM once (don’t give if hyperbilirubinemia, Non-gonococcal – erythromycin 0.5% ointment Consider fluorescein staining if abrasion suspected CDC recommends prophylactic administration of antibiotic eye ointment (ERYTHROMYCIN) 1 hour after delivery Refer to ophthalmologist if herpes, hemorrhagic conjunctivitis or ulcerations present May return to work/school 24 hours after topical HAND-FOOT-AND-MOUTH DISEASE – HIGHLY CONTAGIOUS, viral illness clinical entity evidenced by fever, vesicular eruptions in the oropharynx that may ulcerate and a maculopapular rash involving hands and feet, the rash evolves to vesicles, especially on the dorsa of the hands and feet. Last 1 to 2 weeks. lesions appear on the buccal mucosa, palate, palms of hands, soles of feet and buttocsmost common cause – COXSACKIE A 16 common in children <5 S&S – low grade fever, malaise, abdominal pain, enlarged anterior cervical nodes or submandibular Oral – small red papules on the tongue and buccal mucosa, which will progress to ulcerative vesicles EXANTHEM (papulovesicular) – occurs 1-2 days after oral lesions Differential – herpangina, Stevens- Johnson syndrome Treatment – maintain hydration, cool liquids, avoid spicy food, rest Topical aluminum hydroxide/ magnesium hydroxide gel with diphenhydramine applied to painful lesions Topical anesthetics – Kank A, Orabase Resolution with 7 days STREP PHARYNGITIS – An acute inflammation of pharynx/tonsils, associated with crowding (school) rare in children <3 Viral – rhinovirus, adenovirus, parainfluenza, Epstein-barr virus Bacterial- group A beta hemolytic streptococcus Risk – family hx of rheumatic fever, day care S&S – sore throat, tonsillar exidate, malaise Strep: cervical adenopathy, fever >102F, no cough or nasal congestion, petechiae on soft palate, “Beefy Red” tonsils, “sandpaper” rash (nose, neck and torso), abdominal pain, headache Suggestive of viral : conjunctivitis, nasal congestion, cough, diarrhea When cough - almost always exclude Streptococcus Tests – rapid strep test CBC: WBC shift to left Monospot if mono suspected Treatment: gargling with salt water, change toothbrush, incubation period 2-5 days PCN – one IM or 10 days treatment PO First generation cephalosporins – 10 days treatment Azithromycin (if PCN allergy)Consult/referral – evidence of acute renal failure and reddish, tea collared urine (2-3 weeks post infection) No longer contagious after 24 hours on antibiotics, peak fever on days 2and 3, last 4-10 days KAWASAKI DISEASE (also known as mucocutaneous lymph nodesyndrome or infantile polyarteritis– an acute, febrile, immune-medicated, self-limited disease characterized by vasculitis. Leading cause of acquired heart disease in children 85% <5 years old most prevalent in Japan S&S Stage 1 -Acute (1-2 weeks) – high fever 103-105 for at least 5 days unresponsive to antibiotics, oral mucosa lesions may last 1-2 weeks, perineal rash, non-tender cervical adenopathy, painful rash and edema on feet Diagnosis requires fever for 5 days and 4 of these criteria: Edema or erythema of hands and feet, conjuctival injection (bilat), cervical adenopathy, rash (non-vesicular and polymorphous), exudative pharyngitis, diffuse oral arythema, STRAWBERRY TONGUE, crusting of lips and mouth Stage 2 - Subacute (2-8 weeks after onset) – without treatment: desquamation of palms, feet, periungual area, coronary artery aneurysm, joint aches and pains, acute MI may be seen, Pancardidis, diarrhea, jaundice, hepatosplenomagaly, platelet couns >10, 000 000 per mm Stage 3 – Convalescent – clinical signs have resolved, completed when all lab values are normal, however nail changes include Beau lines (deep transverse grooves across the nails) It is a fatal disease in small % of children who develop coronary artery problems despite treatment Differentials:Group A strep: scarlet fever Measles Epstein barr Toxic shock Rocky mountain spotted fever Steven-johnson syndrome Juvenile RA Tests: based on S&S and diff CBC, anemia, platelets 50% > 450 000 ESR >100 C-reactive protein EKG – prolonged PR intervals, decrease QRS Chest Xray – dilated heart, pleural effusion Pyuria/mild proteinuria Pharmacology IVIG single dose of 2g/kg for over 12 hours in the first 10 days Aspirin 80-100 mg/kg/d in 4 doses (Reye’s syndrome) Complications MI Development and rupture of coronary artery aneurysm may lead to emboli, HF, heart valve problems, dysrhythmias, myocarditis RHEUMATIC FEVER – An inflammatory disease that develops in 1-3% of children who have untreated infection with group A strep (GAS). This can affect the heart, blood vessels, joints , skin, CNS, connective tissues S&S – hx of pharyngitis 2-4 weeks prior onset of symptoms. Modified Jones criteria used to diagnose patient: 2 major, or 1 major and 2 minor criteria must be presented as evidenceMajor – carditis: 65% have with murmurs Polyarthritis:75% Chorea: 15% Erythema marginatum (macular rash with erythematous border Subcutaneous nodules Minor Fever 101-104F Artharlgias Elevated ESR, C-reactive protein Prolonged PR intervals on EKG Tests: throat cultures, negative antigen test ESR, C-reactive protein ASO tites EKG Chest xray CBC Treatment: first line PCN, if allergic Azithromycin Prednisone Aspirin AHA 2010 no longer recommends prophylaxis treatment for endocarditis in those with rheumatic fever PEDIATRIC BENIGN SKIN LESIONS MILIA (superficials cysts filled with keratin) – white papules found on the forehead, face, chin, and cheeks of infants, 1-2 mm in size, disappear few weeks after birth, may appear on palate – EPSTEIN’S PEARLS’SPORT-WINE STAIN (Nevus flammeus) – permanent defect that grows with child, if forehead and eyelids are involved, there is potential for multiple symptoms, includidng Sturge-Weber, Klippel-Trenaunay-Weber and Parkes Weber. Flat port wine stain- dark red to deep purple lesions present at birth, frequently found on face, do not fade with time SALMON PATCH – fade with time, usually by 5 or 6 years old, no treatment needed. Salmon patches (called a "stork bite" at the back of the neck or an "angel's kiss" between the eyes) are simple nests of blood vessels (probably caused by maternal hormones) that fade on their own after a few weeks or months. Occasionally stork bites never go away. CAFÉ AU LAIT SPOT – smooth, regular borders, Child > 5, 6 or more , >1.5 cm - possible Von Recklinghausen’s disease (90 -100%) *LEOPARD syndrome (Lentigines, Electrographic abnormalities, Ocular hypertelorism, Pulmonary stenosis, Abnormalities of genitalia, Retardation of growth, Deafness In child <5 years, 5 or more , 0.5 cm suggests neurofibromatosisSmaller 1-4 cm in diameter I axillae ( axillary freckling or Crow’s sign) rare but diagnostic sign of neurofibromatosis HEMANGIOMA – (dilation of capillaries) – raised, cavernous: appear bluish, located deep beneath the skin, NOT present at birth, appear within a few month and then disappear before the end of first decade of life. Capillary- STRAWBERRY hemangiomas : bright red vascular overgrowth, elevated, vary in size Possible steroids IMPETIGO – Superficial infection of the skin which begins as small superficial vesicles which rupture and form honey colored crust 2- 5 yearsBullous – is caused by Staphyloccocus aureus or group A strep Non – Bullous – MRSA 1-2 mm vesicles which rupture and form honey colored crusts, weeping shallow red ulcer common on mouth, face, nose, or site of insect bites fluid filled vesicles <0.5 cm appear as red macules and papules or pustules regional lymphadenopathy Treatment: good hygiene, hand washing Mupirocin (Bactroban) topical – 3x a day, don’t use <2 month Retapamulin (Altabax) - >9 months, apply thin film 2 x a day For large area- first generation cephalosporin, if unable to use PCN, consider macrolide Resolve within 7-10 days MOLLUSCUM CONTAGIOSUMMolluscum contagiosum is an infection caused by a poxvirus (molluscum contagiosum virus). The result of the infection is usually a benign, mild skin disease characterized by lesions (growths) that may appear anywhere on the body. Within 6-12 months, Molluscum contagiosum typically resolves without scarring but may take as long as 4 years. The lesions, known as Mollusca, are small, raised, and usually white, pink, or flesh-colored with a dimple or pit in the center. They often have a pearly appearance. They’re usually smooth and firm. In most people, the lesions range from about the size of a pinhead to as large as a pencil eraser (2 to 5 millimeters in diameter). They may become itchy, sore, red, and/or swollen. Mollusca may occur anywhere on the body including the face, neck, arms, legs, abdomen, and genital area, alone or in groups. The lesions are rarely found on the palms of the hands or the soles of the feet. The virus that causes molluscum spreads from direct person-to-person physical contact and through contaminated fomites. Fomites are inanimate objects that can become contaminated with virus; in the instance of molluscum contagiosum this can include linens such as clothing and towels, bathing sponges, pool equipment, and toys. Although the virus might be spread by sharing swimming pools, baths, saunas, or other wet and warm environments, this has not been proven. TREATMENT- Because molluscum contagiosum is self-limited in healthy individuals, treatment may be unnecessary. Nonetheless, issues such as lesion visibility, underlying atopic disease, and the desire to prevent transmission may prompt therapy. Other options for topical therapy include iodine and salicylic acid, potassium hydroxide, tretinoin, cantharidin VERRUCA VULGARIS - WART painless, benign skin tumors which are viral and can be transmitted by touch HPV 6 or 11 Common wart – rough surface, elevated, flesh-colored papules Avoid contact with wart exudate from self Treatment- paring and debridement of wart prior to any treatment Soak in warm water, occlude with waterproof tape for 1 week and leave open to air for 8-12 hours, then reocclude for 1 week Topical Duofil, Oclussal Hp must be applied up to 12 weeksCRYOTHERAPY with liquid nitrogen ( 5 second freeze until an ice ball forms Warts resistant to treatment - biopsy Herpetic Whitlow ● occurring on a finger or thumb, is a swollen, painful lesion with an erythematous base and ulceration resembling a paronychia. ● It occurs on fingers of thumb-sucking children with gingivostomatitis or adolescents with genital HSV infection. ● Lesions occur in children of all ages, are contagious as long as they are present, and have an incubation period of 2 to 12 days. ● Primary lesions usually occur before 5 years old, are more painful and extensive, and last longer. S&S - primary herpes, fever, malaise, sore throat, and decreased fluid intake - Deep-appearing vesicles on fingers Diagnostic Studies ● A Tzanck smear can be done on fluid from the lesions to identify epidermal giant cells, but does not distinguish HSV-1 from HSV-2. ● Viral cultures are the gold standard for definitive diagnosis. ● Direct fluorescent antibody (DFA) tests, enzyme-linked immunosorbent assay (ELISA) serology, and polymerase chain reaction (PCR) tests are usually only used with severe forms of HSV infection. Management ● Burrow solution compresses three times a day to alleviate discomfort ● Oral acyclovir 200 mg five times a day for 5 to 10 days may speed healing of herpetic whitlow ● Antibiotics for secondary bacterial (usually staphylococcal) infection: ● Offer supportive care, such as antipyretics, analgesics, hydration, and good oral hygiene ● Recurrent, frequent, and severe HSV infection may be treated with acyclovir prophylaxis for 6 month. Otitis media acute infecton of the middle ear. RSV and influenza 2 viruses most responsibleSX- rapid onsent of sx, ear pain, irritability, otorrhea, fever, bulging TM, decreased translucency of TM, erythema or amber is indicitve of effusion Risk factors- prematurity, unimmunized, breasteeding less than 6 months, overweight, parental smoking, feeding in supine positon TX- Tylenol or ibuprofen, topical analgesics (benzocaine/antpyrine otc drops), abx (amoxicillin or if amox in the last 30 days augmentn) watchful waitng for 48-72 hrs before prescribing OM w/ effusion- can occur afer AOM, viral illness, barotrauma, allergies, or anatomic abnormalites. SX- fullness in the hear, hearing loss, dizziness, popping TX-3 month watchful waitng Otitis externa (swimmers ear)- inflammaton of EAC that can involve pinna or TM. Result from damaged mechanical or chemical mechanisms, retained moisture acidic environment, chronic swimming pool, excessive cleaning of ears SX- pain with movement of tragus, swollen EAC making visualizaton of TM impossible, occasional regional lymphadenopathy, raised area of induraton that can be deep and diffuse or superfcial, red crusty or spreading lesions, thick otorrhea TX- ear drops with acetc acid or abx w/ or w/o cortcosteroid, should improve in 7 days. Do not use neomycin, polymyxin or hydrocortsone drops if TM is not intact (can damage cochlea) Quinolones are effectve against pseudomonas, aureus & pneumonia. Asthma chronic resp disease characterized by periods of coughing, wheezing, resp distress, and bronchospasm. Pathophysiology: result of immunohistopathology responses that produce shedding of airway epithelium and collagen deposits beneath the basement membrane. Factors that precipitate- viral/bacterial infectons, exposure to known irritants, GERD, tobacco smoke, environmental changes, exercise, AR/sinusits, drugs, food, allergies- dust, mites Sx- wheezing, contnuous/persistent cough, long expiratory phase, diminished breath sounds, signs of resp distress- tachypnea, retractons, nasal flaring, accessory muscles, apprehension, drowsiness, tachycardia, cyanosis of lips Dx- o2 sat, PFT- spirometry FEV1- amount of air expelled in 1 sec FVC >75%- normal 80-120%- normal 60-75 mild obstruct 70-79%- mild 50-59% moderate obstruct 50-69%- moderate <49% severe obstruct <50%- severe Levels of Severity pg 567 Mild -Wheezing @ end of expiraton or no wheezing -No or minimal intercostal retracton along posterior axillary line -slight prolongaton of expiratory phase -normal aeraton in al lung felds-can talk in sentences Moderate -Wheezing throughout expiraton -Intercostal retractons -Prolonged expiratory phase -Decreased breath sounds at the base Severe -Use of accessory muscles plus lower rib and suprasternal retractons, nasal flaring -inspir and expir wheezing or no wheezing heard w/ poor air exchange -suprasternal retractons w/ abd breathing -decreased breath sounds throughout base Impending resp arrest -Diminished breath sounds over entre lung feld -tring, inability to maintain resp -severely prolonged expiraton if breath sounds are heard -drowsy, confused See pg 572/573 for table and stepwise treatment. RSV Bronchiolitis RSVChildren less than 2 Highly contagious, spread through resp droplets Sx- wheezing, URI sx, worsening cough, rhinorrhea, irritability Increase WOB, prolonged expiraton, gruntng intercostal retracton, nasal flaring Tx- supportaive, hydraton nutriton Bronchiolits-pg 817- disease that causes inflammaton, necrosis, and edema of resp epithelial cells in lining of airways. Most commonly caused by respiratory syncytal virus (RSV). Common in children < 2. Contagious, spread thru droplet. Sc- URI sx of cough coryza, rhinorrhea, progresses over 3-7 days, gradual resp distress noisy raspy breathing, audible exp wheeze, low grade to mod fever, decrease in appette. Worsening fever with bacterial infecton. Tachypnea, retractons, exp wheeze, fne/coarse crackeles Dx- CXR if needed. Tx- supportve care, supplemental O2 Growth and development Birth -1 month -may lose 5-8% of birth wt but should regain in 10-14 days. >10% requires close monitoring. Nutriton 110 kcal/kg/day -sleep 16/24 hrs day -Reflexes: sucking, rootng, asymmetric tonic neck, Moro, grasp- should be + and symmetric. -Head lag-Should orient to light and sound, self soothe -Vision 8-12in from face 1-3month -Growth spurt 6-8 wks. More defned sleep paterns 15-16 hrs day. -Fine motor skills: atempt to grasp, visible head control, lifing head off bed when prone. -More social, imitate parents expressions- social smile. Can self soothe @ 3 mo-Extension, nondirected hand swipes, rootng reflex 4-5 months 4-6 months, infant doubles birth weight. -Social smile -Begins babbling -More consistent sleep w/ 5 feedings and 1 @ night. Grasping and holding botle. Roll, stronger head control with no head lag when pulled to sitng. -Hands to mouth, swing @ toys -Recognize parents meetng needs w/ breast or botle.. Sleep thru night w/o feeding. 6-8 months -Teething around 6 mo-8 mo, 1st illness can erupt at this tme. -Crawling. Growth may slow down with adding solids into diet. -Vocalizaton increases. “mama” “dada” -Use gestures (pointng, reaching). Stranger and separaton anxiety may appear. Understands cause and effect relatonship. -Introduce solid foods @ 6 mo. -Palmar grasp, pass things from hand to hand -Sits independently, rolls over, supports wt, bounces when held. 9-12 months -child proof house. -Separaton anxiety/stranger -Understands simple commands, imitaton, gives to on request, -Understands gestures like bye-bye/peek a boo -Feeds self/ Pincer grasp -Crawls and cruises around furniture, pull to stand, bears weight 12 mo: 15 mo -Can use sippy -Feeds self w/ spoon -Stands & walks independently -Drinks from cup -Points/clasps hands together -Follows commands -Knows @ least 3-4 words, knows name w/ gestures -Growth rate slows -knows 4-6 words *Health maintenance: check for anemia and lead18 mo. 24 mo (2yr) -Turns page of book -Runs, throws, kicks -Walk up steps -uses spoon, scribble -Knows 10-20 words -2-3 word sentences -Point @ body parts -up stairs w/ same -Pushes & pulls toys foot -Walks well independently -Temper, “No” -Toilet training, transitonal toy -Speech understood by family 36 mo (3yr) 42 mo (4 yr) -Full name, age, sex -Understand # -Speaks in complete sent. 3-5 words -Hops on foot -Knows 3 #’s and colors -Future & past tense -Copies a circle -Tells stories -Builds towers/rides tricycle -Copies a cross + -Imaginaton play -Litle help w/ dress -“Oedipal stage”- interested in opposite sex -Group play, does not like to take turns or share -Speech understood by stranger 60 mo (5 yr) 6 yr (Kindergarten) -Counts 10 or more things -Rides bike -Speaks clearly -Copies triangle -Puts shoes on and tes laces -Ties shoes -Prints own name -Bathes self -Can draw person w/ 6 body parts 7-11( Middle Childhood) -Succeed in school and interact w/ peer group -Thinks of future PURPLE cryingPeak of crying Unexpected Resists soothing Pain-like face Long lastng EveningFontanelles- 12 months- not palpapble. Anterior closes by 18-19 months Pediatric Physical Exam: Gestational and birth history (including maternal gestational history, smoking, and illicit drug use) Immunizations Hospitalizations Major illnesses or trauma (includes fractures, stitches, et cetera) Family history of disease Social: who the child lives with, members of the household in the home and ages, smoking in the home, electricity and clean water access, parents or guardians education and reading level, current school attending if appropriate, smoking,drug, or alcohol use in child, if appropriate, sexual activity in child, if appropriate, piercings or tattoos, if appropriate. -The American Academy of Pediatrics recommends well-child visits at 2 weeks and then at 2, 4, 6, 9, 12, 15, 18, and 24 months, annually up to age 6, and every 2 years from age 6 through adolescence 2. Puberty (pg 121) -Biologic process that ultmately leads to fertlity -Adolescence defnton: psychosocial & emotonal transiton from childhood to adulthood -onset of puberty untl sexual maturity Females: earlier than males -ovaries increase in size, breast budding btw 9-10, breast buds 6 months before pubic hair, menstrual cycle 10-.5-14.5 yrs. Decrease in lean body mass and increase body fat. Males: inital sign is testcular enlargement avg age 11. Release sperm age 13.5-14.5, elong and widening of penis, rapid height growth, hair growth, increase muscle mass and lose body fat. 3. Tanner Stages[Leik Book pg 427] Stage Girls Boys Pubic Hair I Prepuberty Prepuberty None II Breast bud Testes enlarge Rugae on scrotum Sparse, few straight III Breast & areola- 1 mound Penis lengthens Tests contnue to grow Darker, starts to curl IV Breast & areolasecondary mound Penis widens Thicker, curly, dark, coarse V Adult patern Adult patern Adult patern,spreads to inner thigh and lower abd Adolescence 1. Early Adolescence (11-14yrs) 2. Middle Adolescence (15-17) 3. Late Adolescence (18-21) 4. Growth and Development (birth-17) -infant loses 5-8% of birth wt but should regain in 2 wks., double birth wt by 6 mo and triple birth wt by 12 mo. -Infant Weight: 0-6 mo- 6-8 oz/wk and 1 inch per month 6-12 mo- 3-4 oz/wk and ½ inch per month - Head circumference measured tl 36 months , will increase by 12 cm frst 12 months 5. Vaccinatons Common side effects of vaccinations are as follows. Localized erythema, swelling, and pain, particularly with DTaP and Varicella vaccines Pain with injection Low grade fever (Note that activation of the immune system will cause low grade fever, which is desired in vaccinations.) Currently, there is not enough evidence to establish that antipyretic use prior to vaccination has benefit and it may harm antibody response Vaccine contraindications in childhood: Any secondary dose of a vaccine after severe allergic reaction to a prior vaccination. If the patient has severe combined immunodeficiency (SCID), they should not have rotavirus, Varicella, measles mumps rubella (MMR), zoster, or live influenza virus vaccines. Live influenza virus should also not be used in children with asthma, diabetes, or cardiac or renal disease. Influenza inactivated injectable vaccine (IIV) can be used. -Live viruses not given until 12 months (not effective r/t immature immune system) EX: MMR and varicella (Vaccine Breakdown) Pneumonic 2 B DR HIP, 4 DR HIP, B DR HIP IN 6, 12 MAD HPV, VERRY DIM at 4-6, Tada human Men, Hep B: 1. Birth 2. 1-2 mo 3. 6-18 mo.Rotavirus: 1. 2 mo 2. 4 mo 3. 6 mo Dtap: 1. 2 mo 2. 4 mo 3. 6 mo 4. 16-18 mo 5. 4-6 yrs Hib: 1. 2 mo 2. 4 mo 3. 6 mo 4. 12 mo Pneumococcal (PC4): 1. 2 mo 2. 4 mo 3. 6 mo 4. 12-15 mo Inactivated polio (IPV) 1. 2 mo 2. 4 mo 3. 6-18 mo 4. 4-6 yrs MMR 1. 12 mo 2. 4-6 yr Varicella 1. 12 mo 2. 4-6 yr ----Flu vaccine can be given @ 6 mo.MIDTERM STUDY GUIDE PART TWO: - TOPICS COVERED o Diarrhea ▪ Acute ● Cryptosporidium- ▪ Chronic o C-difff o EColi o Rotavirus o Salmonella o Pyloric stenosis o Intussusception o Celiac disease o Juvenile idiopathic arthritis o Osteomyelitis o Juvenile rheumatoid arthritis o Dysplasia of the hip o Transient Synovits of the hip o Legg-Calve’-Perthes Disease o Idopathic Scoliosis o Scoliosis o Osgood-Schlater o Week-4, Lesson:2 o Contraceptives o Testicular torsion o Wilms tumor o Week-4, lesson:3 o Iron-deficicency anemia o Febrile seizureDiarrhea - Do not give hypotonic fluids to prevent hyponatremia - Diarrhea o Contains 10-90 sodium, 10-80 potassium, and 40 HCO3 o S& S of dehydration:- lack of external jugular venous filling when supine, sunken fontanelle, oliguria, AMS, decreased cap refill. ▪ Total body water makes 50-75% of total body mass ▪ Highest in infants and young children Acute Diarrhea ● is a disruption of the normal intestinal net absorptive versus secretory mechanisms of fluids and electrolytes, resulting in excessive loss of fluid into the intestinal lumen. ● This can lead to dehydration, electrolyte imbalance, and in severe cases, death ● In children younger than 2 years old, this translates to a daily stool volume of more than 10 mL/kg (this definition excludes the normal breastfeeding stooling of five or six stools per day). ● In children older than 2 years old, diarrheal stooling is described as occurring four or more times in 24 hours. The duration can last up to 14 days. Epidemiology ● Females have higher rates of Campylobacter species infections and hemolytic uremic syndrome; ● otherwise the incidence of cases shows no gender preference. Nontyphoidal Salmonella, Shigella, Campylobacter, E. coli organisms (bacteria); rotavirus, norovirus, ● In the United States, those most vulnerable include Native Americans and Native Alaskans, ● The most common viral pathogens are noroviruses and rotavirus, followed by adenoviruses and astroviruses. ● Food-borne bacterial or parasitic diarrheal diseases are most commonly due to Salmonella and Campylobacter species, followed by Shigella, Cryptosporidium, E. coli O157:H7, Yersinia, Listeria, Vibrio (Vibrio cholerae and other species), and Cyclospora species. potentially serious infection in the upper intestine indicators • Food-borne illness suspected • Bloody diarrhea, weight loss, dehydration, severe abdominal pain, and fever • Diarrhea lasting several days with more than three stools per day • Neurologic involvement on physical examination Diagnostic Studies Diagnostic studies are ordered if the symptoms of more serious infection are present. • Stool examination & Stool cultures • Electrolytes • CBC Management The foundation of all treatment of acute diarrhea is fourfold: • Restore and maintain hydration and correct/maintain electrolyte and acid-base balance. - Oral rehydration with an oral electrolyte solution should be attempted when dehydration is assessed between 3% and 9%. • Antibiotics are recommended for acute diarrhea caused by G. lamblia, V. cholerae, and Shigella species and can be considered for infections caused by E. coli(if infection prolonged), Yersinia for those with sickle cell disease, and Salmonella in young infants with fever or positive blood culture findings . - Children with HIV at risk for acute diarrhea may benefit from cotrimoxazole and vitamin A- Flagyl (1st line for c-diff) Amoxicillin (salmonella, shigella), azithromycin, vanco & Cipro (ecoli, c-diff), ceftriaxone. • loperamide in children older than 3 years old is safe and decreases the duration and frequency of diarrhea - Children younger than 3 years old and those who are malnourished, those with moderate or severe dehydration, those who are systemically ill, or those who have bloody diarrhea should not be treated with this drug - Some over-the-counter products intended for diarrhea contain salicylates (e.g., Pepto-Bismol), and there is concern for Reye syndrome. Cryptosporidium- microscopic parasite that causes the diarrheal disease S&S: watery Diarrhea, stomach cramps or pain, dehydraton, Nausea, Vomitng, Fever, Weight loss Testng: stool sample TX: Nitazoxanide Chronic Diarrhea - Chronic diarrhea is defined as loose stools of less than 10 mL/kg/day in infants and less than 200 g/24 hours in older children. continuing diarrheal illness that started as acute diarrhea and is affecting growth. - TABLE 33-13 Common Causes of Chronic Diarrhea Seen in Children Age Conditions 0 to 6 months old • Carbohydrate malabsorption (acquired, congenital) (e.g., CMPI) • Protein hypersensitivity • Excessive intake of formula or other fluid (water, juice [especially those containing sorbitol/fructose], high-carbohydrate liquids) • Postenteritis • Infections • CF or other fat absorption conditions • Neuroblastoma (rare) • Immunodeficiency (e.g., HIV/AIDS and others) • Lymphangiectasia (rare) • Hirschsprung disease • Neonatal or infant enteropathies (rare) • Radiation treatments 7 to 24 months old First eight bulleted conditions listed above plus: • Chronic nonspecific diarrhea • Small-bowel overgrowth • Celiac disease • Graft-versus-host enteropathy • Autoimmune enteropathy • Radiation treatments>24 months old • Excessive intake of fruit juice/high-carbohydrate drinks • Infections • Small-bowel bacterial overgrowth • Celiac disease • Munchausen syndrome by proxy • Grant-versus-host enteropathy • Carbohydrate malabsorption • IBS • Adult-type hypolactasia • Encopresis • IBD (e.g., Crohn disease) • Excessive use of laxatives • Radiation treatments • Acquired lactase deficiency in older children, primarily of African, Asian, or Middle Eastern descent • Perforated appendix History and Physical • Occurrence of three or more watery stools per day for more than 2 weeks; 10 watery/runny stools per day that often contain undigested food particles is more typical of “toddler's diarrhea” • Presence of red flags: • Hematochezia or melena • Persistent fever • Weight loss or growth arrest • Anemia • Weight and height measurements; any weight loss • Growth retardation • Clubbing of fingers • Abdominal examination • Rectal examination (skin tags, impaction, tenderness) Diagnostic Studies • Stool: Culture, O&P (best done on three specimens collected on separate days), pH, reducing substances, occult blood, leukocytes, fat and fecal elastase (to evaluate for pancreatic insufficiency) (Normal stool pH greater than 5.5 indicates negative carbohydrate.) • CBC with differential, electrolytes, and albumin • UA and culture in young children The following are ordered as indicated by the history, physical examination, and consideration of differential diagnoses: • ESR, CRP • Hormonal studies to assess for secretory tumors (vasoactive intestinal peptide, gastrin, secretin, urine assay for 5- hydroxytryptamine [5-HT]) • Breath hydrogen test for lactose or sucrose intolerance (difficult to assess in infants) • Viral serologies, such as HIV or CMV • Sweat chloride test • Endoscopy, barium studies Management • Treat the underlying cause.• Chronic nonspecific diarrhea (toddler's diarrhea): Normalize the diet; remove offending foods and fluids; eliminate sorbitol and fructose-containing fluids; reduce fluid intake to no greater than 90 mL/kg/24 hours (give half of fluid as milk [whole or 2%]); increase fat to 35% to 40% of the diet; and increase fiber to bulk up stools. • Treat carbohydrate malabsorption by decreasing lactose or sucrose; add lactase or sacrosidase as indicated by particular carbohydrate intolerance. • Post-gastroenteritis malabsorption syndrome (evidenced in infants with weight loss and fat globules in the stool) can be given a predigested formula (e.g., Pregestimil or Alimentum), if tolerated, for 3 to 4 weeks (elemental formula can be used if those are not tolerated). Refer the following patients to a gastroenterologist: Newborns with diarrhea in first hours of life; patients with growth delay or failure or abnormal physical findings (anorexia, abdominal pain, chronic bloating, vomiting, or weakness); or those with severe illness. Pyloric stenosis Patho: - Pyloric stenosis is the narrowing of the lower portion of the stomach that leads into the small intestine. - The muscles of the stomach thicken, narrow the pylorus and prevent food from moving from the stomach to the intestine. - The environment and genetics play a role. sign and symptoms: - forceful projectile vomiting, olive shaped abdominal mass, visible peristalsis, weight loss, dehydration, fewer bowl movements, constipation, jaundice and lack of energy. diagnosis - included a firm olive mass in the mid abdomen - Blood tests, barium swallow and abdominal ultrasound Treatment - Pyloric stenosis is treated with IV fluids and then pyloromyotomy is performed. - This surgery uses an open or laparoscopic approach that opens up the tight muscle that caused the narrowing. - The outcome is great, there is only 1% chance for pyloric stenosis to occur Intussusception Pathophysiology ▪ Is a condition where the one section of the intestine folds into the another section of the intestine resulting in obstruction. The proximal bowel is trapped in the distal segment o The trapped bowel can exert pressure on the walls which squeezes the blood vessels and leads to ischemia and infarction Cause: ▪ Most cases are idiopathic, but many cases were associated with hyperplastic lymphoid tissue, suggesting an infectious cause, ▪ Predisposing factors include:- polyps, Meckel diverticulum, constipation, lymphomas, lipomas, parasites, rotavirus, adenovirus, and foreign bodies Risk factors: ▪ Infants between 6 and 12 months ▪ Male gender ▪ History of previous intussusception▪ History of intestinal malrotation ▪ Family history ▪ Prior viral illness Epidemiology - It is considered to be the most common cause of intestinal obstruction in children older than 3 months up to 6 years. ▪ In the US, intussusception occurs in 18 to 56 per 100,000 infants ▪ It most commonly occurs in infants between 5 and 10 months of age. ▪ 2/3 of the intussusception happens in infants under one year of age, but it even occur in adults Signs and symptoms ▪ Classical triad symptoms include intermittent/ colicky abdominal pain, vomiting, and bloody mucous stools characterized as “currant jelly”) ▪ Emesis is usually nonbilious. ▪ Other symptoms include lethargy, history of URI, fever, sausage like mass in the right upper quadrant or in right lower when abdomen is empty, tender and distended abdomen Diagnostic Studies ▪ The most accurate diagnostic tool recommended is an abdominal ultrasound. ▪ It shows “bull’s eye” which is telescoped intestine on end. ▪ Other diagnostic tools such as x-ray , CT, and Air contrast enema can also be used Management ▪ Intussuception can develop suddenly putting the infant at a potential risk for developing ischemia and possible infection and even sepsis. Therefore, rapid treatment is necessary. ▪ MEDICAL EMERGENCY ▪ Rehydration and correction of electrolyte imbalance is very important. ▪ After correction of dehydration and electrolyte imbalance, the gold standard is radiologic reduction via air contrast enema under fluoroscopy ▪ The Outcome of air or contrast enema reduction is 100% cure, but 10% recurrence has been identified. ▪ Surgical reduction is also associated with a recurrence rate of 2 to 5%. Celiac disease ● Malabsorption syndromes can be caused by many different genetic, congenital, and acquired conditions and usually lead to an initial decrease in weight followed by a deceleration in height velocity. ● Celiac disease is an immune-mediated systemic disorder triggered by dietary exposure to wheat gluten and related proteins in barley and rye. ● It is characterized by the presence of a variable combination of gluten-dependent clinical manifestations, celiac disease–specific antibodies, HLA-DQ2.5 or HLA-DQ8 haplotypes, and enteropathy. ● Celiac disease has a worldwide distribution with overall prevalence of 1% Risk factors - Demographic changes - Increased gluten exposure - infants born by cesarean section; - The most typical presentation occurs between 6 months and 2 years old.Parent reported gastroenteritis occurring at the time gluten was introduced into the child's diet does not appear to be associated with celiac disease. Clinical Findings • Chronic or intermittent diarrhea, persistent or unexplained GI symptoms (e.g., nausea and vomiting), sudden or unexpected weight loss, and prolonged fatigue. • Delayed puberty can coexist with malabsorption, Impaired growth, FTT, unexplained iron deficiency anemia, abdominal distention, bloating or cramping pain • May have no symptoms at all despite evidence of small bowel changes; ● maintain a high suspicion for celiac disease in children with metabolic bone disease (such as rickets or osteomalacia), low-trauma fractures, or those with dental enamel defects. ● An estimated 85% to 90% of individuals with celiac disease are undiagnosed • Pallor, fatigue, hair and dermatologic abnormalities, digital clubbing, dizziness, cheilosis, glossitis, peripheral neuropathy (symptoms of vitamin deficiency seen with malabsorption), Skinfold thickness and lean body mass Diagnostic Studies • See chronic diarrhea tests Specific Tests for Celiac Disease • Serologic testing should be done if there is clinical suspicion of celiac disease, the child has an associated disorder, or there is a first-degree relative with celiac disease. Gluten should be eaten in more than one meal every day for 6 weeks prior to testing. ● Recommended serologic tests include IgA tissue transglutaminase antibody (tTGA) and IgA endomysial antibody (EMA) because of their high sensitivity and specificity ● EMA is more expensive and less accurate in children younger than 2 years old • Home blood testing is not recommended ● If serologic testing is positive, refer for endoscopy with biopsy for a definitive diagnosis, although colonoscopy may not be necessary if the tTGA level is greater than 100 units/mL • Careful follow-up of growth parameters, tTGA testing after 6 months of gluten-free diet (GFD), and then yearly • Bone density testing (bone problems may be first symptom of celiac disease). Management Celiac Disease • A strict GFD for life is currently the only effective treatment for celiac disease. ● The standard for being gluten-free is a limit of 20 ppm of gluten ● Adding pure oats to a GFD can improve palatability and increase fiber and vitamin B intake without causing a systemic or autoantibody response Complications and Prognosis ● Growth failure is the primary complication of celiac disease. ● risk for fractures and osteoporosis (due to reduced bone mineral density), lymphoma, autoimmune diseases (e.g., type 1 diabetes, thyroid disorders), primary biliary cirrhosis, and primary sclerosing cholangitis. ● Sensory peripheral neuropathy may be related to gluten ● Celiac crisis consisting of abdominal distention, explosive watery diarrhea, dehydration with hypoproteinemia, electrolyte imbalance, hypotensive shock, and lethargy, although rare, can be the first indication of celiac disease. Diarrheal Illnesses Due to Common Bacterial or Vial Pathogens1. Rotavirus Incubation Period: 1 to 3 days; prevalent during cooler months in temperate climates Signs and Symptoms: Acute-onset fever, vomiting, and watery diarrhea occur 2 to 4 days later in children <5 years old, especially those between 3 to 24 months old Duration of illness: 3 to 8 days Route of Transmission: Fecal-oral; viable on inanimate objects; rarely contaminated water or food Laboratory Testing: Enzyme immunoassay and latex agglutination assays for group A rotavirus antigen; virus can be found by electron microscopy and specific nucleic acid amplification methods. Treatment and Complications: Supportive care: May need to correct dehydration and electrolyte imbalances. Oral IG has been used in those immunocompromised. Preventive care: Rotavirus vaccine; hygiene and diapering precautions in day care facilities. 2. Salmonella Incubation Period: 1 to 3 days Signs and Symptoms: Diarrhea, fever, abdominal cramps, rebound tenderness, vomiting. S. typhi and S. paratyphi produce typhoid with insidious onset characterized by fever, headache, constipation, malaise, chills, and myalgia; diarrhea is uncommon, and vomiting is not usually severe Duration of illness: 4 to 7 days Route of Transmission: Contaminated eggs, poultry, unpasteurized milk or juice, cheese, contaminated raw fruits and vegetables (alfalfa sprouts, melons) S. typhi epidemics are often related to fecal contamination of water supplies or street-vended foods Laboratory Testing: Routine stool cultures; positive leukocytes and gross blood. CBC: WBC can be slightly ↑ with left shift, ↓, or normal. Treatment and Complications: Supportive care: Only consider antibiotics (other than for S. typhi or S. paratyphi) for infants <3 months old, those with chronic GI disease, malignant neoplasm, hemoglobinopathies, HIV, other immunosuppressive illnesses or therapies.If indicated, consider ampicillin or amoxicillin, azithromycin, or TMP-SMX; if resistance shown to any of those, use IM ceftriaxone, cefotaxime; or azithromycin or quinolones. A vaccine exists for S. typhi in certain cases. 3. Clostridium difficile Incubation Period: Unknown Signs and Symptoms: Variety of symptoms and severity are seen: mild to explosive diarrhea, bloody stools, abdominal pain, fever, nausea, vomiting Mild to moderate illness is characterized by watery diarrhea, low-grade fever, and mild abdominal pain Duration of illness: During or after several weeks of antibiotic use; can occur without being associated with such treatment Route pf Transmission: Acquired from the environment or from stool of other colonized or infected people by the fecal-oral route Laboratory Testing: Stool cultures; enzyme immunoassay for toxin A, or A and B; positive gross blood, leukocytes; CBC: ↑ WBCs; ESR normal Treatment and Cmoplications: Discontinue current antibiotic (any antibiotic, but notably ampicillin, clindamycin, second- and third-generation cephalosporins). Fluids and electrolyte replacement are usually sufficient. If antibiotic is still needed or illness is severe, treat with oral metronidazole (drug of choice in children) or vancomycin for 7 to 10 days. Supplement with probiotics. Lactobacillus GG, Saccharomyces boulardii are recommended (Jones, 2010; Shane, 2010). Complications include pseudomembranous colitis, toxic megacolon, colonic perforation, relapse, intractable proctitis, death in debilitated children 4. Enterotoxigenic E. coli(ETEC) and enteroadherent E. coli (frequent cause of traveler's diarrhea) Incubation Period: 1 to 3 days Signs and Symptoms: Watery diarrhea, abdominal cramps, some vomiting; often cause of mild traveler's diarrhea Duration of illness: 3 to >7 days Route of Transmission: Water or food contaminated with human feces Laboratory Testing: Stool culture. ETEC requires special laboratory techniques for identification. If suspected, must request specific testing.Treatment and Cmoplications: Supportive care: Antibiotics are rarely needed except in severe cases. Recommended antibiotics include TMP-SMX and quinolones. See www.cdc.gov/travel. 5. Enterohemorrhagic Escherichia coli(EHEC) including E. coli O157:H7 and other Shiga toxin– producing E. coli(STEC) Incubation Period: 1 to 8 days Signs and Symptoms: Severe diarrhea that is often bloody, abdominal pain and vomiting Usually little or no fever, More common in children <4 years old Duration of illness: 5 to 10 days Route of Transmission: Undercooked beef, especially hamburger, unpasteurized milk and juice, raw fruits, vegetables (e.g., sprouts, spinach, lettuce), salami (rarely) Contaminated water; petting zoos Laboratory Testing: Stool culture; E. coli O157:H7 requires special media to grow. If E. coliO157:H7 is suspected, specific testing must be requested. Shiga toxin testing may be done using commercial kits; positive isolates should be forwarded to public health laboratories for confirmation and serotyping. Stool grossly positive for blood. Treatment and Cmoplications: Supportive care: Monitor CBC, platelets, and kidney function closely. E. coli O157:H7 infection is also associated with HUS, which can cause lifelong complications. Studies indicate that antibiotics may promote the development of HUS.Juvenile idiopathic arthritis and osteomyelitis Condition Age pain Historical Findings Clinical Findings Causative Factors Management Juvenile arthritis (JA) Child to 16 yearo f age + Fever, rashes, ↑ WBCs; some iritis; joint stiffness and swelling; S&S >3 months Mono-/polyarticul ar arthropathy; + ANA (25% to 88%); ↑ ESR in moderate/sev ere JA Unknown; genetic (HLA) or environmen tal Treat with NSAIDs initially; may need sulfasalazine , methotrexate ; corticosteroi ds; joint replacements when older Acute Hematogenou s osteomyelitis Toddler, child, adolescen t + Varied: malaise, low-grade to high fever; may have severe constitution al symptoms; toxicity Refusal to walk or move limb; point tenderness; limp; 7 to 10 days to see radiographic bony changes; 25% ↑ WBCs; ↑ CRP S.aureus Organism (Likely) Appropriate antibiotic coverage (generally 7 days, IV; 4 to 6 weeks total or until ESR normal) Juvenile Idiopathic Arthritis ● Also as juvenile rheumatoid arthritis (JRA), now encompasses several disorders that have a common feature of arthritis. ● The diagnosis of JIA requires a persistent arthritis for more than 6 weeks in a pediatric patient younger than 16 years old. TABLE 25-1 Juvenile Idiopathic Arthritis Subtypes and Clinical Joint Characteristics Juvenile Idiopathic Arthritis Subtype Clinical Joint Characteristics Oligoarticular Four or less joints with persistent disease never having more thanfour-joint involvement and extended disease progressing to more than four joints within the first 6 months Polyarticular (RF negative) Five or more joints with symmetrical involvement Polyarticular (RF positive) Symmetric involvement of both small and large joints with erosive joint disease Systemic Either polyarticular or oligoarticular disease Enthesitis-related arthritis Weight-bearing joints involved especially hip and intertarsal joints and a history of back pain, which is inflammatory in nature or sacroiliac joint involvement Psoriatic arthritis Asymmetric or symmetric small or large joints Undifferentiated Most forms of JIA have unclear ● environmentally induced in genetically predisposed individual. ● Human leukocytic antigen (HLA) class I and II alleles have been associated with JIA ● An environmental trigger, such as infection or trauma, is also important in the pathogenetic process in JIA. Systemic juvenile idiopathic arthritis (SJIA) ● does not have HLA gene association, ● may be the result of an autoinflammatory response from the innate immune system. ● The female to male ratio in systemic onset is equal Oligoarticular and rheumatoid factor (RF)-positive polyarticular JIA ● there is autoimmunity with involvement of the adaptive immune system ● The presence of positive ANAs and RF is associated with HLA genes. ● Approximately 1 in 1000 children are affected with oligoarticular JIA, the most common arthritic subtype. ● The rate of JIA is significantly higher in girls than in boys, typically in oligoarticular and pauciarticular JIA.● The approximate percentage of occurrence and age breakdown for each of the subtypes follows: systemic (10%) occurs at any age; polyarticular (40%) has a late (6 to 12 years old) or early childhood (1 to 4 years old) onset; and oligoarticular (50%) has a late or early onset. ● Adolescents tend to have more RF-positive disease Clinical Findings • Pain—generally a mild to moderate aching • Joint stiffness—worse in the morning and after rest; arthralgia may occur during the day • Joint effusion and warmth, tenderness • Non-migratory monoarticular or polyarticular involvement of large or proximal interphalangeal joints for more than 3 months • Systemic manifestations—anorexia, fatigue fever, salmon-colored rashes, leukocytosis, serositis, lymphadenopathy, and rheumatoid nodules, uveitis - growth failure, or leg-length discrepancy if unilateral. • Loss of joint range of motion and function; child typically holds the affected joints in slight flexion and may walk with limp Diagnostic Studies - JIA is a diagnosis of exclusion. - physical findings and history of arthritis lasting for 6 weeks or longer. o polyarticular and systemic-onset typically have elevated acute-phase reactants and anemia of chronic disease. o positive RF occurs in less than 10% of children with JIA and rarely in those with SJIA. o ANA may be present in up to 50% of children with oligoarticular disease o The anti-CCP antibody test is highly specific in polyarticular JIA o Useful laboratory tests include a complete blood count (CBC) (to exclude leukemia); ESR, CRP, Lyme titers, and liver function tests. ▪ The results may reveal lymphopenia, anemia, elevated transaminases, and hypoalbuminemia; ▪ however, laboratory studies may be normal in these children. o Imaging studies (MRI) can help in managing joint pathologic conditions. o Analysis of synovial fluid is not helpful in the diagnosis of JIA. Management o Ophthalmology referral and evaluation is critical in a child with a positive ANA (Uveitis) o The main treatment goals are to suppress inflammation, preserve and maximize joint function, prevent joint deformities, and prevent blindness. o there is no curative treatment o Aggressive early treatment to induce a remission is a key consideration in JIA management in order to prevent deformity and improve o Aspirin therapy has largely been replaced with the use of nonsteroidal anti-inflammatory drugs (NSAIDs). o NSAIDs: Children with oligoarthritis generally respond well to NSAIDs o Ibuprofen: 30 to 40 mg/kg/day three to four divided doses (maximum single dose is 800 mg; maximum daily dose 2400 mg/day) o Naproxen, Indomethacin, Celecoxib (Older than 2 years old and adolescents) o Oral, parenteral, intraarticular corticosteroids:o Disease-modifying antirheumatic drugs (DMARDs o Nonbiologic DMARD treatment: methotrexate, sulfasalazine, leflunomide (managed by pediatric rheumatologist) o Physical therapy—range of motion muscle-strengthening exercises and heat. Rest and splinting are used if indicated. passive, active, and resistive exercises o Ophthalmologic follow-up every 3 months for 4 years (even if it has resolved) for all ANApositive JIA children. The disease process of JIA wanes with age and completely subsides in 85% of children; however, systemic onset, a positive RF, poor response to therapy, and the radiologic evidence of erosion are associated with a poor prognosis. Onset of disease in the teenage years is related to progression to adult rheumatoid disease. Dysplasia of the hip ● The femoral head and the acetabulum are in improper alignment and/or grow abnormally. ● Includes:- dysplastic, subluxated, dislocatable, and dislocated hips. ● Dysplasia is characterized by a shallow more vertical acetabular socket with an immature hip/acetabulum. ● Dysplasia may be diagnosed many years after the newborn period. Risk factors o hormonal effect of maternal estrogen and relaxin that are released near delivery and produce a temporary laxity of the hip joint. o Mechanical factors in utero o This is seen with first pregnancy, oligohydramnios, and breech presentation, 4x more in girls, positive family history (genetic risk factors) increases o Increased in cultures swaddle infants in extended position or cradleboard placement o In the newborn, the left hip is most often involved because this hip typically is the one in a forced adduction position against the mother's sacrum. o 60 to 80% of abnormal hips of newborns resolves by 2 to 8 weeks (self-limiting, but close observation) Clinical Findings. In the older infant, 6 to 18 months old: • Limited abduction of the affected hip and shortening of the thigh is a reliable sign ● Normal abduction with comfort is 70 to 80 degrees bilaterally. ● Limited abduction less than 60 degrees of abduction or unequal abduction ● Positive Galeazzi sign ● Asymmetry of inguinal or gluteal folds- NOT thigh-fold ● unequal leg lengths, shorter on the affected side. In the ambulatory child who was not diagnosed earlier or was not corrected, the following might also be noted: • Short leg with toe walking on the affected side • Positive Trendelenburg sign • Marked lordosis or toe walking • Painless limping or waddling gait with child leaning to the affected side If the hips are dislocated bilaterally, asymmetries are not observed. ● Limited abduction is the primary indicator in this situation ● A waddling gait may also be noted.Diagnostic Studies ● Screening tests are serial physical examinations of the hip and lower extremities. ● Barlow and Ortolani tests are used to screen for DDH in neonates. o Less reliable after 2-3 months ● Klisic and Galeazzi tests are used to screen older infants. ● Routine ultrasonography is not recommended; however, an ultrasound should be obtained if there is a high index of suspicion of dysplasia based on a positive clinical examination. ● Ultrasound recommended for infants after 4 weeks of age. (before 4 weeks false-positive results) ● Radiologic evaluation of the newborn to detect and evaluate DDH is recommended once the proximal epiphysis ossifies, usually by 4 to 6 months o AP and lateral Lauenstein (frog-leg) position radiographs of the pelvis are indicated. Management - The goal of management is to restore the articulation of the femur within the acetabulum. - Many newborns with positive screening tests and abnormal hips resolve without intervention; however, prompt referral to an orthopedist is important. ● Early phase is a Pavlik harness. - The harness is worn 24 hours a day, except for bathing. - seen weekly to ensure it fits properly - Ultrasonography can be performed while the Pavlik harness is worn to assess hip reduction and acetabular development. - The length of time the harness is worn depends on the age of the child, when it was applied, and whether or not reduction is successful. - Generally the harness is worn full time for 3 to 6 weeks and then may be required only during waking hours for decreasing periods of time. ● The 6- to 18-month-old infant with a dislocated hip is likely to require either closed manipulation or open reduction. o Preoperative traction, adductor tenotomy, and gentle reduction are especially helpful in preventing osteonecrosis of the femoral head. o After the closed or open reduction, a hip spica cast is applied o Annual or biennial follow-up including radiographs o Screening of all neonates and infants should include full hip abduction; examination for unequal inguinal and gluteal folds and unequal leg lengths; and Barlow, Ortolani, and Galeazzi maneuvers at every examination. o The Ortolani test should only be used in the first 2 to 3 months of age. Transient Synovits of the hip pg 1079 Self-limited inflamm disorder of the hip, common in boys, r/o septc arthrits Cause-inflammatory rx, URI, unknown Sx-mild to mod fever, irritability, limited hip moton, ESR < 25 mm/h3-8 year olds Tx- rest Legg-Calve’-Perthes Disease self-limitng disease of femoral head comprising of necrosis, collapse, repair and remodeling -Cause-familial, breech birth, prior trauma Sx- acute or chronic onset, pain in hip, groin, knee stffness (male). + trendelenburg, shortening, decreased abducton, internal rotaton, hip extension, + radiographs but not early Tx- BR, tracton, PT, brace surgery may be needed Idopathic Scoliosis pg 1057 Occurs in adolescence, mild curve, sexes -lateral curve of the spine in the frontal plan Dx- Cobb method that measures angle btw superior and inferior end vertebrae Cause-usually unknown that’s why termed idiopathic, may have familial or genetc---most common type Infantle 0-3 Juvenile 3-10 Adolescent 11 and up Generally painless and insidious onset. Adam’s forward bend test---unequal shoulder height, scapula prominences, waist angles, rib heights. Dx-AP and lateral spine, cobb angle, MRI for underlying cause Tx-goal is to delay spinal fusion, observaton for less than 20 degree, bracing or surgery for larger curve Scoliosis Osgood-Schlater pg 1068 -caused by micotrauma in deep fbers of patellar tendor @ inserton to tbial tuberosity Dx- clinical h & p Hx- recent physical actvity, pain increase during and immed afer, running/jumping/kneeling/squatng, and up and down stairs exacerbates Physical exam- pain reproduced by extending need against resistance, stressing quad, squatng with knee full flexed, focal swelling, heat and point tenderness, full ROM of knee Tx-self-limitng, modifying actvity, ice/cold, stretching, NSAIDs, neoprene sleeveWEEK-4: LESSON-2 Endocrine malfunction can lead to delays in growth, short stature, significant illness, developmental or cognitive impairment or delays, and even death ● At birth: Routine state newborn screenings should test for endocrine diseases like congenital hypothyroidism and congenital adrenal hyperplasia (CAH). ● At each well child exam: At each well-child exam, the child should be monitored appropriately for height and weight, HC, growth velocity, and rapid changes in weight loss or gain. These are important screenings for endocrine disorders. ● well-child assessment should include tanner staging of breasts and genitals, along with pubic and axillary hair development. o Height measured standing after age 2 if possible o Infants should only be measured with a dry diaper on and supine length must be accurate and possibly measured more than once. ● Endocrine system to function properly not only must the endocrine organs themselves be working, but also the neurologic and central nervous systems. ● There are seven classic endocrine glands; the pituitary, thyroid, parathyroid, testes, ovaries, adrenal (cortex and medulla), and endocrine pancreas. ● Hormones released from an endocrine gland either work directly on the gland itself, or travel through circulation to target tissue and cells where they exert action on the cell or cell nucleus directly. ● The hypothalamus and pituitary gland of the brain are critical to this process because the hypothalamus stimulates the pituitary gland action. Delayed Puberty: Males • No secondary sexual characteristics by 14 years • > 5 years since first signs of puberty to Tanner V • Causes: constitutional growth delay, primary or secondary gonadal failure, malnutrition or disordered eating, Klinefelter’s syndrome Delayed Puberty: Females • Evaluated if no pubertal signs by 13, or no menarche by 16 • Failure to complete development Tanner V within 4 years of onset of secondary sex characteristics • Most common cause: constitutional growth delay (delayed skeletal muscle growth) • Other causes: Turner’s Syndrome, extreme athleticism, disordered eating, primary or secondary gonadal failure. Precocious Puberty - Pubertal development prior to normal age of onset GIRLS: • Before 8 years old in Caucasian, 7 years old African-American and Latino • Pubertal onset advanced in obesity • Central: Breast development, followed by pubic hair growth, menarche *Note that girls who are obese can have breast bud development without other signs of puberty. BOYS:• Secondary sexual characteristics prior to age 9 BOTH Bone age on X-ray will be older than chronological age. • Treatment in both is medications to stop stimulation of their hypothalamus-pituitary-adrenal axis. Contraceptives Epidemiology ● Unintended pregnancy rates are highest among poor and low-income women, women aged 18–24, cohabiting women and minority women • Rates tend to be lowest among higher-income women, white women, college graduates and married women. • highest rate of unintended pregnancy was seen among women 20 to 24 years of age, followed by women 18 to 19 and women 25 to 29 years of age. • IUCs, implants, and sterilization are considered a “top-tier” method because less than 1 pregnancy per 100 women occurs in a year with the use of these methods. • These methods are more effective in preventing pregnancy than the second tier methods, not due to their mechanisms of action, but because they are easier to use properly. Once the top tier methods are initiated, they require little additional action to provide highly effective contraception. Sterilization • Vasectomy is an outpatient surgical procedure for male sterilization. - The failure rate of vasectomy is very low—0.10 % with perfect use and 0.15 % with typical use. - Vasectomy is cheaper, safer, and more effective than female sterilization • Traditional tubal occlusion o A surgical procedure (either by minilaparotomy or laparoscopy). o Requires a small abdominal incision and general or regional anesthesia.o Occlusion techniques include tying (ligating) and blocking with mechanical devices, such as clips or rings and cauterizing. o Typical failure rates are less than 1%. • Newer tubal occlusion: transcervical sterilization (nonsurgical methods)Essure: o Employ micro-inserts that expand and occlude the fallopian tubes as tissue grows in and around the insert. o Involve a half-hour procedure, using a hysteroscopic technique. o Procedure is performed in an outpatient setting, under local anesthesia. o Candidates: o Women who want permanent birth control and are willing to use another birth control method for the first 3 months after the procedure, and who have a medical condition that precludes general anesthesia. o For women with medical conditions such as heart disease and obesity, microinsert procedure may be safer, partly because of routine use of local anesthesia. Some of these women are ineligible for conventional tubal sterilization. Intrauterine Contraception • There are two general categories of Intrauterine devices; o one containing no hormone o the other containing a small amount of levonorgestrel • The Cooper T (Paraguard) IUD is a small T-shaped device made of polyethylene. o The device has two flexible arms that fold down for insertion and expand to form a T shape when released inside the uterus. o The vertical stem of the device is wound with fine copper wire, and the two horizontal arms also have a sleeve of cooper. o The Copper-T IUD is approved for 10 years of use; however, efficacy lasts 12 years or more. • LNG IUS: o Two products with 52 mg (Mirena by Bayer and Liletta by Activis); o Mirena® Approved for up to 5 years of use; data demonstrate 7-year efficacy o Liletta™ Approved for 3 years of use Bayer has two newer products: Skyla and Kyleena • Skyla Contains 13.5 mg of LNG, and Kyleena has 17.5 mg LNG o Smaller size and lower dose than Mirena, aimed at greater acceptability among younger, nulliparous women o Nulliparous women may have smaller uterine cavities and tighter cervical os than their parous counterparts. o Horizontal length = 28 mm; vertical length = 30 mm Vs. Mirena which measures 32 mm in both directions o Skyla Approved for up to 3 years of use and Kyleena for 5 years Candidates: ● Women who are at low risk for STIs ● Women who are looking for a convenient method ● Women who are considering sterilization ● However, appropriate candidates include all women of reproductive ages who are seeking a longterm, highly effective contraceptive. TYPES OF IUC o The Copper T IUD:- o who don’t want hormonal contraception o women who want regular periods• women seeking a form of emergency contraception. o Can be inserted up to 5 days after unprotected intercourse to prevent pregnancy o More effective than use of emergency contraception pills. Insertion of a copper T IUD can reduce the risk of pregnancy after unprotected intercourse by more than 99%. ECPs have the potential to reduce unintended pregnancy by 75%-89%. o The LNG IUS should NOT be used for emergency contraception • The LNG IUS devices prevent fertilization rather than disrupt implantation (a common misconception). o The LNG 52 IUS o women who wish to reduce their menstrual flow or who experience dysmenorrhea or dysfunctional uterine bleeding. o The LNG 17.5 and 13.5 IUS ( smaller) o women who wish to have a lower-dose LNG IUD or o have smaller uterine cavities ● IUC does not increase the risk of ectopic pregnancy or PID; rather, it decreases the risk of both ectopic and intrauterine pregnancy (more effective). ● Clinical guidelines state that removal of the IUD is not necessary in STI OR PID unless symptoms fail to improve within 72 hours of the start of treatment. o An IUD can be started immediately postpartum or post-abortion. Side effects and complications ● Menstrual changes: the Copper T IUD can increase the duration and amount of menstrual flow and menstrual cramping. ● Expulsion is rare, occurring in only 5% of users, especially first three months after insertion ● Uterine perforation is a rare complication of IUC (at insertion) ● possible increased risk of PID during early postinsertion period in women with cervical infections. ● During the first 3-6 months of LNG IUS use, bleeding may be irregular and the number of days with bleeding or spotting may be increased from baseline. o Thereafter, bleeding generally decreases to the point that about 50% of users have amenorrhea at 12 months after insertion. Absolute contraindications o Current breast cancer is rated Category 4 (risks outweigh the benefits), However, breast cancer in the past; no evidence of disease for 5 years is a Category 3. o In addition to these conditions, the following conditions are Category 3: o Ischemic heart disease or stroke (current or history of)—for continuing method (i.e., if heart disease worsens in a woman who is already using the contraceptive implant) o SLE (positive for antiphospholipid antibodies or status unknown) o Migraine with aura—for continuing method (i.e., if migraines worsen in a woman who is already using the contraceptive implant) o Unexplained vaginal bleeding prior to evaluation o Breast cancer in the past; no evidence of disease for 5 years o Severe cirrhosis o Malignant liver tumor (Hepatocellular adenoma) IMPLANT : NEXPLANON • It contains 68 mg of the synthetic progestin etonogestrel. • The implant continuously releases etonogestrel over 3 years. It is for subdermal use only andis placed in the upper arm.. • Mechanism of Action: o •The contraceptive effect of NEXPLANON® is primarily achieved by suppression of ovulation. o In addition to inhibiting ovulation, the implant increases viscosity of the cervical mucus, which helps inhibit sperm migration. o Finally the implant alters in the endometrium by decreasing its thickness. • Back up method for 4 days, if insertion is not during the first five days of menses. • Inserted at the inner side of the non-dominant arm about 8-10 cm (3-4 inches) above the medial epicondyle. Insertion is subdermal. Advantages: o Rapid reversibility. After implant is removed, most women (94%) ovulate by 3 months, the majority within 3 weeks. o Can use when lactating as soon as 6 wks postpartum o Noncontraceptive benefits, such as improved dysmenorrhea and possibly acne. Disadvantages: o Bleeding irregularities, including infrequent bleeding (33.6%), amenorrhea (22.2%), prolonged bleeding (17.7%), and frequent bleeding (6.7%). o ethinyl estradiol may help control bleeding during the first few months of implant use. potential side effects Most common (≥10%) adverse reactions o change in menstrual bleeding pattern, headache, vaginitis o weight increase, acne, breast pain, abdominal pain, and pharyngitis. Initial potential side effects include: o Hormone types of side effects, including headache, acne, etc. o Spotting, cramping o Slight bruising, discomfort Ongoing potential side effects include: o Lighter menses or amenorrhea o Less predictable light, short menses Absolute contraindications: o Current breast cancer is rated Category 4, However, breast cancer in the past; no evidence of disease for 5 years is a Category 3. o Pregnancy o Unexplained vaginal bleeding o Current breast cancer o Severe cirrhosis o Malignant liver tumor Combined Oral Contraceptives • Combined oral contraceptives (COCs) are a combination of estrogen and progestin. • Most COC formulations now contain between 20 to 35 mcg of ethinyl estradiol plus one of 8 available progestins. • A high number of unintended pregnancies are due to misuse or discontinuation of OCs. • Consider the “quick start” method when initiating oral contraceptives. o If last menstrual period (LMP) was within the last 5 days, the method can be started immediately. o In unprotected sex within last 2 weeks, start the contraceptive method today and advise patient to return to the clinic for a pregnancy test in 3 weeks. o Instruct women who are using the pill, patch, ring, injection, or implant to use backupcontraception for the first 7 days. o Research shows that there are no significant differences in the number of bleedingspotting days or any other bleeding parameter between the immediate and conventional starters. • Mechanism of Action: o The progestin in COCS is the main actor in preventing pregnancy. It suppresses the secretion of gonadotropin (mainly luteinizing hormone) by the pituitary gland. The estrogen primarily inhibits follicle-stimulating hormone secretion. o The estrogen also works synergistically with the progestin to affect the uterine lining and cervical mucus production. • Candidates: o Women with dysmenorrhea and menorrhagia o Women who want to regulate menses o Women who will use a daily method consistently • Advantages: o Reduced menstrual flow and dysmenorrhea for most users o Reduce the risk of ovarian cancer by 40-80% after ~ one year of use and decrease the risk from 10-12% annually thereafter o Even after discontinuing COC use, protection continues for 15-20 years. o COCs also reduce the risk of endometrial cancer by 40-50%, and like ovarian cancer, protection increases with duration of use. o 90 percent protection from ectopic pregnancy with current OC use. o Reduced incidence of benign breast disease o Effective in reducing acne. o Possible Advantages: 1) May preserve bone density, and 2) May protect against iron deficiency anemia, ovarian cysts with higher doses, and pelvic inflammatory disease. • Contraindications: o Multiple risk factors for arterial cardiovascular disease, such as smoking, diabetes, hypertension o Known thrombogenic mutations o Current or history of current ischemic heart disease, history of stroke, history of or current deep venous thrombosis or pulmonary embolism o Vascular disease o Complicated valvular heart disease o Hypertension (systolic ≥160 or diastolic ≥ 100) o Smoking (>15 cigarettes/day and age 35 or older) o Migraine headache with aura o Major surgery with prolonged immobilization o Current breast cancer o Active viral hepatitis o Severe cirrhosis o Benign or malignant liver tumors o Breastfeeding <6 weeks postpartum • Disadvantages: o Obesity may impair the effectiveness of COCs, increasing the risk of contraceptive failure by 8-12% with typical use. • Counseling: o Breakthrough and /or irregular bleeding may occur. Other side effects include breast tenderness, nausea, and bloating. o Many of these side effects usually disappear after the first few cycles of pill use. o Side effects are less likely with low-dose pills. But the lower the dose the more likely breakthrough bleeding will occur. o OC use does not increase breast cancer risk.o Use of combination OCs increases the risk of venous thromboembolism (VTE). However, the annual risk is low (1.0–3.0 per 10,000 women) and approximately half that associated with pregnancy (5.9 per 10,000). o Obesity and use of COCs are independent risk factors for venous thromboembolism. o OC use does not increase the risk of heart attack or stroke among healthy nonsmokers under age 35 who do not have other risk factors for these events. • Side effects related to Progestin (switching to a method with a different type of progestin may be helpful if experienced): o Bloating o Anxiety o Irritability o Depression o Menstrual irregularities o Reduced libido • Progestins o Most Androgenic: levonorgestrel, norgestre o Androgenic: norethindrone, ethynodiol diacetate o Least Androgenic: desogestrel, norgestimate o Spirinolactone like: drosperinone • Side effects related to Estrogen: o Breast tenderness o Nausea o Vomiting o Headaches o Elevated blood pressure (rare) Postpartum and oral contraceptives • postpartum women should not used combined hormonal contraceptives during the first 21 days after delivery because of high risk for (VTE) during this period. • During days 21-42 postpartum, women without risk factors for VTE can generally initiate combined hormonal contraceptives. W • omen with risk factors for VTE, such as previous VTE or recent cesarean delivery generally should not use these methods. • After 42 days postpartum, no restrictions on the use of combined hormonal contraceptives based on postpartum status apply. “Mini-pills,” progestin-only pills o There are currently two formulations--norethindrone (Micronor) and norgestrel (Ovrette). o Candidates: o Progestin-only pills are useful for women who want immediately reversible hormonal contraception but for whom estrogen is contraindicated because of breastfeeding, cardiovascular disease, and migraine with aura, for example. o Advantages: o Progestin-only pills (COCs also are used) can be used to correct dysfunctional uterine bleeding. o no estrogen-related side effects that COCs have, such as nausea, headache, and bloating, but they do cause irregular vaginal bleeding. o These pills protect against cancer of the uterus and ovaries, benign breast disease, and pelvic inflammatory disease. o Contraindication:o The only contraindication to taking progestin-only pills is current breast cancer. o Disadvantages: o The primary side effect is irregular menstrual bleeding, including spotting or breakthrough bleeding, amenorrhea, or shorted cycles. Irregular bleeding decreases in many users by cycle 12. Less common side effects are headache, breast tenderness, and dizziness. o Counseling: o The pill must be taken at the same time each day. o If a pill is more than 3 hours late, a backup method of contraception should be used for at least the next 48 hours. Inform women about emergency contraception. Transdermal contraceptive patch o is applied once a week to the abdomen, buttock, upper outer arm, or upper torso. o Serum concentrations are maintained for up to 10 days, suggesting that clinical efficacy would be maintained even if a scheduled change is missed for as long as 2 full days. o Three consecutive 7-day patches (21 days) are applied, followed by 1 patch-free week per cycle. o Use of the patch should be initiated during the first 24 hours of menses; no back-up is recommended. o The contraceptive efficacy of the transdermal patch is comparable to that of combination OCs.. Disadvantages: o Increased exposure to estrogen, which may increase the risk of side effects o Application site reactions. Adhesion is not affected by heat, humidity, or exercise. o Breast tenderness (1st few cycles) o Contraceptive failures may be increased among women weighing 90 kg (198 lbs) or more. Vaginal ring: Nuva ring • One ring is inserted into the vagina per cycle and is to remain in place continuously for 3 weeks, followed by a ring-free week. • Women not previously using hormonal contraception should insert the ring on or before day 5 of the cycle, counting the first day of menstruation as day 1. o Back-up contraception is recommended for the first 7 days of ring use. • Women switching from a combination OC may insert the ring any time within 7 days after the last combined estrogen/progestin OC and no later than the day that a new cycle of pills would have been started. No back-up method is needed. • Ring improves vaginal flora, leading to reduced frequency of bacterial vaginosis. • low incidence of gastrointestinal problems, such as nausea and vomiting. • Disadvantages: o Possibility of leukorrhea and vaginitis, and 1% possibility of expulsion o Hormone-related side effects o ring is rarely felt during intercourse. **If the ring falls out, it should be rinsed with warm water and reinserted within 3 hours** 3-month injectable (Depo-Provera): PROGESTIN-ONLY ● intramuscularly into the deltoid or gluteus maximus muscle every 11–13 weeks. • Mechanism of Action: o As with other progestins it not only prevents ovulation; it also reduces ovarian production of estradiol. • Candidates: o DMPA can be initiated immediately postpartum because it does not contain estrogen--it does not affect breastfeeding.o May improve conditions such as menorrhagia, dysmenorrhia, and iron deficiency anemia. o At least one-half of users develop amenorrhea within 12 months. o DMPA also can decrease the risk of dysfunctional menstrual bleeding in women who are overweight. o Women who do not wish to conceive immediately after discontinuing it. • Advantages: o Reduces the risk of endometrial cancer by up to 80%, with continuing protection after discontinuation. o Reduces risk of PID and uterine leiomyomata o Can decrease the number and severity of crises in patients with sickle cell anemia. Contraindication: o Known or suspected malignancy of the breast • Disadvantages: o Weight gain o Menstrual irregularities o Long Return to fertility (10 months) o Currently is a “black box” warning that prolonged use (> 4 years) of DMPA causes an increase in fractures or has an effect on postmenopausal bone health. OTHER METHODS • Less effective methods include male and female condoms, sponge, spermicides, and the cervical cap, which are likely to prevent pregnancy about 75% of the time with typical use. • A new study indicates that the withdrawal method is almost as effective as the male condom at preventing pregnancy. o Typical Use – estimates of typical use indicate an effectiveness rate of 82% versus 83% for typical use of male condoms. ● Female condoms can be inserted up to 8 hours before intercourse ● Simultaneous male condom use because the two materials can adhere to each other and cause slippage or breakage of one or both devices. Sponge, Diaphragm, and Cervical Cap SPONGE • The vaginal sponge is a small, circular, polyurethane sponge that contains 1 gram of nonoxynol-9 spermicide. It has a dimple on one side that fits over the cervix and a loop on the opposite side to aid in removal. It is recommended to use spermicide with the vaginal sponge. • Effective for up to 24 hours, regardless of the number of times intercourse occurs during that time. • After the last act of intercourse, it should be left in place for at least 6 hours but for no more than 24-30 hours . Diaphragms • Diaphragms come in diameters ranging from 50 to 95 mm, and a woman must be fitted for the correct size before she uses the device. • Patients should be refitted after pregnancy or childbirth or if they gain or lose 10 or more pounds. • A spermicide is applied to the diaphragm before use. • The diaphragm can be inserted up to 6 hours before intercourse and should be left in place for at least 6 hours after the last act of intercourse. (remove before 24 hrs to avoid shock) o If the woman has additional acts of intercourse before 6 hours have elapsed, she should insert fresh spermicide into the vagina without removing the device. o Women should never use any type of oil-based lubricantCERVICAL CAP ● Currently, a non-latex cervical cap (FemCap) is available in the U.S. ● reusable, flexible, domed cap ● The cervical cap comes in 3 sizes to fit most women (fitting required). o The device should be used with spermicide. Fertility Awareness • Fertility awareness methods use physical signs, symptoms, and cycle data to determine when ovulation occurs. • The Standard Days Method (SDM), on which CycleBeads are based, helps the woman track her cycle days and know when she is fertile. o avoid unprotected intercourse on days 8–19 of the menstrual cycle, as these are the fertile days. • These methods are suitable for women with menstrual cycles between 26 and 32 days long. o Users who have 2 or more cycles outside the 26–32-day range within any 1 year of use should be advised that the method may not be appropriate because of a higher risk of pregnancy • Films and suppositories spermicide require 10–15 minutes for activation o Nonoxynol-9 spermicides increase a woman’s risk of HIV-1 infection. Emergency contraception ● For most the instructions are to take 1 tablet within 72 hours (3 days) after unprotected sex or contraceptive failure • Not an abortifacient - not same as abortion pill (RU-486/mifepristone) • No effect on future fertility • There are 5 methods available in the U.S. for EC: o Plan B One-Step - high-dose progestin-only pill o Next Choice One Dose and My Way pill are one-pill 1.75mg levonorgestrel generics. o Levonorgestrel tablests are two 0.75mg pill formulation o Ella is a 30mg ulipristal acetate dedicated emergency contraception pill for use up to 120 hours (5 days) after unprotected sex. o Certain daily oral contraceptive pills that contain a combination of estrogen and progesterone when prescribed in higher-than-normal doses o Insertion of the copper-T IUD. Testicular torsion - Acute scrotal pain is a medical emergency requiring PROMPT attention to rule out testicular torsion. - the result of twisting of the spermatic cord, which subsequently compromises the blood supply to the testicle. - Generally, there is a 6-hour window following a testicular torsion before significant ischemic damage and alteration in spermatic morphology and formation occurs - occur after physical exertion, trauma, or on arising. - most common in adolescence and is uncommon before 10 years old. - left side is twice as likely to be involved because of the longer spermatic cord. Clinical Findings • Sudden onset of unilateral scrotal pain, often associated with nausea and vomiting. The pain is unrelenting. • History of bouts of intermittent testicular pain. Prior episodes of transient pain are reported in about half of patients. • May be described as abdominal or inguinal pain by the embarrassed child. • Fever is minimal or absent. • Gradual, progressive swelling of involved scrotum with redness, warmth, and tenderness• The ipsilateral scrotum can be edematous, erythematous, and warm • Testis swollen larger than opposite side, elevated, lying transversely, exquisitely painful • Spermatic cord thickened, twisted, and tender • Slight elevation of the testis increases pain (in epididymitis it relieves pain) • Transillumination can reveal a solid mass • The cremasteric reflex is absent on the side with torsion • Neonate—hard, painless, non-transilluminating mass with edema or discolored scrotal skin Diagnostic Studies • UA is usually normal and pyuria and bacteriuria indicate UTI, epididymitis, or orchitis. • Doppler ultrasound: Testicular flow scan considered if Doppler ultrasound within normal and time allows. Management ● surgical emergency ● Occasionally manual reduction can be performed, but surgery should follow within 6 to 12 hours to prevent retorsion, preserve fertility, and prevent abscess and atrophy. ● Rest and scrotal support do not provide relief Wilms Tumor - Wilms tumor or Nephroblastoma is the most common type of renal cancer in children accounting for 90% of childhood malignancies that arise in the urogenital tract. - It is the fifth most common type of pediatric cancers. - Wilms tumor is an embryonal renal neoplasm which contains blastemal, stromal or epithelial cell types. Epidemiology ● Wilms tumor is seen more in females than males, Whites more than Blacks and rarely in Asians. ● It makes up 6-7% of all childhood cancers. ● More than 80% are diagnosed before age 5 years. ● The median age at diagnosis is 3.5 years. ● It makes up 95% of all renal cancers seen in children younger than 5 years old. Etiology of Wilms ● The majority of cases are of sporadic occurrence. ● In some children they also have malformation or syndromes including: o aniridia( no iris in either eye), o hemihypertrophy (where one side of the body is larger than the other, these children have 100 times the risk factor), o GU abnormalities (cryptorchidism, hypospadias, gonadal dysgenesis, pseudohermaphroditism, and horseshoe kidney), o Beckwith Wiedermann syndrome ( a genetic over growth syndrome), o Denys-Drash Syndrome, and WAGR Syndrome( Wilms tumor, aniridia, ambiguous genitalia, mental retardation ). o Abnormality of chromosome 11 at the 11p15 locus are associated with Beckwith Wiedermann syndrome. o Wilm’s tumor suppressor gene WT1 has been identified. P53 has been linked with anaplastic Wilms tumor. Risk factors o There are different causes of Wilms tumors there areo heredity or mutation of genes, o familial which is autosomal dominant with low penetrance, o possible parental work exposure. ● Risk factors include work exposure is listed because of increased cases involving children of parents who worked in the following jobs. o (auto mechanic, auto body workers and welders). o Maternal exposure to pesticides. o High birth weight or preterm delivery. o Being first born has an increased risk. Signs and Symptoms ● 80% of children present with abdominal mass with or without associated abdominal pain or hematuria. o Asymptomatic with palpable abdominal mass o Parents usually state that they noticed the child’s stomach getting bigger. o The mass is usually smooth and firm and unilateral. o 25% will present with hyptertension, o gross hematuria is rare but microscopic hematuria may be present in 25% of patients. o Kidney function is usually normal. Diagnosis o renal ultrasound should be done asap to confirm the diagnosis. o A chest CT scan and abdominal CT scan needs done to assess for metastases. o Biopsies are not routinely performed. Treatment o Nephrectomy is the treatment of choice and should be done as soon as possible after diagnosis. o The surgeon should be familiar with Wilms tumors since they will be the one staging the disease during the surgery. o 10% of patients will have metastases at diagnosis. o Of that 10% 80% will have pulmonary mets and 20% will have liver mets. Staging of Wilms Tumor is based on the spreading of the tumor. Stage 1- Tumor is limited to the kidney and is able to be totally removed. Stage 2- Tumor extended beyond the kidney no peritoneal involvement, can be Totally removed. Stage 3- No metastases but residual tumor remains in abdomen after surgery. Stage 4- Metastases are present usually to lung. Stage 5- Bilateral kidneys have tumors at time of diagnosis. Histology is also looked at for treatment plans the histology is listed as favorable or unfavorable. o Favorable histology refers to the normal Wilms tumor histology but loss of heterozygosity of chromosomes 1p and 16q are adverse prognostic factors for those patients. o Unfavorable histology means diffuse anaplasia (extreme nuclear aplasia) is present in 5% of Wilms tumors. Even a small number of abnormal nuclei can worsen the prognosis in stage 2,3 and 4 tumors.Treatment Plans o Treatment in North America is multifactorial. o Treatment for stage 1 and 2 involves surgery pending tumor location and size different surgical options are available to the surgeon ( partial nephrectomy- removal of the tumor and some surrounding tissue but leaving a partial functioning kidney, total nephrectomy- removal of entire kidney, radical nephrectomy – removal of entire kidney and surrounding tissues the ureter, adrenal gland and lymph nodes). o Chemotherapy is started usually within 5 days of surgery. Stage 3 and 4 o Surgery and chemotherapy same as stage 1 and 2 but radiation is started within 10 days of surgery. Stage 5 o If both kidneys are removed pt will be on dialysis until a transplant is available. o Pt will undergo both chemo and radiation therapy post op. The length and type of chemotherapy given depends on stage and histology results. o In Europe chemo therapy is started preop to downgrade tumor staging at surgery. No studies have been done as of yet to show if chemo preop changes patient outcomes or not. o The national Wilms Tumor Study Group’s 4th study (NWTS-4) stated survival rates were improved by intensifying treatment initially but shortening the treatments from 60 weeks average to 24 weeks. o currently 4-year overall survival rates through NWTS-4 are as follows: stage I FH, 96%; stage II–IV FH, 82%–92%; stage I–III UH (diffuse anaplasia), 56%–70%; stage IV UH, 17%. Follow up management o Pts with Wilms tumor treatment will be followed up every 4 months for first year then every 6 months for year 2 to 3 then yearly. o At each follow up appointment they will have CBC and CT scan of chest and abdomen. o For patients at risk for Wilms tumor should have renal ultrasound every 3 to 4 months until age 5 years. Questions 1. Sally age 15 months is brought to your office for her 15month well child visit. Her mother and father are both present for the exam. Her mother tells you she has noticed over the past 3 weeks that Sally had to go up a size in clothes because they are too tight on her stomach. On examination of Sally’s abdomen, you feel a smooth firm mass in the right upper quadrant of her abdomen. Bowel sounds are normal and abdomen is soft other than for the mass. What needs to be ordered to evaluate this mass? a) CT Scan chest and abdomen b) Ultrasound of liver c) CT Scan of brain. d) Exploratory Lap Answer A.2. Jane is 3 months old she is the first born of Steve and Mary. Steve works as an autobody repairman and Mary works as a pest exterminator. What does Janes history put her at risk for? a) Acute Myelocytic Leukemia b) Wilms Tumor c) Enlarged Spleen d) Pulmonary Fibrosis Answer b: Wilms Tumor 3. What is the standard for screening high risk children for Wilms Tumor. a) renal ultrasound every 3-4 months until age 5 years b) yearly renal ultrasound c) no screening is necessary unless a mass is detected on routine examination d) .Ct Scan abdomen and chest every 6 months until age 5 years. Answer A: renal ultrasound every 3-4 months until age 5 yearsWEEK-4: Lesson:3 Cardiac Symptoms and Diseases in Children Review of Fetal Circulation and Cardiac Cycle - Cardiac anomalies affect almost 8 in 1,000 children, with 90% of these patients living well into adulthood - The majority of children are noted to have a murmur at some point in their life noted on routine physical examinations, but less than 1% of all murmurs are caused by a congenital defect - review the differences between fetal and non-fetal circulation and have a working knowledge of the locations and closure times for open fetal circulation routes. - Please note the location of the following fetal shunts. ● Ductus venosus: Connects the umbilical vein to the inferior vena cava. ● Ductus arteriosus: Connects the pulmonary artery to the aorta. ● Foramen Ovale: Opening between the right and left atrium. ● A routine and complete cardiac exam for symptomatic patients or for patients undergoing a sports physical should include a thorough familial and past medical history and include the evaluation of syncopal events, past cardiac history, medications, other substances, diet, hydration, and neurological symptoms. ● The physical exam should include vital signs, general inspection, skin and nail bed color, respiratory rate, and full inspection, auscultation, and palpation of the chest and peripheral pulses. Evaluation of Murmurs Murmurs are the most common finding leading to a cardiology referral in children. New onset, worsening, or murmurs associated with other symptoms should always be evaluated further by a pediatric cardiologist. In documenting murmurs, the following should be noted. ● Location ● Radiation ● Relationship to the cardiac cycle ● Intensity (Grade I-VI) ● Quality ● Positional changesGrading for murmurs is as follows. Grade I—soft Grade II—soft, but easily heard Grade III—loud but without a palpable thrill Grade IV—loud and with a precordial thrill Grade V—loud with a thrill, and audible with only the edge of the stethoscope Grade VI—very loud and audible with the stethoscope off of the chest There are several types of innocent murmurs. Two of the most common are below: Newborn murmurs—This murmur is heard at the left lower sternal boarder and only in the first few days of life, is quiet and does not radiate, and lasts only the first few weeks of life. Still’s murmur—This murmur is the most common innocent murmur in children. It is soft, grade I-III, is more prominent in a supine position, with fever or anemia, and can disappear with inspiration. (Hay et al., 2014) Congenital Cardiac Disease Congenital cardiac anomalies and the structure of the heart should be known by the NP. Many anomalies are noted prior to birth now due to ultrasonography, but many can still go undetected. For example, Coarctation of the aorta can be missed until the child is well into their first year of life or has presenting symptoms. Do not assume that you will not find congenital cardiac defects in children outside of the newborn period and be aware of signs and symptoms of disease. The following are listings of acyanotic and cyanotic heart diseases. Acyanotic Cyanotic Atrial septal defect Tetralogy of Fallot Ventricular septal defect Pulmonary atresia Atrioventricular septal defect Tricuspid atresia Patent ductus arteriosus Hypoplastic left heart Pulmonary valve stenosis Transposition of the great vessels Coarctation of the Aorta Truncus arteriosus Aortic stenosisProlonged QT Syndrome and Sudden Cardiac Death Sudden cardiac death in youth and athletes can occur for various reasons; prolonged QT syndrome and cardiovascular disease are two of the most common. The survival rate of non-traumatic cardiac arrest is only 7.8%, but bystander witnessed ventricular fibrillation has a 57% survival rate (American Heart Association, 2013). Athletes are at increasing risk due to increasing rates of youth hypertension, high cholesterol, and stimulant use. The majority of sudden deaths in athletes from cardiovascular disease are male (89%), in high school (54%), during exertion (82%), and being of African-American descent (29%) (American Heart Association, 2013). Some of the most important actions to prevent deaths are completion of a good history and sports physical examination, screening of children with a familial history of sudden cardiac death, education of patients, families, and schools about the importance of limiting exertion in heat, adequate hydration, and proper training of coaching staff to deal with and recognize important symptoms and take action in emergent situations. Iron deficiency anemia (Microcytic anemia) ● Approximately 3% to 7% of children at age 1 year suffer from iron deficiency ● Nine percent of adolescent girls develop iron deficiency and 2% to 3% between the ages of 12 and 19 years old develop anemia primarily due to rapid growth, heavy menses, and nutritionally inadequate ● Iron deficiency is the most common cause of anemia, even as cases steadily decline when nutritional practices improve. Risk Factors for Iron Deficiency Anemia • History of prematurity or low birth weight • Exposure to lead • Exclusive breastfeeding beyond 6 months without iron supplementation • Weaning to whole cow's milk without iron source • Feeding problems • Special health care needs • Prolonged bottle use • Low socioeconomic status • Excessive or prolonged intake of cow's milk • Obesity • Hispanic or Asian descent • Adolescent female, excessive menstrual bleeding Diagnostic tools ● most cost-effective measurement is a CBC, which includes the Hgb, Hct, MCV, and RDW. ● A ferritin level may also be helpful because this indicates body stores of iron (interpret carefully) ● Hgb screening for anemia at 12 months old (including screening for risk factor of iron deficieny) ● Risk assessment for anemia should be performed at all preventive pediatric health care visits with followup blood testing if positive. ● The presence of low levels of iron facilitates intestinal absorption of lead. ● The RDW is the earliest marker of iron deficiency. ● Pica (appetite for nonfood items such as paper, dirt, and clay) and pagophagia (the desire to ingest ice) may be present ● Serum iron is low, hypochromic, microcytic, low saturation, MCV/RBC ratio >13, blood in stool or urineA trial of iron supplementation for 4 to 6 weeks without further diagnostic testing and then follow the child's Hgb and reticulocyte counts. - ferrous sulfate (3 to 6 mg/kg/day of elemental iron in two to three divided doses or 3 mg/kg/day in one or two divided doses for mild or moderate IDA - Levels less than 4 g/dL necessitate consultation with a hematologist - If treatment with oral iron supplements is effective, follow-up Hgb in 1 month should reveal a minimum 1 to 2 g/dL improvement, but the reticulocyte count will increase to greater than 3% in 48 to 96 hours (diagnosis can be made then). - iron supplementation should continue for 2 to 3 months to normalize Hgb, then continue for 2 to 4 months to replace depleted iron stores. - Hematologic and iron status should be rechecked 6 months after iron supplements are stopped to determine resolution of the anemia and adequacy of iron stores Classification History Physical Findings Screening Tests Diagnostic Studies Treatment Iron deficiency anemia (IDA) Infant and toddler Excessive cow's milk ingestion Poor solid food intake; Fatigue Irritability Excess milk intake Waxy, sallow appearance of skin; Pallor or none PICA, Rarely high HR,CHF systolic murmurs, Hgb: 8-11 g/dL (moderate); <7 g/dL (severe) MCV: <60 fL Reticulocyte count: ↓ to sl ↑ Serum Fe: ↓ TIBC: ↑ % Saturation: ↓ Ferrous sulfate, 3 to 6 mg/kg/day of elemental iron Discontinue cow's milk Limit formula to <24 oz/day and encourage solid food Diagnosis Mean Corpuscular Volume Red Blood Count Number Red Blood Cell Distribution Width Ferritin Total IronBinding Capacity Iron deficiency anemia (IDA) Low or normal Low High (>14%) Low High Patient and Family Education - increase iron-rich food sources in their child's diet.- Exclusively breastfed term infants should be started on iron supplementation at 4 months old and pureed meats added to the child's diet after 6 months old. - Whole cow's milk should be avoided in infants younger than 12 months old due to its low iron content and possibility of insensible GI blood loss. - After 12 months old, cow's milk ingestion should be limited to 24 ounces per day. - For preterm infants, supplementation with oral iron drops should begin no later than 1 month old. (2 mg/kg/day after 2 weeks of age through 12 months old) - avoid giving iron with meals or milk, that vitamin C juice enhances absorption, and that the child's stools will probably turn black. o Foods containing soy can inhibit the absorption of iron. o Any dental staining associated with taking iron can be removed with dental cleaning. o Commercial cereal (such as, Kix) can be given as a dry food snack Febrile seizures - most common type of seizures in children. - brief, generalized, clonic or tonic-clonic in nature, and can be either simple or complex. - A concurrent illness is present with rapid fever rise to at least more than 102.2° F (39° C), but the fever is not necessarily that high at the time of the seizure. - Minimal postictal confusion is associated with febrile seizures. o Simple febrile seizures last less than 15 minutes and may recur during the same febrile illness period. o Complex febrile seizures last longer than 15 minutes, can recur on the same day, and can have focal attributes (even during the postictal phase). - Febrile SE is uncommon, rarely stops spontaneously, is fairly resistant to medications, and can persist for a long period of time. - Most children in febrile SE require one or more medications to end the seizure. - A report found that reducing the time from seizure onset to anticonvulsant medication administration was key to reducing the seizure duration during an episode. Risk factors - Family medical history for febrile seizures or - in those with predisposing factors (e.g., neonatal intensive care unit [NICU] stay more than 30 days, developmental delay, day care attendance). - Age 6 months to 60 months. - Male gender - lower sodium level. - Approximately 2% to 5% of neurologically healthy infants and young children experience at least one simple febrile seizure with about 30% of this group experiencing a second episode Diagnostic Studies. • A lumbar puncture may be done in infants younger than 12 months old and who may also have used an antibiotic prior to seizure onset, and/or in those who have signs of meningeal irritation. • Blood glucose in all children. • CBC, calcium, electrolytes, and urinalysis are optional but frequently included. • EEG if neurologic signs are present or seizure was atypical. • MRI for complex febrile seizure features or if any doubt exists about the diagnosis. Management • Protect the airway, breathing, and circulation if the seizure is still occurring. Place the child in a side-lying position to prevent aspiration or airway obstruction. • Reduce the fever with acetaminophen or ibuprofen (oral or suppository) after the seizure has stopped, although the use of antipyretics will not necessarily prevent another febrile seizure.• The child should be seen shortly after the seizure. transport to an emergency center if the seizure lasts more than 10 minutes. • anticonvulsants are not recommended for febrile seizures, but they may be considered if the child has abnormal neurologic findings or developmental delays; the initial seizure was complex febrile, and there is a family history of afebrile seizures or if the child has recurrent, prolonged simple febrile seizures. Prophylaxis for Recurrent Febrile Seizures - Prolonged anticonvulsant prophylaxis is not recommended. - In the rare instance that prophylaxis is indicated, diazepam PO or Rectal can be given over the course of the febrile illness (usually for 2 to 3 days). - Antipyretics can reduce the discomfort associated with a fever but do not alter the risk of having another febrile seizure. - no long-term consequences are associated with febrile seizures, information that febrile seizures recur in some children and that nothing can be done to prevent the seizures (no serious impairment of any kind; recurrent higher chance for epilepsy). Study guide- part-3 Topics covered 1. Turner Syndrome 2. Down Syndrome 3. Precocious puberty 4. Menarche 5. Puberty 6. Primary Dysmenorrhea 7. Coarctation of the aorta 8. Supravalvular Aortic Valve Stenosis 9. Mitral Valve prolapse 10. Dissecting aortic arch 11. Headaches Turners syndrome 45 XO genotype most common – short stature – variable degrees of puberty– primary amenorrhea – multiple congenital anomalies – primary ovarian failure – variable breast and axillary/pubic hair development – associated with short stature homeobox (SHOX) mutations – Residual ovarian function » breast development (15-25%) » menarche (5-10%) pregnancy (1-3% Turner syndrome is a chromosomal condition that affects development in females. The most common feature of Turner syndrome is short stature, which becomes evident by about age 5. An early loss of ovarian function is also common. The ovaries develop normally at first, but egg cells (oocytes) usually die prematurely and most ovarian tissue degenerates before birth. Many affected girls do not undergo puberty without hormone therapy, and most are infertile. High rate of spontaneous pregnancy lossin XO female fetus. Antenatal diagnosis possible & blood testing. Turner Syndrome: Important to monitor ▪ growth using specialized chart ▪ non-verbal learning disabilities ▪ annual vision hearing, bp for htn, thyroid screen ▪ Scoliosis ▪ Cardiac and renal abnormalities ▪ Estrogen supplementation with puberty Signs & Symptoms: About 30 percent of females with Turner syndrome characterized by short stature, 5ft (152cm), aeb age 5. ➢ Wide neck webbing, ➢ and a low hairline, ➢ swelling of the hands and feet, ➢ skeletal abnormalities, renal abnormalities. ➢ Absent menses and infertility ➢ Broad shield-shaped chest ➢ At birth noticeable narrow, high arched palate, retrognathia (Lower jaw not prominent). ➢ Low set ears, edema of hands and feet, ➢ Females classified as Mosiac Turner’s syndrome have milder features. About ½ of those born with Turner syndrome are also born with a heart defect, such as coarctation of the aorta and valve defects. Downs syndrome or trisomy 21 is the most common inherited genetic syndrome associated with a variable degree of mental impairment and karyotype 47 XY or XX _ 21. Down Syndrome: Monitor▪ Growth using spcld growth chart ▪ OSA ▪ Annual vision/hearing ▪ Annual thyroid screen ▪ Caution- Increased risk of leukemia, duodenal atresia & cardiac anomalies Developmental Cues: (Burns) pg 1163 ▪ Intellectual disability/ developmental delays ▪ Hearing loss ▪ Hypotonia as infant Etiology/Incidence 1. Three different genetic alterations a. In 95%, Down syndrome is result of a random nondisjunction (trisomy 21) b. Less commonly, it occurs as mosaicism where some cells are affects and others are normal c. Balanced translocation, often involves chromosome 21 and 14 2. 1 in 800 to 1,000 live births 3. Affects males and females equally. Risk factors include ▪ advanced maternal age, ▪ previous child with Down syndrome or ▪ another chromosomal abnormality; ▪ parental balanced translocation; ▪ parents with chromosomal problems Signs and Symptoms 1. Mental retardation, mild to severe 2. Typical phenotypic signs at birth a. Head—midface hypoplasia; small brachycephalic head with epicanthal folds, fl at nasal bridge, upward slanting palpebral fissures, Brushfield spots, small mouth Eyes- Myopia b. Ears—small ears c. Neck—excessive skin at the nape of the neck d. Hands and feet—simian crease and short fifth finger with clinodactyly; a wide space, often with a deep fissure between the first and second toes; lymphedema, brachydactyly (shortened digits), e. Neurological—mental impairment is variable, ranging from mild (IQ: 50–70), to moderate (IQ: 35–50), and only occasionally to severe (IQ: 20–35) f. Cardiac—increased risk of congenital heart defects (50%) g. GI—Hirschsprung’s disease (1%); gastrointestinal atresias (12%) h. Musculoskeletal—hypotonia; acquired hip dislocation (6%) Differential Diagnosis: Other genetic or chromosomal syndromes Physical Findings:▪ Phenotype as above ▪ Hearing loss (75%); otitis media (50%–70%)3. Obstructive sleep apnea (50%–75%) ▪ Signs of congenital heart disease—50%; ▪ Endocardial cushion defect most common(45%) with ventricular septal defects (35%) second ▪ Signs of hypothyroidism and other endocrine problems—15% ▪ Signs of anomaly of GI tract 5%; Celiac disease15% ▪ Ligamentous laxity—100% ▪ Hematological—leukemia ( 1%)9. Eye—eye disease (60%), including cataracts 15%), and severe refractive errors (50%) ▪ Obesity—50% by early childhood ▪ Musculoskeletal—ankle pronation and pes planus ▪ Premature aging ▪ At risk for Alzheimers, Hypothyroidism & Leukemia Diagnostic Tests/Findings Pre or postnatal chromosome analysis reveals 47 XY or XX _ 21 karyotype ▪ CBC with differential to identify those with leukemia; 10 to 15 fold increased risk ▪ Symptoms of atlantoaxial instability (neckpain, decreased range of motion of theneck, gait disturbance, bowel or bladder dysfunction, hyperreflexia or paresthesias): ▪ radiographic finding of atlantoaxial instability ▪ Ophthalmologic evaluations every two years between 3 to 5 years then yearly after this (50% ▪ risk of refractive errors between (3 to 5 years) Management/Treatment : Primary prevention via education : ▪ Risk factors: Secondary prevention via prenatal diagnosis Monitor for growth and family support every well visit ▪ CBC at one year, every year starting at age 13 ▪ to 21, and if clinically indicated ▪ Initial evaluation by cardiology to rule out congenital heart defect even if no murmurs are hear Screen for celiac disease using tissue transglutaminase ▪ and IgA starting at age 2 ▪ Early intervention by PT, OT, speech ▪ therapists; special education; review individualized ▪ educational plan ▪ Genetic counseling for parents and older siblings ▪ . Periodic full history and physical with sensory and developmental evaluations ▪ Nutritional support ▪ Screen for thyroid disease yearly; up to 30% risk ▪ Prompt referral for associated conditions ▪ Patient advocate and guide family during transition to adult care ▪ Referral to appropriate web sites for education and support Precocious puberty - Signs of puberty earlier than expected All endocrine occurs in the pituitary Causes :▪ Exogenous ▪ Adrenal ▪ Obesity Signs- no endometrial stripe should be present – Females • Thelarche – Generally considered the onset of puberty – Occurs in most girls at 9.5-10.4 • Menarche – Mean age of onset = 12 yrs • Adrenarche – Usual onset at approx. age 9.4-10.6 yrs • Linear Growth – Generally occurs before Tanner Stage 2 breast development – Generally adds 20-25cm of height in females – Growth hormone (GH) increases during puberty » yielding 50% of growth spurt Menarche onset of menses at age 12 or 13 Menarche is the occurrence of a first menstrual period in the female adolescent. Menstruation is the monthly shedding of the functional layer of the uterine endometrial lining that occurs when ovulation is not followed by fertilization. It occurs approximately every 28 days, with a range from every 21 to every 45 days. The average age of onset of menarche is 12.4 years. Most menstrual periods last between 3 and 7 days, and menses that last more than 10 days are considered abnormal. Menarche signals maturation of the adolescent female body and is commonly associated with the ability to ovulate and reproduce. However, the appearance of menarche does not guarantee either ovulation or fertility. Puberty: Puberty is the developmental stage that is characterized by physical, as well as psychological and social maturation. When an adolescent does not experience puberty in the expected time frame, there can be adverse affects upon the adolescent’s well-being. This delay can be caused by a wide range of either benign or pathologic etiologies. Healthcare providers evaluate the patient’s history, physical exam findings, and other diagnostics to determine if ongoing surveillance is needed and/or whether the individual requires treatment for an underlying medical condition. Puberty is the beginning of sexual maturity. Puberty is the period when a child changes physically, hormonally, and sexually, and becomes able to reproduce. Delayed Puberty: Males No secondary sexual characteristics by 14 years > 5 years since first signs of puberty to Tanner V Causes: constitutional growth delay, primary or secondary gonadal failure, malnutrition or disordered eating, Klinefelter’s syndrome Delayed Puberty: Females Evaluated if no pubertal signs by 13, or no menarche by 16 Failure to complete development Tanner V within 4 years of onset of secondary sex characteristics Most common cause: constitutional growth delay (delayed skeletal muscle growth) Other causes: Turner’s Syndrome, extreme athleticism, disordered eating, primary or secondary gonadal failure. Precocious Puberty: Most cases of precocious puberty have no known cause. In some cases, the pituitary gland, which regulates the release of most of the body's hormones, signals the ovaries and testicles to begin hormone production prematurely. Signs of puberty may also appear early because of problems with adrenal gland, ovary or testicle function. Some causes of early puberty include congenital adrenal hyperplasia (CAH), McCune-Albright Syndrome, and spina bifida with hydrocephalus.Pubertal development prior to normal age of onset GIRLS: Before 8 years old in Caucasian, 7 years old African-American and Latino Pubertal onset advanced in obesity Central: Breast development, followed by pubic hair growth, menarche *Note that girls who are obese can have breast bud development without other signs of puberty. Precocious Puberty BOYS: Secondary sexual characteristics prior to age 9 BOTH Bone age on X-ray will be older than chronological age. Treatment in both is medications to stop stimulation of their hypothalamus-pituitary-adrenal axis. Primary Dysmenorrhea : Burns (pg 968) ▪ Primary Dysmenorrhea has no pelvic pathologic condition identified whereas secondary has a pelvic pathologic condition Pathophysiology ▪ PD is painful menses caused by an exaggerated production of prostaglandins, (F2 ALPHA) in the endometrium- causing uterine contractions and vasoconstriction leading to ischemia and pain, elevation or peak of prostaglandins is brought about by falling progesterone levels during luteal phases in ovulatory cycles. Epidemiology: ▪ Leading cause of absenteeism in schools and work > 10% ▪ Present in 50 % of adolescents Clinical findings: ▪ Ask about history (menstrual), attitudes and beliefs ▪ Onset: 6-24 mos after menarche ▪ Location- lower mid-abdominal area radiating to back/thighs ▪ Duration/ timing of pain ▪ Character ▪ Associated sx, n/v, diarrhea, headaches, fatigue, nervousness, dizziness, urinary frequency low back pain ▪ Aggravating factors ▪ Treatment or meds tried including complementary and Alternating medicines, (CAM) ▪ Sexual activity ▪ Absenteeism from school and work ▪ Cigarette smoking ▪ Family hx of dysmenorrhea ▪ For secondary dysmenorrhea ask about onset and pelvic pain other menstruation, character of pain, hx of infection dyspareunia, hx of sexual abuse, family hx of endometriosis ▪ Physical Examination: ▪ Complete physical exam if secondary dysmenorrhea is suspected, may defer bimanaul or speculum if hymen intact Diagnostic studies if indicated: ▪ NAAT’S or cervical cultures for GC ▪ CBC with sed rate if PID suspected ▪ Pregnancy test ▪ Pelvic ultrasoundManagement- ▪ Prostaglandin Synthetase inhibitors, administered at onset of menses or if cramping precedes menses at onset of sx. ▪ Tx for duration of pain 1-2 days ▪ Trial period should extend 3 cycles if fails try another alternative prostaglandin inhibitor, eg- PI ARE ▪ Ibuprofen 400-800 mg po tid with food ▪ Naproxen 500 mg at onset f/o by 250 mg-500mg ▪ Naproxen Sodium: 550 mg at onset f/o 275 mg q6-12 hrs, max dose 1375 mg/24 hrs ▪ Mefenamic acid : 500 mg at onset f/o 250mg q6h ▪ Meclofenanate: 100 mg initially 50-100mg q6h ▪ OCP’S used also as suppress ovulation total progesterone-induced prostaglandin production is decreased in the endometrium. Dose recommended is 30-35 mcg estrogen-progestin combimation pill for 3-6mos trial if PI arenot successful. ▪ CAM is beneficial like, application of topical heat, ▪ Thiamine 100 mg/daily ▪ Toki-shakuyaku-san (herbal remedy), 2.5mg 3 times a day ▪ High frequency TENS ▪ Vit E , 500 units/DAY ▪ Magnesium f/o up by telephone or visit to adjust dose or change as needed. Stress, reduction exercise, and well-balanced diet wit ample of fiber and water in addition to decreasing caffeine, chocolate, and salt intake maybe helpful. Coarctation of the aorta (Burns, 779) • Congenital birth defect that presents with narrowing within the aorta can be due to the following factors : • Occurs as a single defect caused by a disturbance in the development of aorta or 2ND to PDA ➢ abnormal genetic development of embryo, ➢ decreased blood flow within the uterine through the aorta resulting in underdevelopment of the aorta, and ➢ abnormal arterial duct tissue in the wall of aorta which inhibits blood flow to the aortic vessel ➢ Coarctation usually occur at the lower end of left subclavian artery at the site where arterial duct closes➢ Narrowing leads to higher pressure closer to the obstruction and hypoperfusion distal to the defect or coarctation ➢ The increase pressure and overload eventually results in enlargement of left ventricles and heart failure ➢ Apparent in the first 6 weeks in newborns Epidemiology ➢ CoA occurs in 4 out of 10,000 live births in the US ➢ CoA accounts to 6 to 8 percent of all congenital defects of the heart ➢ Genetic predisposition ➢ Prevalent in male more than female ➢ Affects 30 %percent of female with Turner syndrome Signs & symptoms: ▪ Tachypnea ▪ Poor feeding ▪ Cool lower extremities ▪ In children 3-5 yrs of age COA may go unnoticed until htn or a murmur is detected ▪ Retrospective children with COA may c/o of leg pain with exercises and headaces. Physical Examination: ▪ Upper extremity hypertension with lower extremity hypotension , ▪ poor lower extremity perfusion with mottling or pallor can be present in severe cases ▪ delayed timing and absent or weak arterial and other distal arterial pulses ▪ Bounding brachial , radial , and carotid pulses may occur ▪ Signs of CHF may be evident ▪ A systolic ejection murmur may be detected in the left infraclavicular region- radiating to back ▪ Ventricular heave at the apex may be palpated ▪ A gallop rhythm may occur in infants with CHF. Diagnostics • Chest X-ray may display normal findings, slight cardiomegaly • Echocardiogram is the initial test per ACC/AHA guidelines for patients with valvular disease • Echocardiogram will confirm the diagnosis and can detect the location of constriction; can be helpful after surgical repair of CoA postoperative evaluation • MRI will show the location and structure and anatomy of aortic coarctation Management: ▪ In neonatal coarctation, PGE is used to maintain or reopen the ductus ▪ Surgical resection of constricted area is performed. Restenosis occurs id repair was befor 1 year of age, Balloon angioplasty or valvulopasty is also performed for initial coarctation ▪ In older children mgmt. of hypertension with anti-hypertensives may be required post surgery, BP should be monitored postoperatively ▪ If residual bp gradient between arm and legs is less than 20 mmhg children with surgery may participate in an competitive sports, however intense weight lifting and wrestling should be avoided in the first year ▪ Lifelong f/o is necessary due to risk of recoarctation and residual htn ▪ SBE prophylaxis is no longer considered necessary except in the 6 month period postop if prosthetic material used Supravalvular Aortic Valve Stenosis: (Burns) pg 777 ▪ Most common form of stenosis ▪ Usu bicuspid rather tricuspid ▪ Stenosis causes increased pressure load on the left ventricle leading to LVH and ventricular failure▪ The bicuspid valve becomes more stenotic and often regurgitant ▪ More common in females with Turners syndrome ▪ AS occurs in 3%-8% of all CHD with male to female ratio of 4:1 Signs AND Symptoms: ▪ Asymptomatic with a murmur noted on routine P.EXM as progression is experienced ▪ Activity intolerance, chest pain and fatigue or syncope can develop ▪ CHF, low cardiac output and shock may be evident in newborns ▪ Sudden death from arrhythmias can occur from increasing stenosis and exertion ▪ Growth and development is normal Physical Examination ▪ BP may reveal a narrow pulse pressure, apical pulse is pronounced ▪ A grade III TO IV/VI , loud, harsh systolic crescendo-decrescendo ▪ Murmur is best heard at upper right sternal border radiating to neck. LLSB and apex ▪ With a valvular lesion a faint early systolic click at LLSB may be heard Diagnostic Tests ▪ Chest radiographs are usually normal or may show LVH enlarged heart, and or rib notching ▪ Adults develop calcification of aortic valves over time ▪ ECG/EGG can be normal or show LVH and inverted T-Waves ▪ 24 hr holter monitor or 30-day monitor can show ventricular arrhythmia ▪ ECHOCARDIOGRAM is the diagnostic examination of choice. Management ▪ Balloon valvuloplasty of the stenotic valve is the initial palliative tx in the newborn ▪ In older children valve replacement may be necessary ▪ Patients with supravalvular aortic stenosis require resection of the narrowed area wit patch material ▪ For gradient > 35 mmHG surgical resection is required ▪ Children with mild AS, can participate in all sports but should have all annual cardiac examination ▪ Moderate aortic stenosis children should low intensity sports such as ( golf, bowling, table tennis or softball). ▪ Children with severe AS, or moderate AS should avoid competitive sports because of the risk of sudden death from ventricular arrhythmias. ▪ SBE prophylaxis is necessary for 6 mos after surgery ▪ Anticoagulation is necessary with mechanical valve replacement Headaches: Burns, (pg 685) Most Common Types of Primary Headaches Seen in Primary Care Settings Diagnostic Criteria Based on History Pediatric Migraine Headache A. More than five attacks fulfilling features of B through D B. Duration: 2 to 72 hours C. At least two of the following features: 1. Bilateral or unilateral (commonly bilateral in young children; unilateral pain usually emerges in late adolescence or early adult life) a. Usually frontal/temporal b. Occipital is unusual and should be carefully evaluated (occipital headache in children whether unilateral or bilateral is rare and calls for diagnostic caution; many cases are attributable to structural lesions)2. Pulsating quality 3. Moderate to severe intensity aggravated by routine physical activity 4. At least one of the following: a. Nausea and/or vomiting b. Photophobia and phonophobia (can infer from behavior) 5. Not attributed to another disorder Infrequent Episodic Tension Type Headache A. At least 10 episodes occurring on <1 day per month on average (<12 days per year) and fulfilling criteria B through D B. Headache lasting from 30 minutes to 7 days C. Headache has at least two of the following characteristics: 1. Bilateral location 2. Pressing/tightening (non-pulsating) quality 3. Mild or moderate intensity 4. Not aggravated by routine physical activity, such as walking or climbing stairs D. Both of the following: 1. No nausea or vomiting (anorexia may occur) 2. No more than one of photophobia or phonophobia E. Not attributed to another ICHD-3 diagnosis Chronic Tension Headache A. Headache occurring on ≥15 days per month on average for >3 months (≥180 days per year) and fulfilling criteria B through D B. Headache lasts hours to days or may be continuous C. Headache has at least two of the following characteristics: 1. Bilateral location 2. Pressing/tightening (non-pulsating) quality 3. Mild or moderate intensity 4. Not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. No more than one of photophobia, phonophobia, or mild nausea 2. Neither moderate or severe nausea nor vomiting E. Not attributed to another ICHD-3 diagnosis ICH Physical Examination. A complete physical and neurologic examination is in order: • Blood pressure, supine and standing with 2-minute interval between them • Height and weight • Head circumference (all children) • Eyes: Palpate for tenderness; check discs for papilledema, movements • Ears: Patency of canals, normal tympanic membranes • Neck: Palpate muscles; check range of motion for nuchal rigidity • Sinuses (frontal and maxillary) • Teeth (percuss, inspect) • Temporomandibular joints (mouth and jaw): Palpate and check range of motion • Thyroid gland • Bones and muscles of skull: Palpate for tenderness; listen for cranial bruits; check range of motion of cervical spine • Extremities: Tandem gait • Nerves: Palpate supraorbital, trochlear, occipital nerves; assess CN IX to CN XII• Reflexes: Pronator drift test (Romberg) • Vision screen Clinical Findings History. Headache diaries may be used to gather history and track symptoms over time. Important questions to ask the child and parent(s) include: Duration: Recent severe onset is worrisome. Frequency and triggers: Children with recurrent, low-intensity headaches, with no neurologic changes, and who recover completely between episodes are unlikely to have serious intracranial etiology. Triggers can include ovulation or menstruation, exercise, food or odors, and stress. Other triggers can include chocolate, processed meats, aged cheeses, nuts, altered amounts of caffeine intake, dairy products, shellfish, and some dried fruits. Consistent findings such as perimenstrual exacerbation, food triggers, and a stable pattern to the headache with intervals of wellness over a long time period are reassuring symptoms that suggest a primary headache. 686In most cases, a specific trigger or etiology is not ever identified. Location: Occipital or consistently localized headaches can indicate underlying pathology. Facial pain might be sinusitis. Ocular motor imbalance can produce a dull periorbital discomfort, whereas temporomandibular joint pain tends to localize around the periauricular or temporal areas. Quality and severity of pain: Sharp, throbbing, or pounding pain is vascular (migraine). Dull and constant pain may be tension or organic. Severity can be assessed by asking about limitations to activities and missed school days, although there are other factors that contribute to missed school and limited activities. How many “different kinds of headaches” are experienced? Age of onset: Progression of the headaches over time and longest period of time without symptoms. Home management and medication dosages, including dosage and self-management activities. Associated symptoms can include nausea, vomiting, visual changes, dizziness, paresthesia, neck/shoulder pain, back pain, otalgia, abdominal pain, hypersomnia, food cravings, confusion, ataxia, pallor, photophobia, and phonophobia. Changes in gait, personality, vision, mentation, or behavior that do not occur at the same time as the headache are worrisome and merit further evaluation with referral. There are some precursor symptoms and conditions that can indicate a predisposition to migraines. These include cyclic vomiting abdominal migraine and BPV. Alone, they do not warrant extensive or expensive workups unless the diagnosis is unclear. These conditions may evolve into migraine without aura in later childhood • Head trauma: If associated with headache, a subdural hematoma or postconcussive syndrome must be considered. • Psychologic symptoms: Evaluate for the presence of depression, school stressors, or concerns about family functioning. Additional things to consider include bullying or peer issues at school, “over programming” and family expectations, and meal, hydration, and sleep status. • Family history: Some children with headache, especially migraine, have a family history of headaches. Distinguishing Features of Headache Types . Headache has at least two of the following characteristics: 1. Bilateral location 2. Pressing/tightening (non-pulsating) quality 3. Mild or moderate intensity 4. Not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. No more than one of photophobia, phonophobia, or mild nausea 2. Neither moderate or severe nausea nor vomiting E. Not attributed to another ICHD-3 diagnosis Mitral Valve prolapseMitral valve prolapse (MVP) occurs when one of your heart's valves doesn't work properly. The flaps of the valve are "floppy" and don't close tightly. Most people who have the condition are born with it. It also tends to run in families. Most of the time, MVP doesn't cause any problems. Rarely, blood can leak the wrong way through the floppy valve. This can cause ● Palpitations (feelings that your heart is skipping a beat, fluttering, or beating too hard or too fast) ● Shortness of breath ● Cough ● Fatigue, dizziness, or anxiety ● Migraine headaches ● Chest discomfort Most people who have mitral valve prolapse (MVP) don't need treatment because they don't have symptoms and complications. If you need treatment for MVP, medicines can help relieve symptoms or prevent complications. Very few people will need surgery to repair or replace the mitral valve. MVP puts you at risk for infective endocarditis, a kind of heart infection. To prevent it, doctors used to prescribe antibiotics before dental work or certain surgeries. Now, only people at high risk of endocarditis need the antibiotics. Overview ● Aortic dissection and aortic aneurysm An aortic dissection is a serious condition in which the inner layer of the aorta, the large blood vessel branching off the heart, tears. Blood surges through the tear, causing the inner and middle layers of the aorta to separate (dissect). If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal. Aortic dissection is relatively uncommon. The condition most frequently occurs in men in their 60s and 70s. Symptoms of aortic dissection may mimic those of other diseases, often leading to delays in diagnosis. However, when an aortic dissection is detected early and treated promptly, the chance of survival greatly improves. Symptoms Aortic dissection symptoms may be similar to those of other heart problems, such as a heart attack. Typical signs and symptoms include:● Sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation, that radiates to the neck or down the back [Show More]
Last updated: 1 year ago
Preview 1 out of 67 pages
Instant download
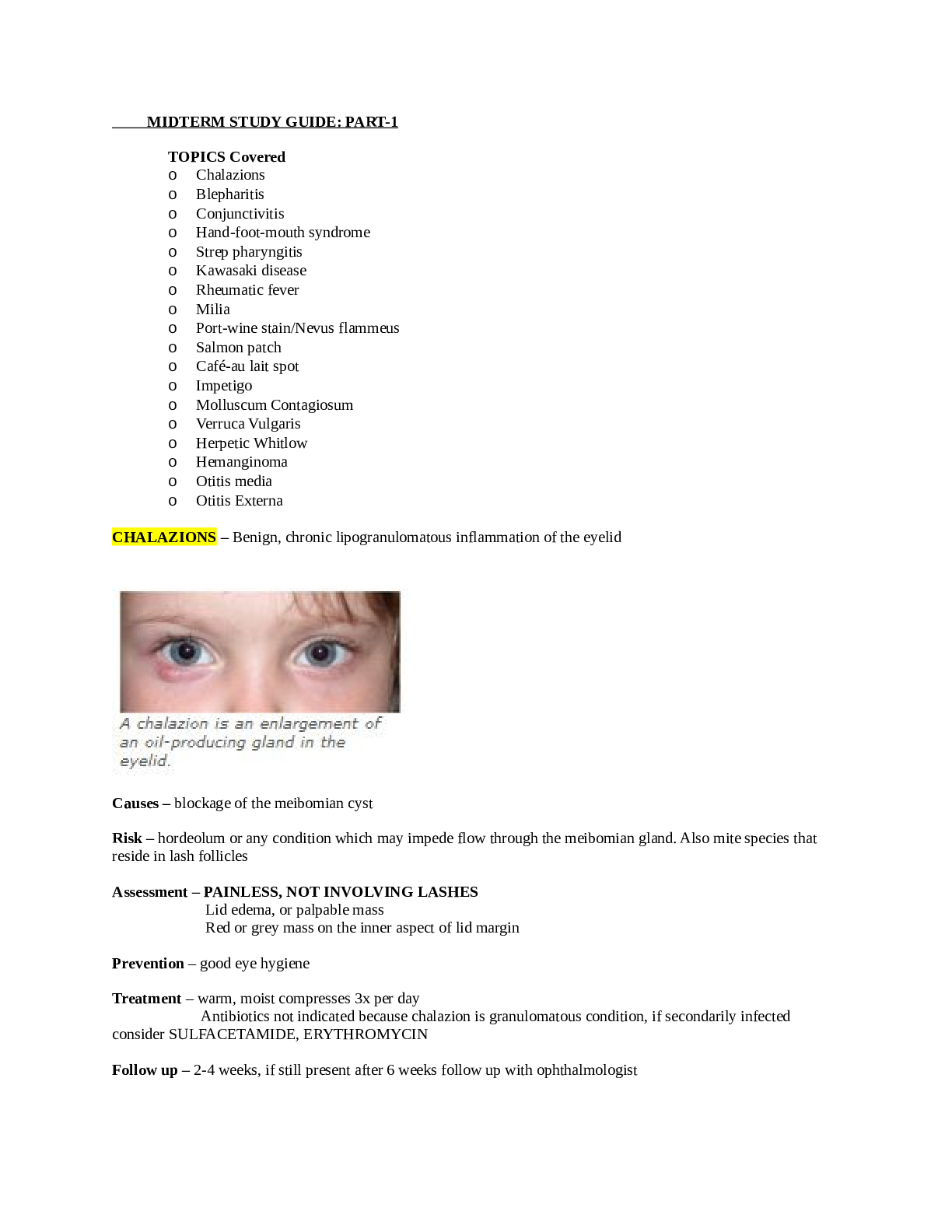
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
67
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
39


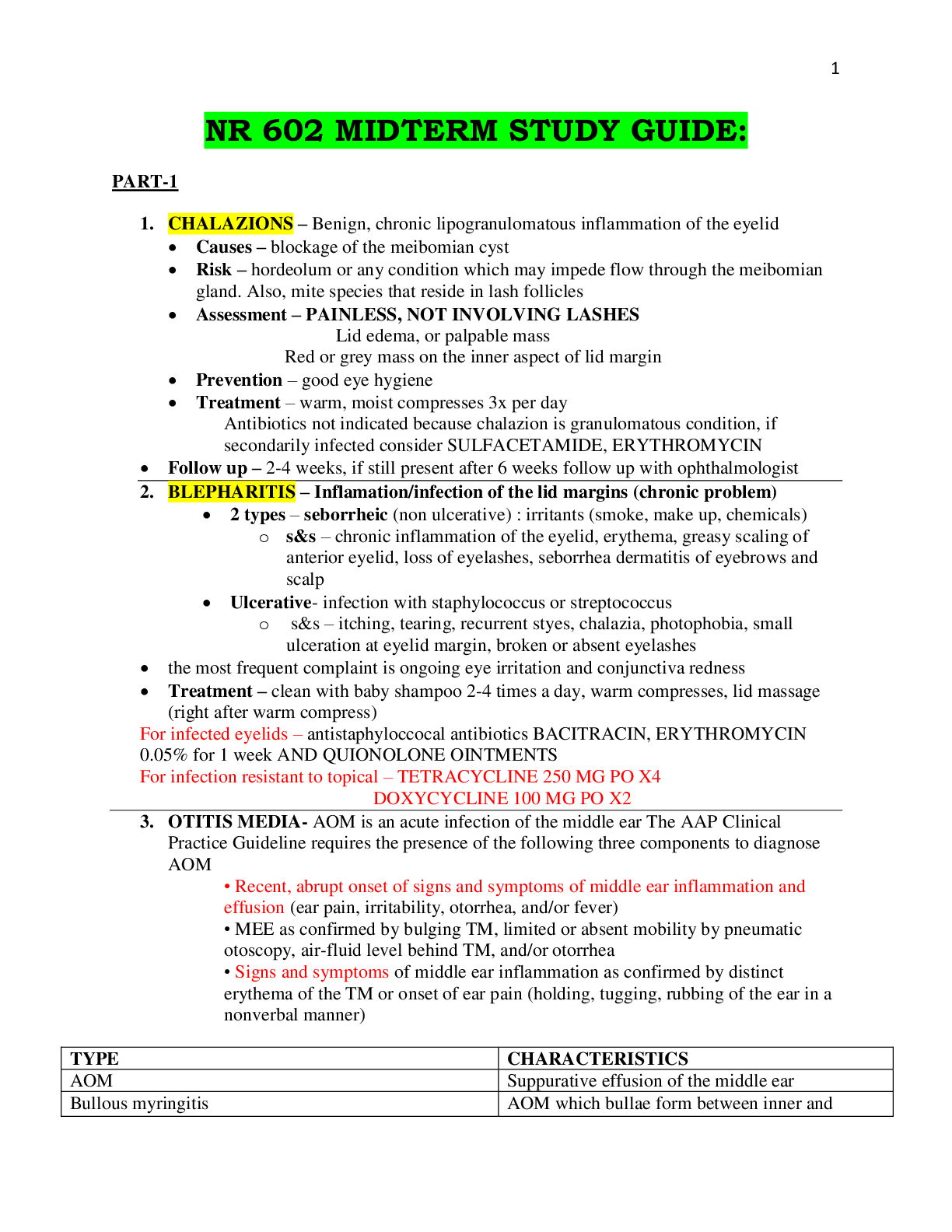
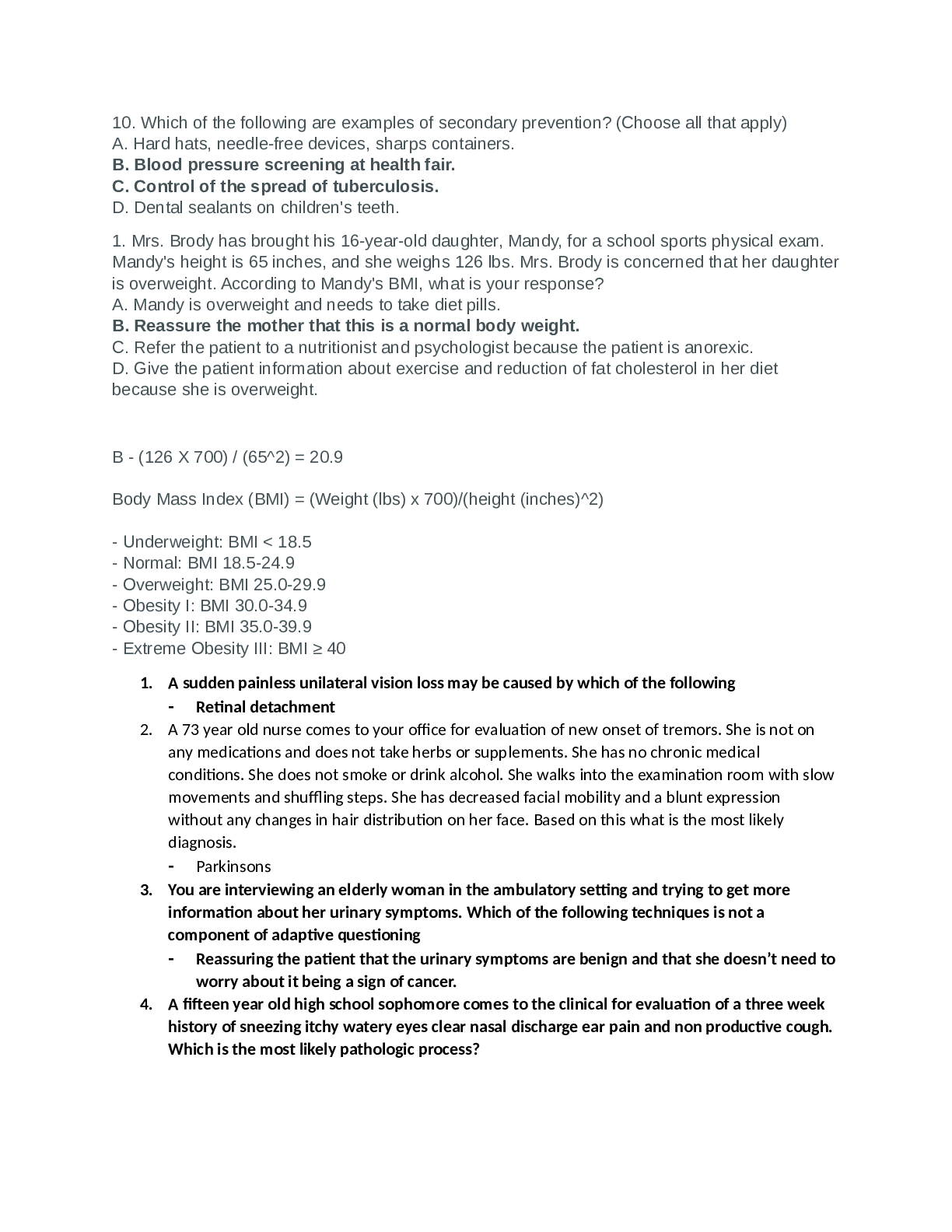
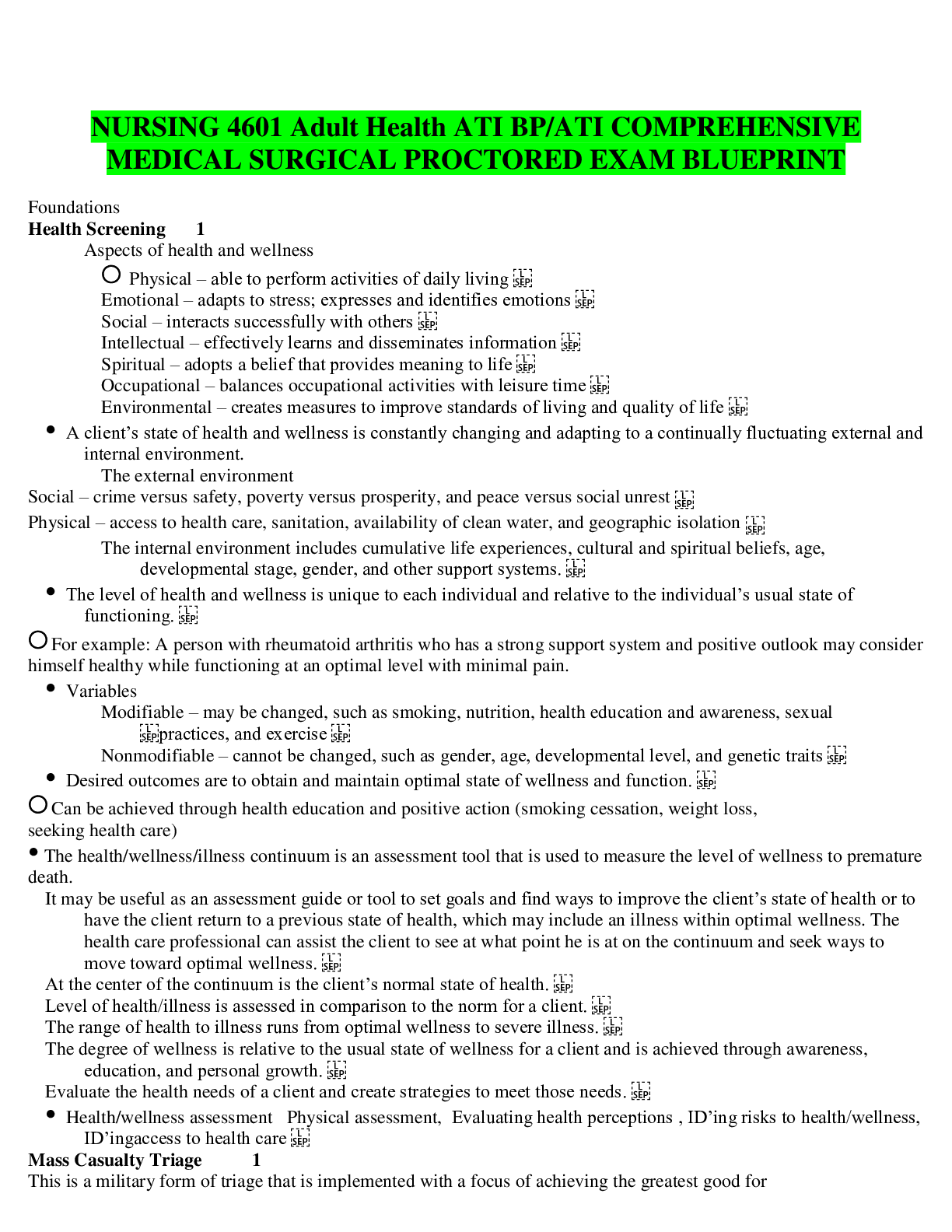
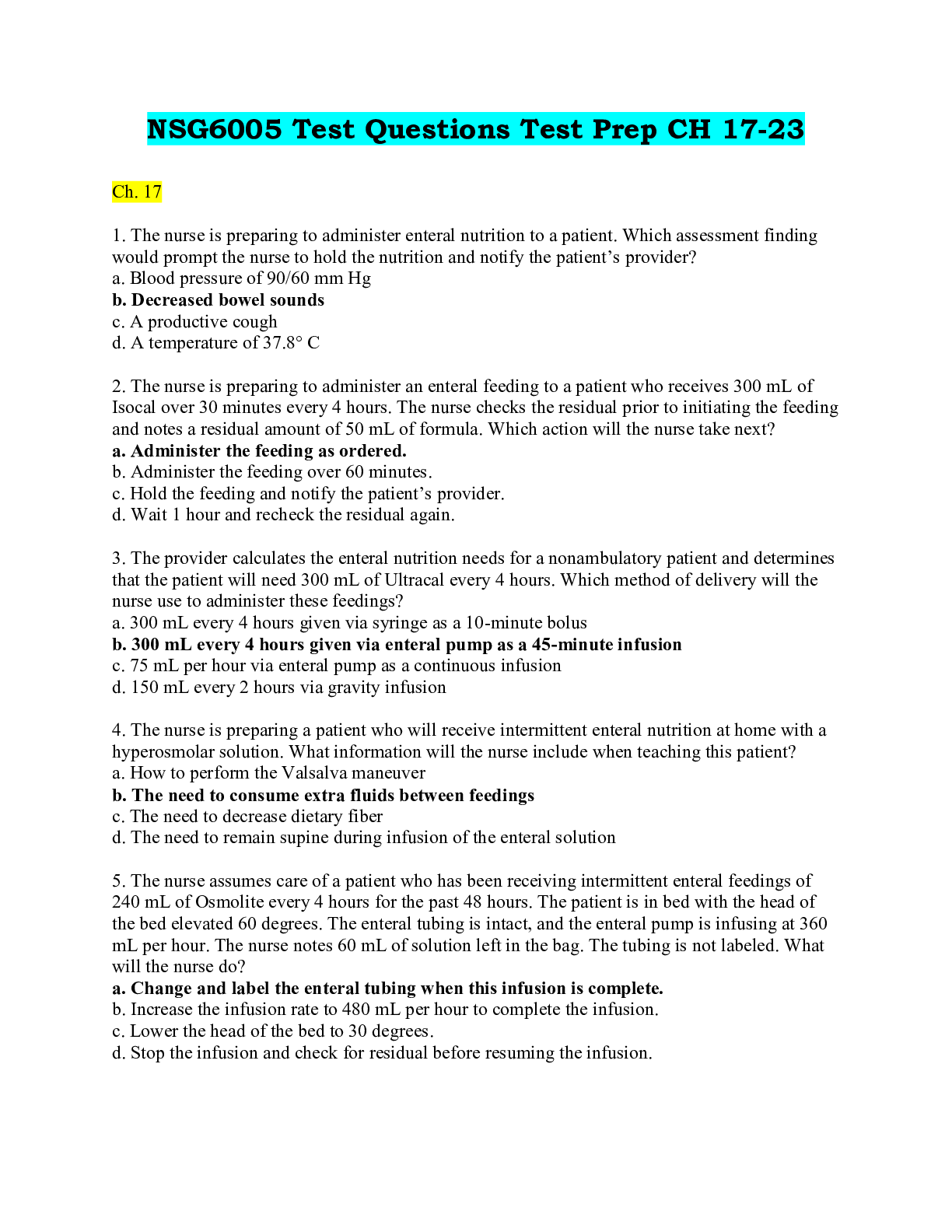
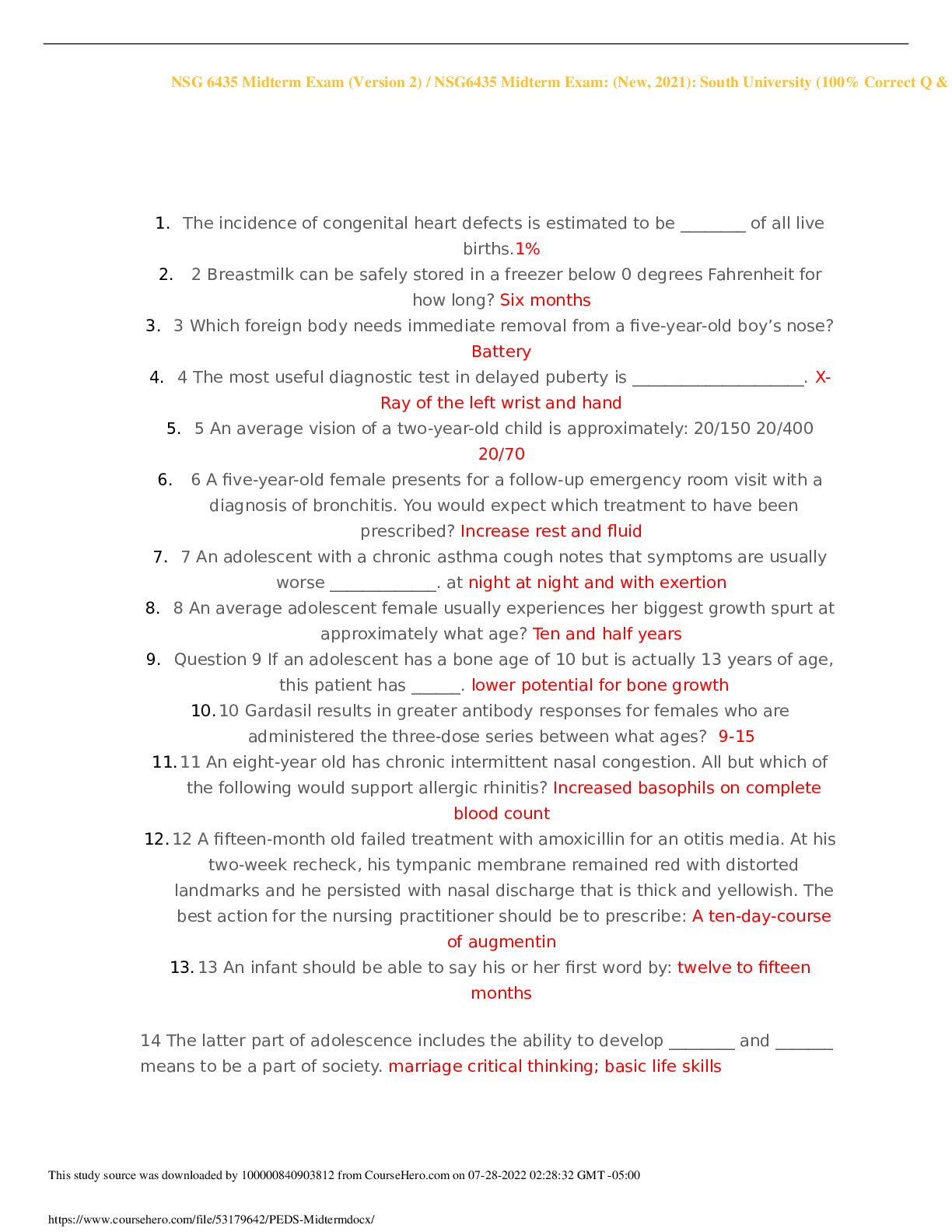
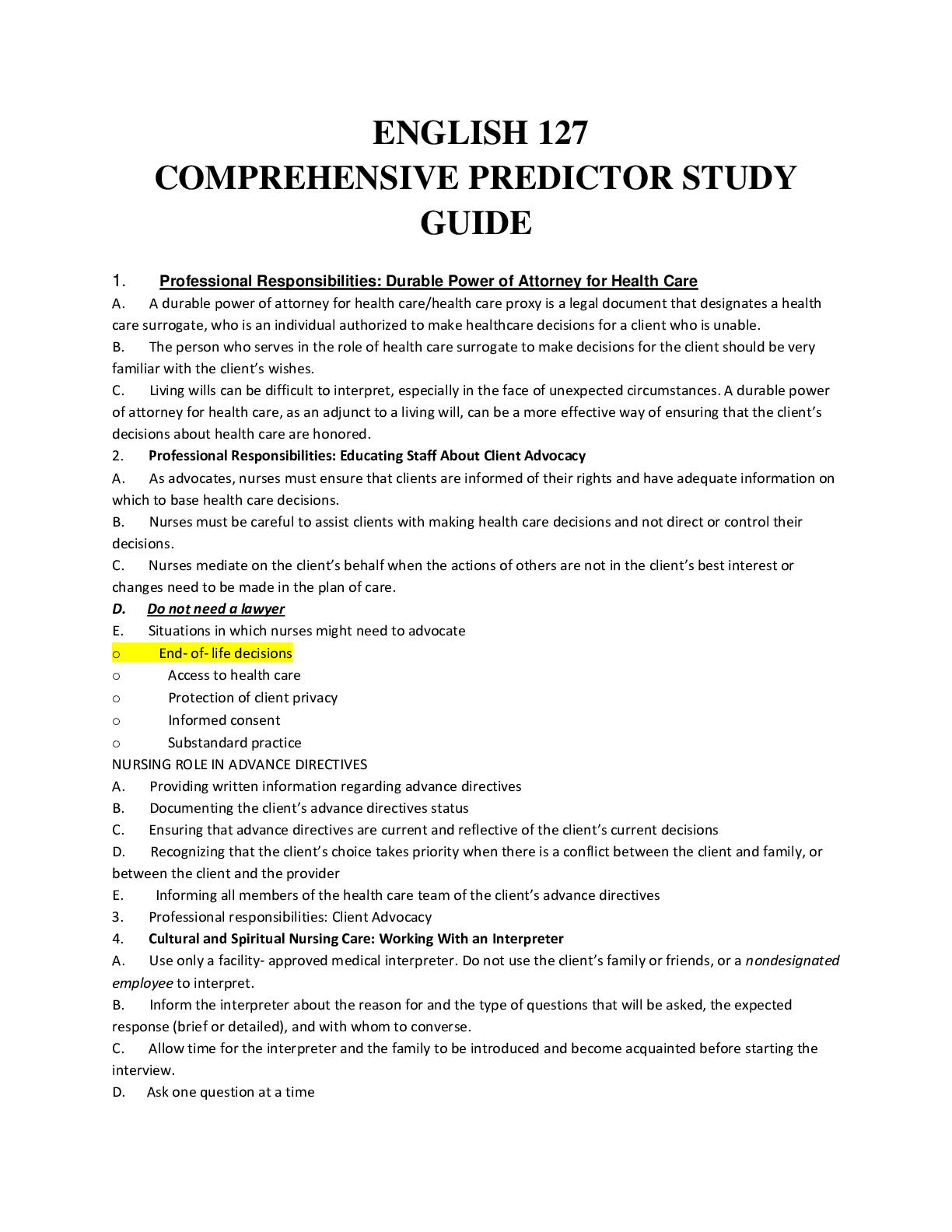
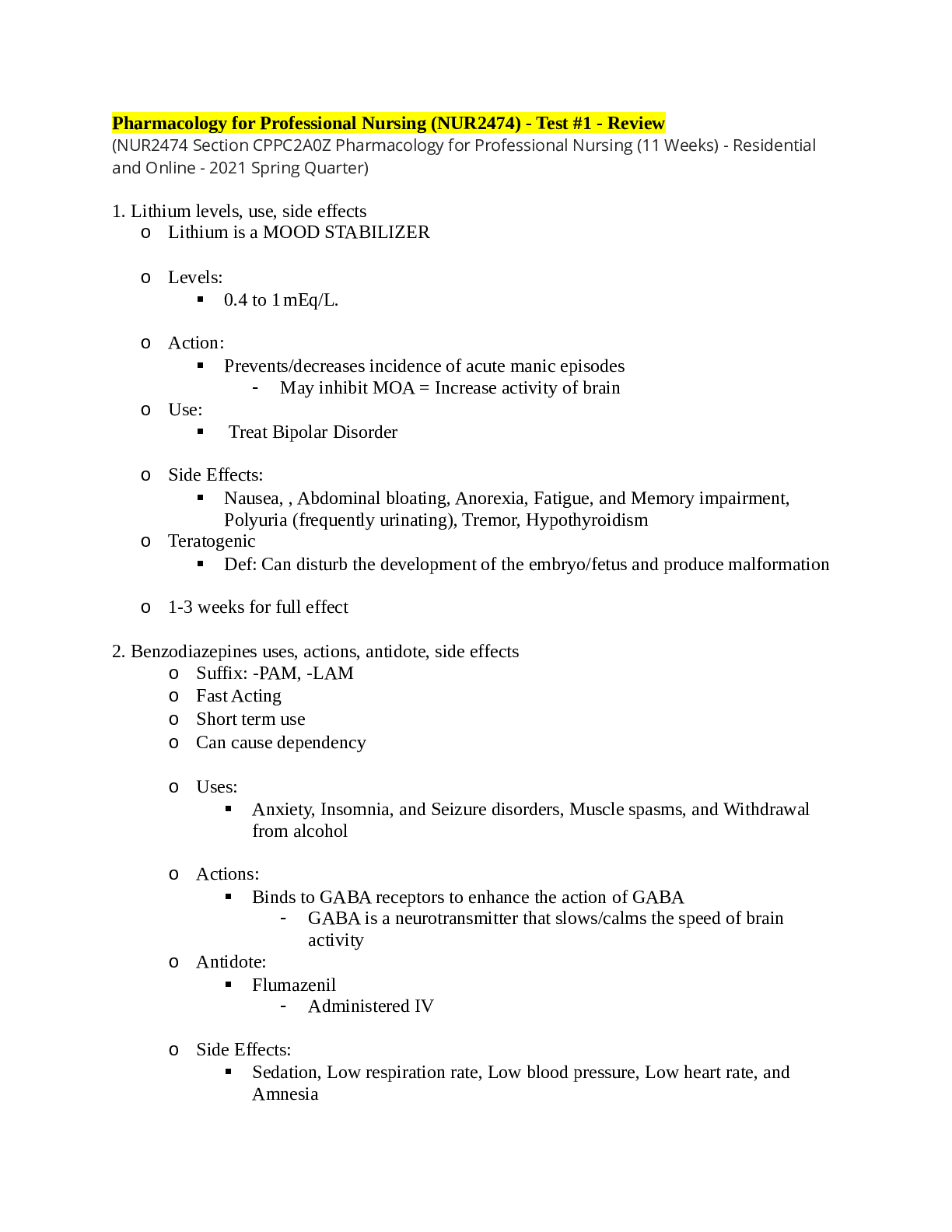
_2nd_E_Completed.png)