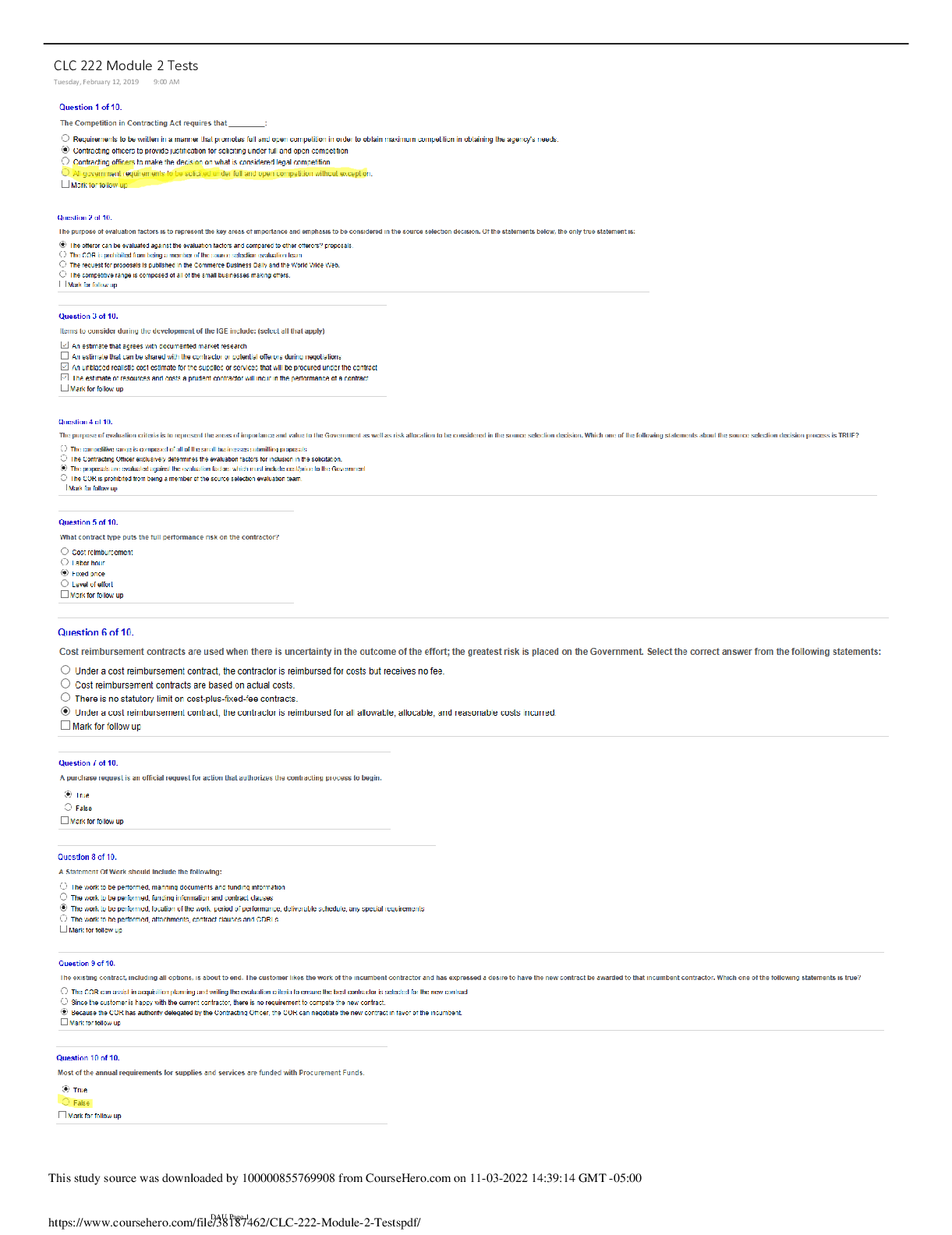
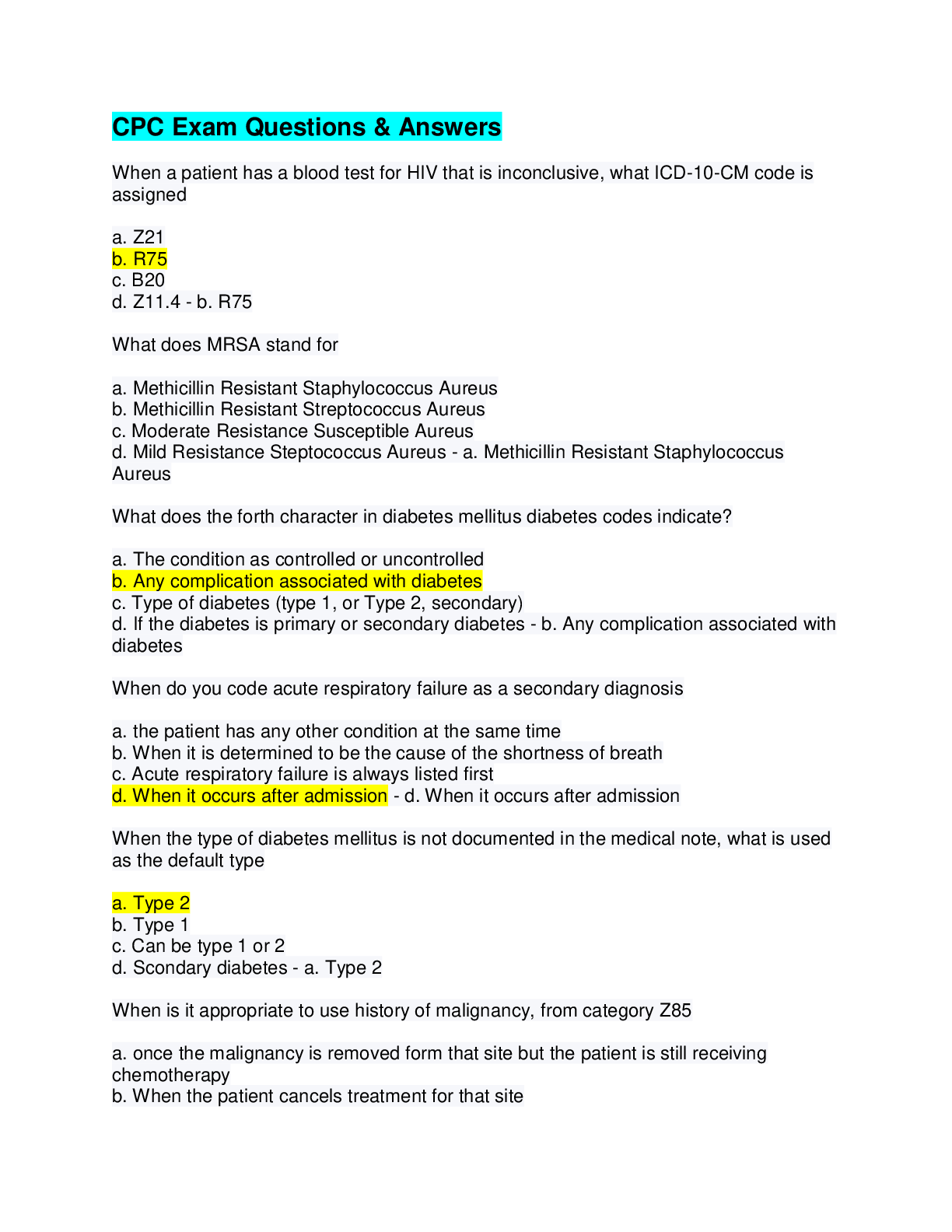
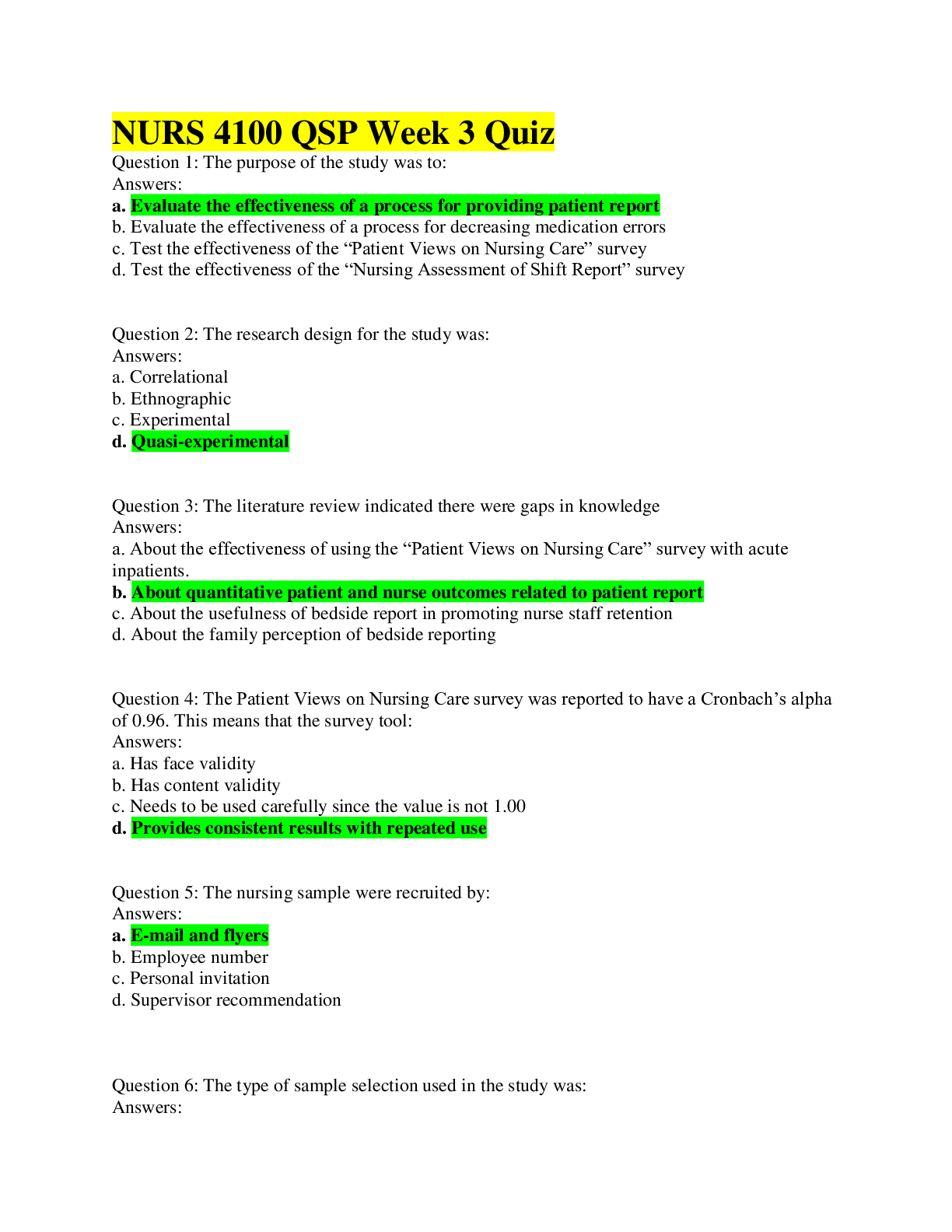
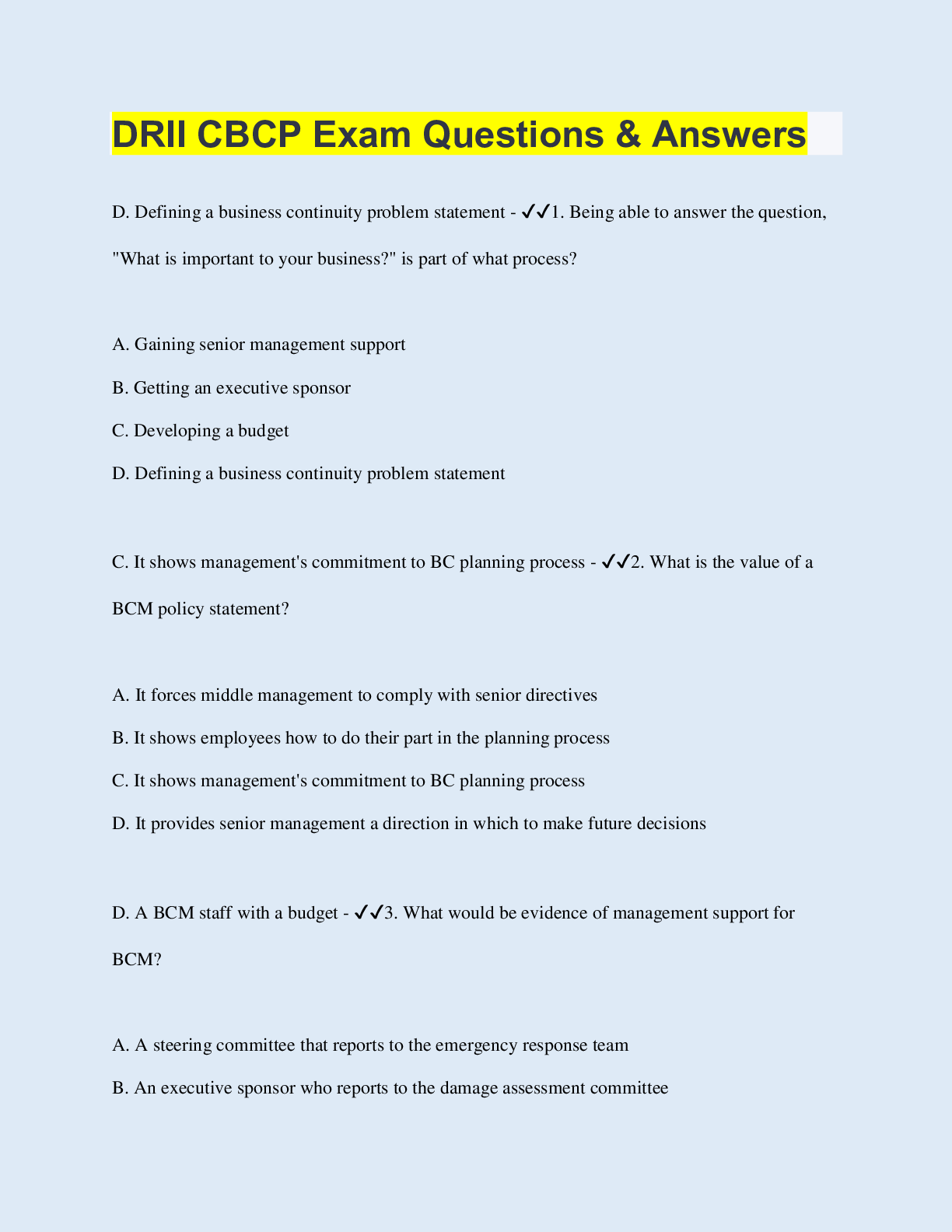
*NURSING > QUESTIONS & ANSWERS > NR 305 Health Assessment Patho Formative Review (Unit 1-6) Test bank questions & answers all 100% co (All)
NR 305 Health Assessment Patho Formative Review (Unit 1-6) Test bank questions & answers all 100% correct.
Document Content and Description Below
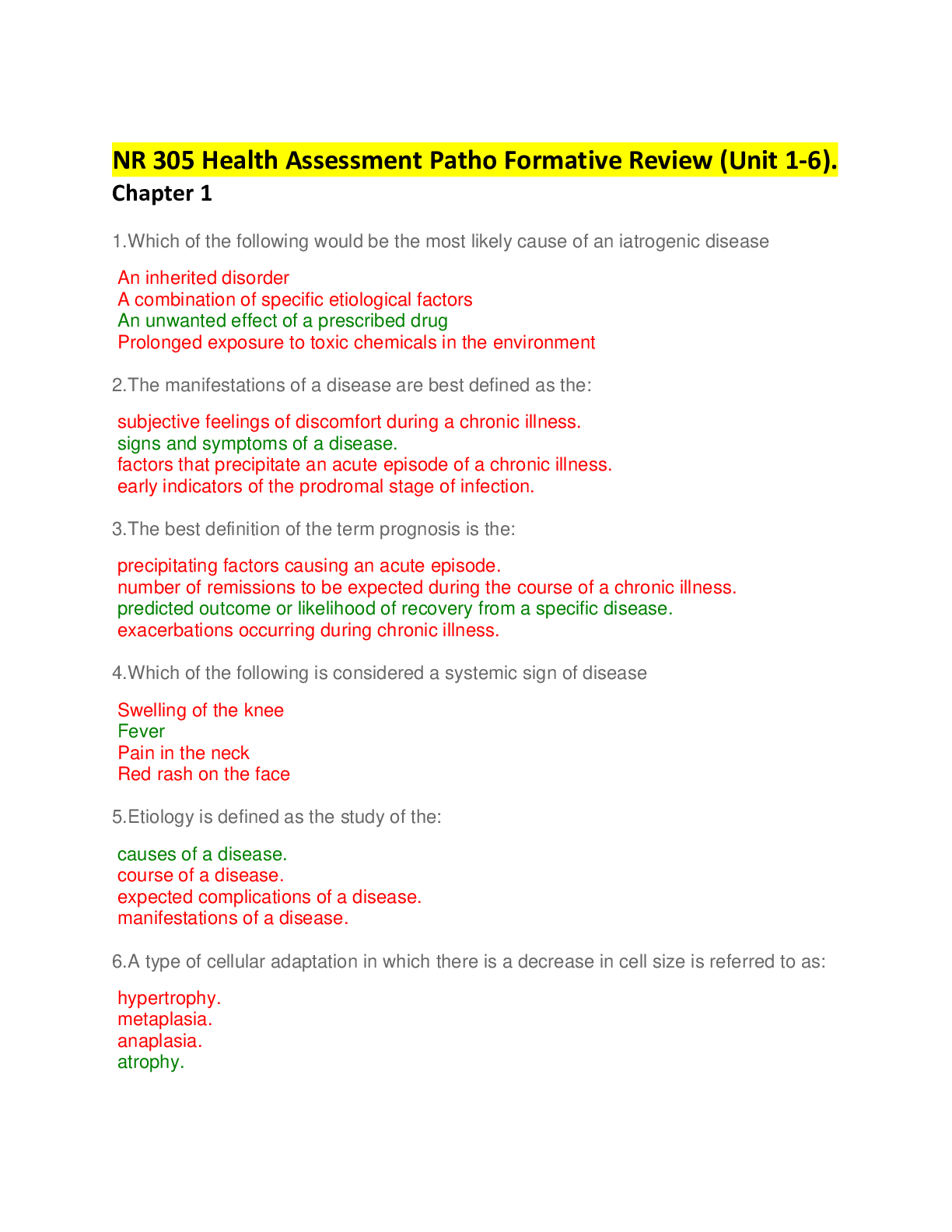
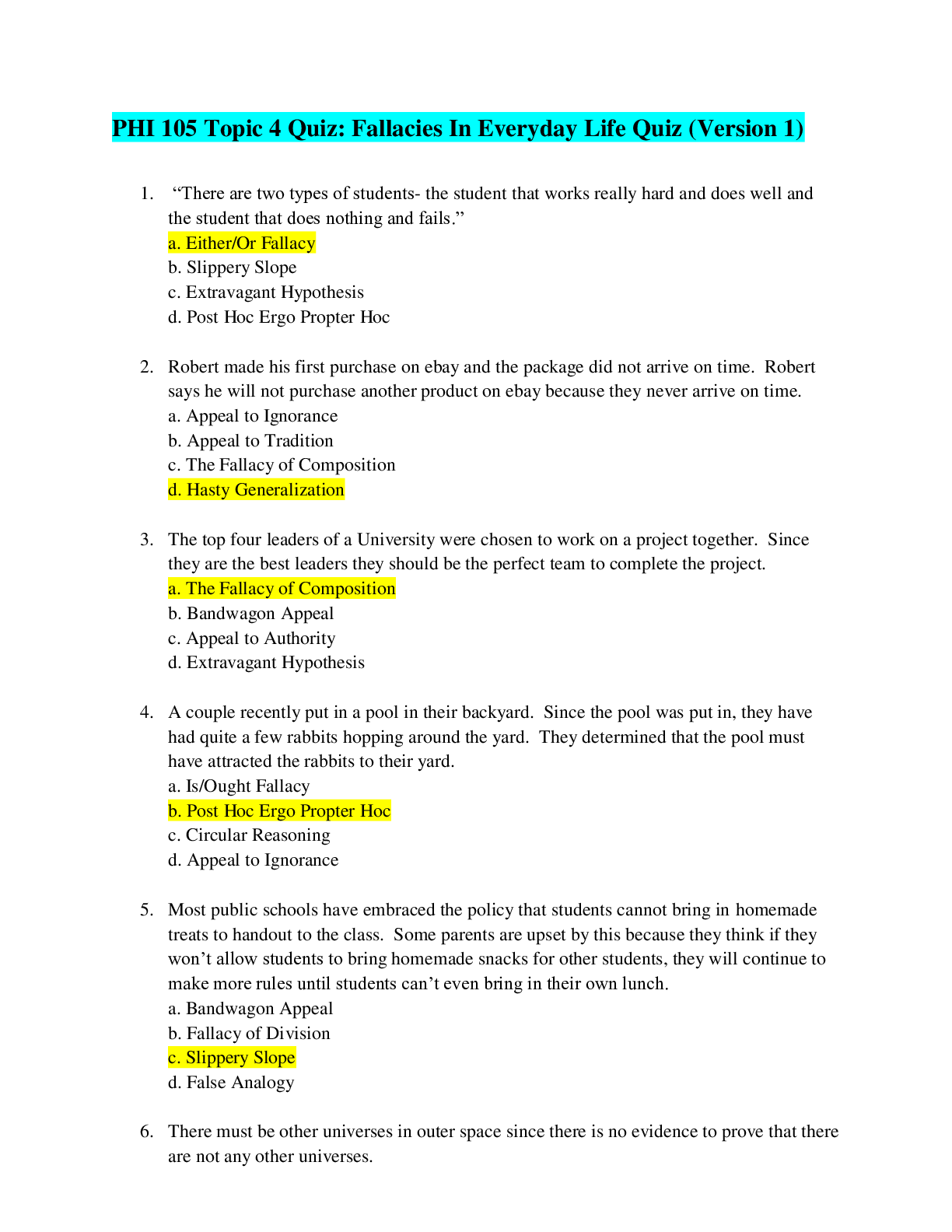
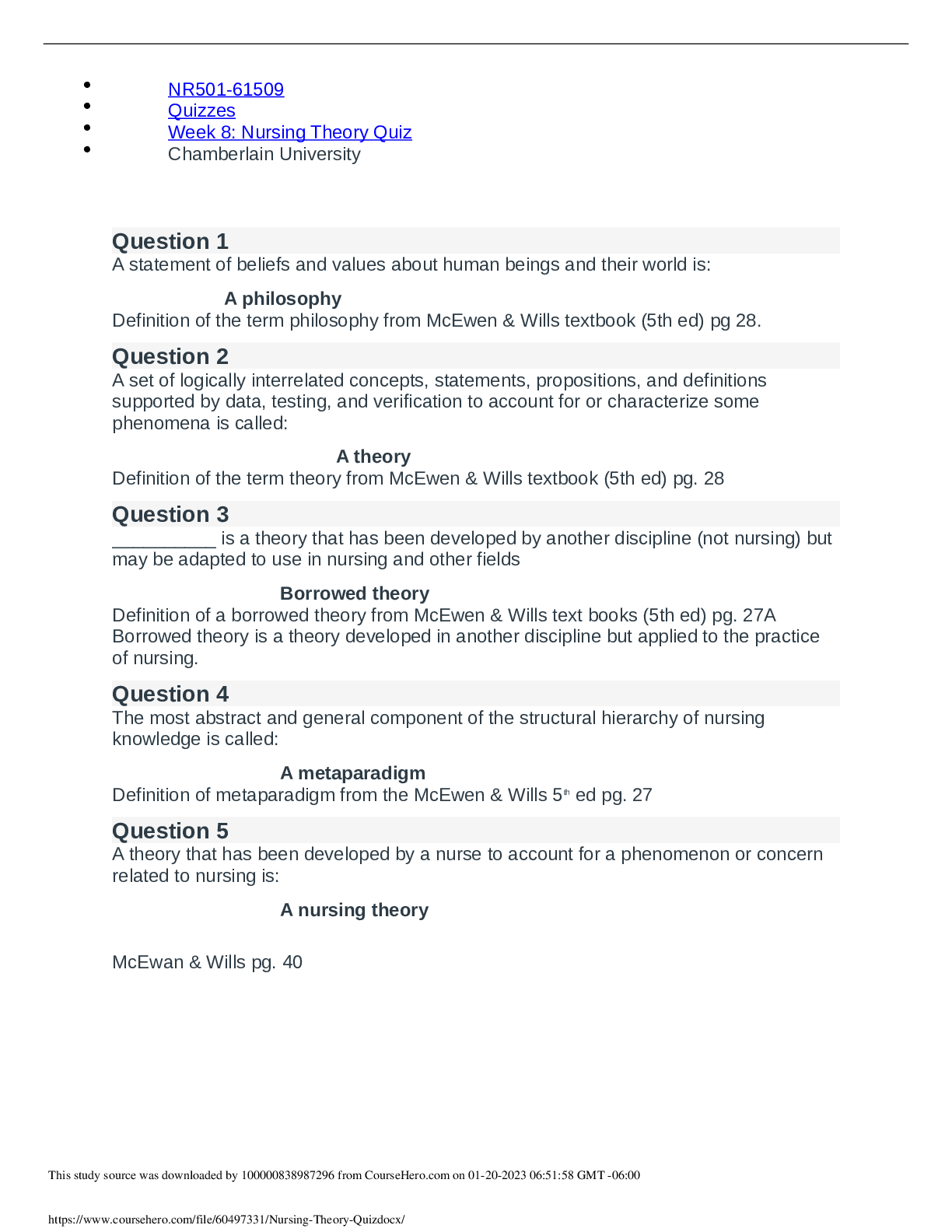
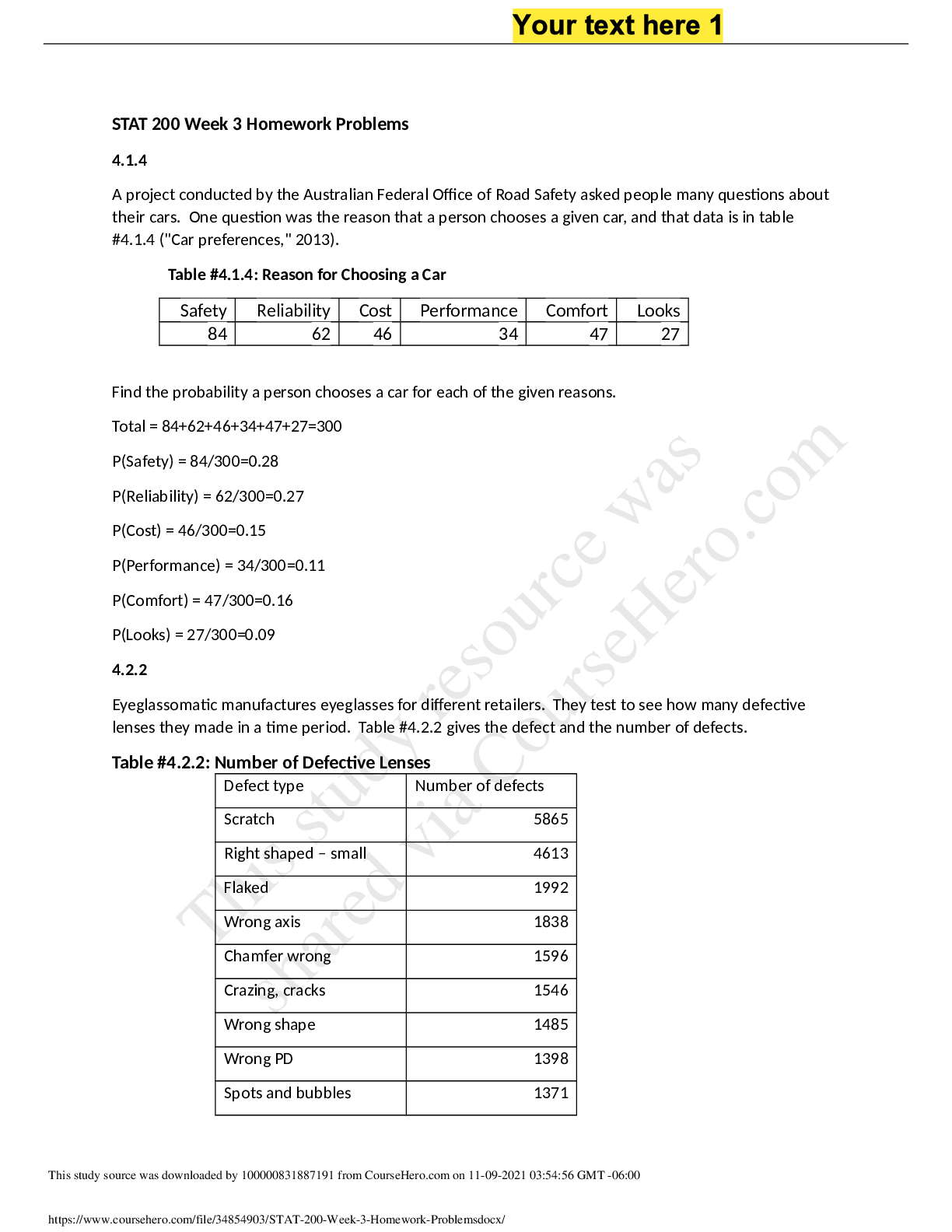
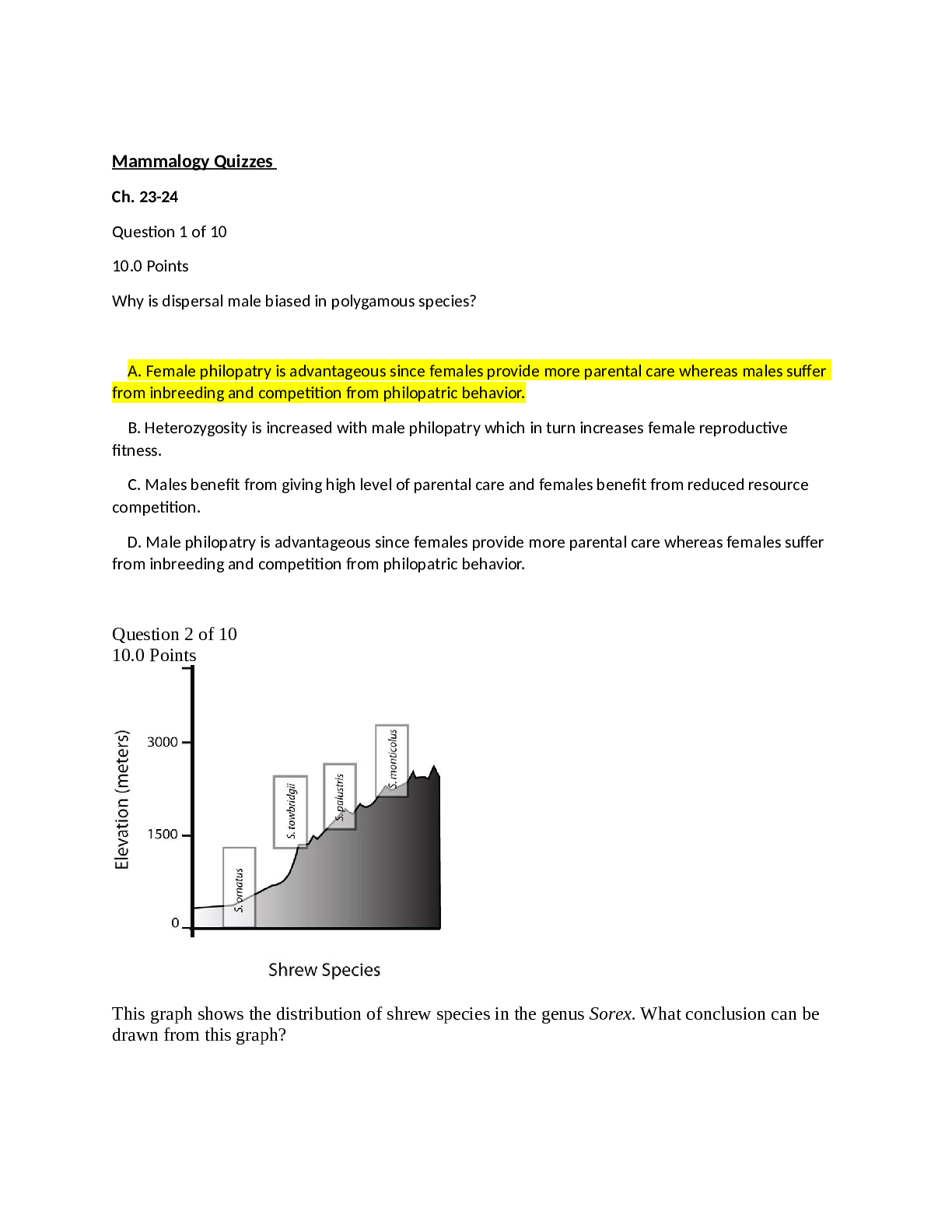
NR 305 Health Assessment Patho Formative Review (Unit 1-6). Chapter 1 1.Which of the following would be the most likely cause of an iatrogenic disease An inherited disorder A combination of sp... ecific etiological factors An unwanted effect of a prescribed drug Prolonged exposure to toxic chemicals in the environment 2.The manifestations of a disease are best defined as the: subjective feelings of discomfort during a chronic illness. signs and symptoms of a disease. factors that precipitate an acute episode of a chronic illness. early indicators of the prodromal stage of infection. 3.The best definition of the term prognosis is the: precipitating factors causing an acute episode. number of remissions to be expected during the course of a chronic illness. predicted outcome or likelihood of recovery from a specific disease. exacerbations occurring during chronic illness. 4.Which of the following is considered a systemic sign of disease Swelling of the knee Fever Pain in the neck Red rash on the face 5.Etiology is defined as the study of the: causes of a disease. course of a disease. expected complications of a disease. manifestations of a disease. 6.A type of cellular adaptation in which there is a decrease in cell size is referred to as: hypertrophy. metaplasia. anaplasia. atrophy. 7.A change in a tissue marked by cells that vary in size and shape and show increased mitotic figures would be called: metaplasia. atrophy. dysplasia. hypertrophy. 8.A deficit of oxygen in the cells usually due to respiratory or circulatory problems is called: apoptosis. ischemia. hypertrophy. necrosis. 9.When a group of cells in the body dies, the change is called: ischemia. gangrene. hypoxia. necrosis. 10.Rigorous weight lifting/body building regimens may result in the skeletal muscle cells undergoing: hypertrophy. dysplasia. atrophy. regeneration. 11.The term cancer refers to: dysplasia. hyperplasia. metaplasia. malignant neoplasm. 12.To which of the following does the term apoptosis refer Increased rate of mitosis by certain cells Ischemic damage to cells Liquefaction of necrotic tissue Preprogrammed cell self-destruction 13.Which of the following statements is TRUE Alteration of DNA does not change cell function. Damaged cells may be able to repair themselves. All types of cells die at the same rate. Mild ischemia causes immediate cell death. 14.Caseation necrosis refers to an area where: cell proteins have been denatured. cell are liquefied by enzymes. dead cells form a thick cheesy substance. bacterial invasion has occurred. 15.A circumstance that causes a sudden acute episode of a chronic disease to occur is termed: latent stage. predisposing factor. incidence. precipitating factor. 16.The term homeostasis refers to: the causative factors in a particular disease. maintenance of a stable internal environment. a condition that triggers an acute episode. a collection of signs and symptoms. 17.Pathophysiology involves the study of: the structure of the human body. the functions of various organs in the body. functional or structural changes resulting from disease processes. various cell structures and related functions. 18.Which of the following is the best definition of epidemiology The science of tracking the occurrence and distribution of diseases The relative number of deaths resulting from a particular disease Identification of a specific disease through evaluation of signs and symptoms The global search for emerging diseases 19.All of the following are part of the Seven Steps to Health EXCEPT: follow cancer screening guidelines. use sun block agents whenever exposed. participate in strenuous exercise on a regular daily basis. choose high fiber, lower fat foods. 20.A collection of signs and symptoms, often affecting more than one organ or system, that usually occur together in response to a certain condition is referred to as a (an): acute disease. multiorgan disorder. syndrome. manifestation. 21.All of the following statements are correct about cell damage EXCEPT: The initial stage of cell damage often causes an alteration in metabolic reactions. If the factor causing the damage is removed quickly, the cell may be able to recover and return to its normal state. If the noxious factor remains for an extended period of time, the damage becomes irreversible and the cell dies. Initially, cell damage does not change cell metabolism, structure, or function. 22.A short-term illness that develops very quickly with perhaps a high fever or severe pain is called: acute. latent. chronic. manifestation. 23.When prolonged ischemia occurs to an area of the heart, the resulting damage is referred to as: atrophy. liquefactive necrosis. apoptosis. infarction. 24.During the evaluation process for a new therapy’s effectiveness and safety, a double blind study may be conducted during: the first stage. the second stage. the third stage. 25.Cell damage may be caused by exogenous sources such as: abnormal metabolic processes. certain food additives. genetic defects. localized hypoxia. 26.A situation when there is a higher than expected number of cases of an infectious disease within a given area is called a/an: epidemic. exacerbation. morbidity. pandemic. 27.The term pathogenesis refers to: the development of a disease or sequence of events related to tissue changes involved in the disease process. the determination of the cause(s) involved in the development of a malignant neoplasm. the specific signs and symptoms involved in the change from an acute disease to a chronic disease. the changes in cells of affected tissue that result in necrosis. Chapter 2 1.Choose the correct proportion of water to body weight to be expected in a healthy male adult’s body: 30% 45% 60% 70% 2.Choose the correct proportion of blood (to body weight) in an adult male’s body: 30% 20% 10% 4% 3.Insensible fluid loss refers to water lost through: perspiration only. feces only. perspiration and expiration. urine and feces. 4.When the osmotic pressure of the blood is elevated above normal, water would shift from the: blood into the cells. interstitial compartment into the cells. interstitial compartment into the blood. cells into the interstitial compartment. 5.Which of the following would result from a deficit of plasma proteins Increased osmotic pressure Decreased osmotic pressure Increased hydrostatic pressure Decreased hydrostatic pressure 6.Which of the following terms refers to a combination of decreased circulating blood volume combined with excess fluid in a body cavity Dehydration Third-spacing Hypovolemia Water retention 7.Which of the following is a common cause of hyponatremia Loss of the thirst mechanism Excessive sweating Excessive aldosterone secretion Prolonged period of rapid, deep respirations 8.Which of the following is a common effect of both hypokalemia and hyperkalemia Skeletal muscle twitch and cramps Oliguria Elevated serum pH Cardiac arrhythmias 9.Choose the correct effect of increased parathyroid hormone. Increased movement of calcium ions into the bones Increased activation of vitamin D Increased absorption of calcium from the digestive tract Decreased reabsorption of calcium in the kidneys 10.Which of the following causes tetany Increased permeability of nerve membranes due to low serum calcium Excess calcium ions in skeletal muscle due to excess parathyroid hormone (PTH) Excess calcium ions inside somatic nerves as a result of neoplasms Increased stimulation of the nerves in the cerebral cortex 11.In which of the following processes is phosphate ion NOT a major component Bone metabolism Metabolic processes involving adenosine triphosphate (ATP) Blood clotting Acid-base balance 12.When many excess hydrogen ions accumulate in the blood, what happens to serum pH The pH: decreases. increases. remains constant. varies based on metabolism. 13.What is the slowest but most effective control for acid-base balance Respiratory system Buffer systems in the blood Kidneys Brain 14.Which of the following is essential in order to maintain serum pH within normal range Carbonic acid and bicarbonate ion must be present in equal quantities. All excess carbonic acid must be excreted by the kidneys. The concentration of bicarbonate ion must remain constant. The ratio of carbonic acid to bicarbonate ion must be 1:20. 15.Which condition is likely to cause metabolic acidosis Slow, shallow respirations Prolonged diarrhea Mild vomiting Excessive fluid in the body 16.What is the effect on blood serum when excessive lactic acid accumulates in the body Bicarbonate ion levels decrease Bicarbonate ion levels increase Carbonic acid levels increase pH increases 17.The direct effects of acidosis are manifested primarily in the functioning of the: Digestive system Urinary system Nervous system Respiratory system 18.Compensation mechanisms in the body for dehydration would include: increased antidiuretic hormone (ADH). decreased aldosterone. slow, strong heart contraction. peripheral vasodilation. 19.Which acid-base imbalance results from impaired expiration due to emphysema Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis 20. In patients with impaired expiration associated with emphysema, effective compensation for the acid-base imbalance would be: increased rate and depth of respiration. decreased rate and depth of respiration. increased urine pH and decreased serum bicarbonate. decreased urine pH and increased serum bicarbonate. 21.One of the factors involved in the increased need for water in infants is: proportionally smaller body surface area. higher metabolic rate. smaller respiratory capacity. greater surface area of exposed mucous membranes. 22.Compensation for respiratory system depression due to anesthesia and sedation would be: decreased reabsorption of bicarbonate ions in the kidneys. increased secretion of hydrogen ions into the filtrate. increased respiratory rate and depth. increased renin secretion. 23.A prolonged state of metabolic acidosis often leads to: hypokalemia. hyperkalemia. hyponatremia. hypercalcemia. 24.Strenuous physical exercise on a hot day is likely to result in: hypokalemia. hypernatremia. hyperchloremia. hypovolemia. 25.Which of the following is a manifestation of respiratory alkalosis Bradycardia and deep rapid breathing Drowsiness and general lethargy Increased nervous system irritability Decreased urine pH 26.Which two ions are most important for acid-base balance in the body K+, Na+ Cl– and HCO3– Ca++, Na+ Na+, Cl– 27.Alkalosis increases irritability and spontaneous stimulation of nerves by: blocking normal nerve conduction. increasing the permeability of nerve membranes. blocking movement of calcium ions. decreasing phosphate ion levels. 28.Which of the following is the primary control of serum Na+ levels ADH Aldosterone Serum H+ levels serum K+ levels 29.What are the three mechanisms that control or compensate for serum pH Hypothalamus, metabolic changes by digestive system, lymphatic system filtration Buffer pairs in blood, change in kidney excretion rate, change in respiration rate Neural feedback, increase in heart rate, decrease in calcium intake Modification of water intake, increased capillary permeability, decrease in blood volume 30.Increased milk and/or antacid intake can contribute to development of “milk-alkali syndrome,” which can cause which of the following Hyponatremia Hyperkalemia Hypercalcemia Hypovolemia Chapter 21 1.Which of the following statements applies to the sex chromosomes They are identified as XY in the female. They are numbered pair 23 in the karyotype. They contain the same genes as in the other pairs of chromosomes. They are found only in the cells in the gonads (the ovaries and the testes). 2.What is the term for an arrangement of the chromosomes from an individual’s cell, organized in pairs based on size and shape Pedigree Punnett squares Karyotype 3.What is characteristic of a congenital disorder Genes are not involved. It is strictly a developmental anomaly. A cause is known. It is usually manifested in the neonatal period. 4.What is the probability of two parents, both carriers of a defective recessive gene, producing a homozygous child (with each pregnancy) 0% 25% 50% 75% 5.In the case of an X-linked recessive disorder, a carrier mother and unaffected father could produce a/an: normal female. affected female. male carrier. 6.What is an example of a multifactorial congenital disorder Type AB blood Down syndrome Color blindness Cleft lip and palate 7.Which of the following statements regarding Down syndrome is TRUE The typical physical characteristics are present at birth. All children with Down syndrome have the same organ defects and medical problems. The extent of cognitive impairment can be assessed at birth. The birth of a child with Down syndrome is only a risk to mothers over age 35. 8.Which of the following statements applies to Huntington’s disease The effects are obvious at birth. There is a test for the defective gene. There is a 50% probability that the child of an affected parent will be a carrier. The child must inherit the defective gene from both parents in order to be affected. 9.Hemophilia A has been diagnosed in a young boy. He has inherited this defective gene from: his father. his mother. both parents. 10.A father affected with hemophilia A, whose wife is unaffected, will pass on the defective gene to: all of his sons, who will be affected. 50% of his sons, who will be affected. all of his daughters, who will be carriers. 50% of his daughters, who will be carriers. 11.A person with sickle cell trait that is heterozygous has: an incomplete dominant gene. a multifactorial condition. co-dominant genes. X-linked dominant trait. 12.Which term refers to prenatal diagnosis through examination of amniotic fluid Chorionic villus testing Preparing a family pedigree Amniocentesis Triple-screen test 13.The purpose of the Human Genome Project was to: map the nucleotide sequence and identify the genes on each human chromosome. study the common patterns of inheritance of single-gene disorders. manipulate the sequence of DNA in microorganisms and animals. identify spontaneous alterations in genetic material caused by teratogens. 14. Genes located at the same site on a pair of homologous chromosomes that are also matched for function are called: alleles. genotypes. autosomes. phenotypes. 15.Blood tests are performed on neonates primarily to: determine need for immediate surgical correction of anomalies. identify disorders requiring immediate treatment. identify the presence of any inherited disorders. rule out the presence of any infection. 16.The cellular division process that produces the chromosomes that are in the sperm and ova is called: meiosis. mitosis. organogenesis. polysomy. Chapter 5 1.A specific defense for the body is: phagocytosis. sensitized T lymphocytes. the inflammatory response. intact skin and mucous membranes. 2.Chemical mediators released during the inflammatory response include: albumin and fibrinogen. growth factors and cell enzymes. macrophages and neutrophils. histamine and prostaglandins. 3.Granulation tissue is best described as: highly vascular, very fragile, and very susceptible to infection. an erosion through the wall of viscera, leading to complications. a type of adhesion with no vascularization. a form of stenosis, in a duct, that is extremely tough and resists attack by microbes. 4.Which of the following statements applies to fever Viral infection is usually present. Heat-loss mechanisms have been stimulated. It is caused by a signal to the thalamus. It results from release of pyrogens into the circulation. 5.Mechanisms to bring an elevated body temperature down to the normal level include: general cutaneous vasodilation. generalized shivering. increased heart rate. increased metabolic rate. 7.Scar tissue consists primarily of: granulation tissue. epithelial cells. collagen fibers. new capillaries and smooth muscle fibers 8.Glucocorticoids are used to treat inflammation because they directly: promote the release of prostaglandins at the site. decrease capillary permeability. mobilize lymphocytes and neutrophils. prevent infection. 9.Patients taking glucocorticoids for long periods of time are likely to develop all of the following EXCEPT: decreased bone density. wasting of skeletal muscle. opportunistic infections. increased leukocyte production. 10.The characteristic appearance of a full-thickness burn is: painful with multiple blisters. heavy bleeding. red with some swelling. dry, firm, charred, or hard white surface 11.A typical source of infection in burn areas is: the skin grafts. microbes surviving in the hair follicles in the burn area. circulating blood bringing microbes to the burn wound. opportunistic virus in digestive tract. 12.A large burn area predisposes to decreased blood pressure because: bleeding occurs under the burn surface. the heart is damaged by toxic materials from the burn. fluid and protein shift out of the blood. vasoconstriction occurs in the burn area. 13.During an inflammatory response, hyperemia is caused by: increased blood flow in the area. increased capillary permeability. irritation of sensory nerve endings by histamine. increased leukocytes in the area. 14.Purulent exudates usually contain: small amounts of plasma protein & histamine in water. red blood cells & all types of white blood cells. numerous leukocytes, bacteria, and cell debris. large amounts of water containing a few cells. 15.Isoenzymes in the circulating blood: are a type of plasma protein normally present in the circulating blood. often indicate the precise location of an inflammatory response. are normally released from leukocytes during the inflammatory response. are pyrogens, causing low-grade fever. 16.Application of ice to an injured knee reduces edema by: promoting return of lymph fluid. causing local vasoconstriction. increasing the rate of tissue repair. causing systemic vasodilation. 17.Healing of large areas of skin loss (including dermis and epidermis) would be most successful through: rapid mitosis and regeneration of skin layers. resolution of damaged cells in the area. covering the area with biosynthetic skin substitute. graft of fibrous tissue to the area. 18.Prostaglandins are produced from _______and cause ___________. activated plasma protein; increased capillary permeability mast cells; vasodilation and pain platelets; attraction of neutrophils, chemotaxis mast cell granules; activation of histamines and kinins 19.The number of neutrophils in the blood is increased significantly: during allergic reactions. during chronic inflammation. to produce antibodies. in order to promote phagocytosis. 20.An abscess contains: serous exudate. purulent exudate. fibrinous exudate. hemorrhagic exudate. 21.Nonspecific agents that protect uninfected cells against viruses are called: neutrophils. macrophages. interferons. Pyrogens 22.In normal capillary exchange, what is net hydrostatic pressure based on The difference between the hydrostatic pressure within the capillary, as compared with the hydrostatic pressure of the interstitial fluid The relative osmotic pressures in the blood and the interstitial fluid The difference between the hydrostatic pressure and osmotic pressure within the capillary The difference between the concentrations of blood cells, plasma proteins, and dissolved substances in the blood and the interstitial fluid 23.Systemic manifestations of inflammation include all EXCEPT: pyrexia. malaise. local swelling. anorexia. 24.Which of the following cellular elements found in the inflammatory response are responsible for phagocytosis Macrophages Basophils B lymphocytes T lymphocytes Eosinophils 25.Which chemical mediator is involved in prolonging the inflammatory response Bradykinin Histamine Leukotrienes Chemotactic factors 26.Potential complications after healing by scar formation include all the following EXCEPT: lack of sensory function in the area. contractures and adhesions. increased hair growth. keloid formation. 27.Which of the following statements regarding inflammation is incorrect Inflammation caused by an allergen or a burn will typically produce a serous exudate. Infection is one cause of inflammation. Inflammation is the body’s nonspecific response to tissue injury. Disorders are named using the ending -sarcoma to indicate inflammation. 28.Which of the following helps to localize and “wall off” the foreign material during an inflammatory response Lymphocytes Increased fluid Fibrinogen Antibodies 29.Identify the proper sequence in the healing process. A blood clot forms; granulation tissue grows into the gap; new blood vessels develop; phagocytosis of foreign material and cell debris occurs; and collagen fibers form a tight, strong scar. A blood clot forms; phagocytes remove foreign material and cell debris; granulation tissue grows into the gap; new blood vessels form; and collagen fibers promote formation of a tight, strong scar. Collagen fibers form in the damaged area; a blood clot forms; granulation tissue grows into the gap; angiogenesis takes place; and foreign material and cell debris are removed by phagocytes. Foreign material and cell debris are removed by phagocytes; a blood clot forms; granulation tissue grows into the gap; new blood vessels form; and collagen fibers grow and cross-link. 30.Which of the following is a serious potential complication found only with the anti-inflammatory COX-2 inhibitor drugs Increased risk of infection at the site of inflammation Reye’s syndrome developing in children and young adults Increased incidence of heart attacks Greatly delayed blood clotting Chapter 6 1.Bacteria that form an irregular cluster of spheres are called: bacilli. diplococci. staphylococci. streptococci. 2.A strict anaerobe requires which specific environment A dry environment An acidic medium Air at a temperature less than 61 F/16 C The absence of oxygen 3.What method do viruses use to replicate Binary fission Budding of a daughter cell from the parent viral cell Producing reproductive spores Using a host cell to produce and assemble components 4.Which of the following is a characteristic of rickettsia It is a very small gram-negative intracellular microbe. It exists in three forms. It causes sexually transmitted disease. It reproduces by budding. 5.Which of the following is a characteristic of resident or normal flora (microflora) It exists in all areas of the body. Different species inhabit various areas of the body. It is of no benefit to the human host. It consists only of bacteria. 6.The term nosocomial infection means: transmission involves an insect or animal host. acquired in a hospital or medical facility. transmitted by a fomite. spread by direct contact with secretions from an open lesion. 7.Opportunistic infection may develop when: pathogens enter the body but cannot colonize the site of entry. an imbalance occurs in the normal resident flora. host resistance increases, and the balance of resident flora is restored. contaminated food or water is unknowingly ingested. 8.Which of the following factors would NOT increase the virulence of a specific microbe Secretion of endotoxin Presence of a bacterial capsule Production of interferons Secretion of invasive enzymes 9.That time in the course of an infection when the infected person may experience a headache or fatigue and senses he or she is “coming down with something” is referred to as which of the following Subclinical period Eclipse period Prodromal period Presymptomatic period 10.A broad-spectrum bactericidal agent would be expected to: destroy many gram-positive and gram-negative bacteria. destroy all pathogenic microbes in contact with the agent. reduce the replication of many bacteria. inhibit the growth of most spores and acid-fast bacteria. 11.Secondary infection may occur with administration of antibacterial drugs because the: patient is allergic to the drug. balance of species in the resident flora is upset. mucosa of the stomach is irritated. infecting microbes spread to adjacent areas. 12.All of the following are mechanisms of antiviral drug action EXCEPT: interference with attachment to host cell. block assembly of viral particles. interference with mitosis. shedding of protein coat. 13.Secondary bacterial infections occur frequently during influenza epidemics primarily because: antiviral drugs lower host resistance. the virus causes extensive tissue inflammation and necrosis. respiratory droplets transmit infections. the viral infection is usually self-limiting. 14.The primary pathological effect of influenza virus is: destruction of the mucosa in the lower respiratory tract. replication of the virus in respiratory secretions. destruction of leukocytes and macrophages in the lungs. inflammation and necrosis of the upper respiratory epithelium. 15.Which of the following microbes is classified as an obligate intracellular parasite Fungus Bacterium Virus Protozoa 16.Prions cannot be cultured in a PETRI plate of media because: they take so long to grow. they require extensive amounts of specialized nutrients. they are proteinaceous particles, not living organisms. they are viruses that don’t grow on conventional media. 17.Which of the following does NOT directly determine the virulence of a microbe Capacity for opportunism Production of toxins Ability to mutate Invasive qualities 18.Inflamed tissue is likely to become infected because: the immune system is not effective in inflamed tissue. the increased fluid and protein in the inflamed area supports microbial growth. phagocytes cannot penetrate the inflamed areas. capillaries are less permeable in the affected area. 19.Drugs that are designed to inhibit or slow down growth of microbes but not necessarily kill them are considered: ineffective. bacteriostatic. narrow-spectrum. bactericidal. Chapter 7 1.Neutrophils: are phagocytic cells. produce histamine. produce antibodies. are elevated during an allergic response. 2.Which cells are required to process and present antigens from foreign material as the initial step in the immune response T–helper cells Macrophages Eosinophils Monocytes 3.Humoral immunity is mediated by: natural killer cells. T lymphocytes (T cells). B lymphocytes (B cells). 4.A secondary immune response differs from the primary immune response in that: it is more rapid than the primary response and results in higher antibody levels. it is slower than the primary response and doesn’t change the antibody levels. it occurs at the same time as the primary response but results in a decrease in antibodies. it only occurs in hyperallergic reactions and results in a decrease of antibodies. 5.When an allergen binds with IgE antibodies on mast cells, resulting in release of chemical mediators, this reaction is called: cytotoxic hypersensitivity. immune complex hypersensitivity. type I hypersensitivity. type IV hypersensitivity. 6.Which statement applies to contact dermatitis It occurs when IgE antibodies on the skin react with the causative substance. It may result from ingested foods. Urticaria (hives) gradually spread over the body. A type IV reaction occurs in affected areas. 7.Which of the following causes anaphylaxis A severe, systemic allergic reaction Type III hypersensitivity Cell-mediated hypersensitivity Immune complex deposits in many tissues 8.Following a positive HIV antibodies blood test and ELISA test, what is the test commonly used for confirmation Agglutination Double immunodiffusion test Western blot test Sedimentation rate test 9.Systemic lupus erythematosus is caused by: a chronic allergic condition. development of an immune-deficient state. a deficiency of T lymphocytes. immune complex deposits of antinuclear antibodies. 10.Distinguishing clinical features of systemic lupus erythematosus include: inflammation in multiple organs. lack of a specific diagnostic blood test. acute onset and nonprogressive course. typical skin rash on the chest and back. 11.Which of the following are the target cells for HIV Helper T lymphocytes (CD4 lymphocytes) B lymphocytes Natural killer cells Macrophages 12.A diagnosis of HIV positive means that: the number of T lymphocytes in the circulating blood is decreased. significant opportunistic infection is present in the body. the individual has AIDS. the virus and its antibodies are present in the blood. 13.Immunodeficiencies may result in an increased risk of infections by normally harmless microorganisms. These infections are referred to as: opportunistic. prophylactic. abnormal. transient. 14.Which of the following statements does NOT apply to major histocompatibility complex (MHC) proteins or molecules They are genes on chromosome 6. All members of a family have identical MHCs. They alert the immune system to virus-infected cells. A close match is essential for successful tissue transplants. 15.CD4-positive helper T cells function by: direct cytotoxic action. facilitating all immune system activity. producing immunoglobulins. inactivating allergens. 16.Host-versus-graft disease refers to: hyperacute rejection of tissue. T cells in grafted tissue attacking host cells. infection resulting from immunosuppression therapy. transplant rejection by the recipient’s immune system. 17.In cases of HIV infection, the “window period” refers to the time between: entry of the virus into the blood and the initial manifestations. entry of the virus into the body and the appearance of antibodies in the blood. entry of the virus into the body and a significant drop in CD4 T-helper lymphocyte count. diagnosis of “HIV positive” and diagnosis of “AIDS.” 18.The term tolerance refers to: surveillance and destruction of new cancer cells by the immune system. the ability of the immune system to ignore “self” cells. the ability of T and B lymphocytes to work together. the role of lymphoid tissue in the body defenses. 19.Which of the following statements applies to the complement system It is activated by IgE. It blocks the inflammatory response. It consists of proteins in the blood that must be activated. It may destroy antibodies in the circulation. 20.The most common cause of death in patients who have AIDS is: HIV encephalopathy. tuberculosis. Pneumocystis carinii pneumonia. Candida infection. 21.Tissue transferred between two genetically identical twins is referred to as a/an: allograft. syngraft. isograft. autograft. Chapter 20 1.What is a benign neoplasm originating from adipose tissue called Adenoma Lipoma Fibrosarcoma Adenocarcinoma 2.What are malignant neoplasms arising from connective tissue cells called Carcinomas Sarcomas Melanomas Fibromas 3.Which factor provides the basis for the grading of newly diagnosed malignant tumors Size of the tumor Number of metastases Degree of differentiation of the cells Number of lymph nodes involved 4.Which of the following does paraneoplastic syndrome refer to The effects of substances such as hormones secreted by the tumor cells Severe weight loss and cachexia associated with advanced cancer The decreased resistance to infection resulting from malignant tumors The effects of multiple metastatic tumors 5.Which term refers to the spread of malignant cells through blood and lymph to distant sites Invasiveness Seeding Metastasis Systemic effect 6.Radiation therapy destroys: all cells in the tumor at one time. the cells in the center of the tumor. primarily rapidly dividing cells. radioresistant cells. 7.The most critical adverse effects of chemotherapy and radiation therapy are: thrombocytopenia and leucopenia. headache and lethargy. nausea and constipation. alopecia and weight loss. 8.Select the correct pair representing a malignant tumor and its marker: colon cancer: carcinoembryonic antigen (CEA) hepatic cancer: CA125, AFP prostate cancer: human chorionic gonadotropin (hCG) testicular cancer: Philadelphia chromosome 9.Antiangiogenesis drugs act on a malignant tumor by: promoting the immune response and removal of abnormal tumor cells. blocking hormonal stimulation of tumor cells. reducing blood flow and nutrient supply to tumor cells. transporting radioisotopes into the tumor. 10.Identify the common dose-limiting factor for chemotherapy: Alopecia Bone marrow depression Nausea and vomiting Weight loss 11.Glucocorticoids are often prescribed during a course of chemotherapy and radiation because: glucocorticoids greatly potentiate the effect of chemotherapy. the immune system is stimulated. skeletal muscle atrophy will be decreased. inflammation around the tumor may be reduced. 12.What type of normal cells are often damaged during chemotherapy and radiation treatments Epithelial cells Skeletal muscle cells Nerve tissue Collagen and fibrous tissue 13.Remission for cancer is generally defined as a period in which: chemotherapy cannot be used. signs and symptoms are absent. complications are evident. metastases occur. 14.The term apoptosis refers to: programmed cell death. abnormal or immature cells. degree of differentiation of cells. the development of new capillaries in a tumor. 15.Drugs or agents that augment the natural immune response in the body to improve identification and removal of abnormal cells are called: biological response modifiers. angiogenesis stimulators. analgesic complements. targeted receptor modifiers. 16.The method that can be used as an alternative to surgical removal of a tumor by using heat generated by a needle inserted into the tumor is referred to as: radiation therapy. thermolysis intervention. brachytherapy. radiofrequency ablation. Chapter 8 1.Which of the following areas lacks blood vessels and nerves Epidermis Dermis Subcutaneous tissue Fatty tissue 2.What is a raised, thin-walled lesion containing clear fluid called Papule Pustule Vesicle Macule 3.Which of the following is a common effect of a type I hypersensitivity response to ingested substances Contact dermatitis Urticaria Discoid lupus erythematosus Psoriasis 4.Why do secondary infections frequently develop in pruritic lesions Loss of protective sebum Entry of resident flora while scratching the lesion Blockage of sebaceous glands Increased sweat production 5.Which disease is considered an autoimmune disorder Pemphigus Erysipelas Contact dermatitis Scleroderma 6.Which of the following skin lesions are usually caused by Staphylococcus aureus Furuncles Verrucae Scabies Tinea 7.Which of the following statements applies to impetigo Lesions usually appear on the hands and arms. The cause is usually a virus. The infection is highly contagious. Scar tissue is common following infection. 8.How are antiviral drugs effective in treating a viral infection They destroy the virus if administered for at least 2 weeks. They limit the acute stage and viral shedding. They prevent any systemic effects of viruses. They prevent any secondary bacterial infection. 9.Plantar warts are caused by: the fungus aspergillus. a parasitic arthropod. human papillomavirus. the bacterium Streptococcus pyogenes. 10.What causes the pruritus associated with scabies An allergic reaction to the causative microbe due to endotoxins Mites burrowing into the epidermis and reaction to their feces Bleeding and injected toxin from bites of the larvae Neurotoxins secreted by mites on the skin surface 11.What is the major predisposing factor to squamous cell carcinoma Viral infection Presence of nevi (moles) on the skin Exposure to ultraviolet light Frequent hypersensitivity reactions 12.Which of the following factors has contributed to the increased incidence of Kaposi’s sarcoma Excessive sun exposure Increased number of nevi Increase in immunosuppressed individuals Presence of more seborrheic keratosis 13.Which of the following applies to actinic keratoses They predispose to malignant melanoma. They arise on skin exposed to ultraviolet radiation. They occur primarily on dark-skinned persons. They are malignant and invasive. 14.Systemic effects of acute necrotizing fasciitis include: low-grade fever and malaise. toxic shock and disorientation. mild nausea and vomiting. headache and difficulty breathing. 15.The cause of contact dermatitis can often be identified by: using a culture and sensitivity test on the exudate. checking the frequency of the exacerbations. noting the location and size of the lesion. the type of pain associated with the lesion. 16.The pathological change associated with scleroderma is: abnormal activation of T lymphocytes and an increase of cytokines. an autoimmune reaction damaging the epidermis. collagen deposits in the small blood vessels of the skin and sometimes the viscera. Type I hypersensitivity and increased serum IgE levels. 17.Leprosy (Hansen’s disease) is caused by: a fungus. a bacterium. a virus. a helminth. 18.One factor that is responsible for increasing the mortality rate among patients suffering with necrotizing fasciitis is: a delay in initial diagnosis. lack of proper antibiotics. the appearance of additional opportunistic infections. secondary fungal infections. Chapter 13 1.Which of the following activities does NOT require muscle contractions and energy Quiet inspiration Forced inspiration Quiet expiration Forced expiration 2.The maximum volume of air a person can exhale after a maximum inspiration is termed the: expiratory reserve volume. inspiratory reserve volume. total lung capacity. vital capacity. 3.The central chemoreceptors in the medulla are normally most sensitive to: low oxygen level. low concentration of hydrogen ions. elevated oxygen level. elevated carbon dioxide level. 4.Oxygen diffuses from the alveoli to the blood because: PO2 is higher in the blood. PO2 is lower in the blood. CO2 is diffusing out of the blood. more CO2 is diffusing out of cells into the blood. 5.Carbon dioxide is primarily transported in the blood: as dissolved gas. attached to the iron molecule in hemoglobin. as bicarbonate ion. as carbonic acid. 6.What would be the most effective compensation for respiratory acidosis The kidneys eliminating more bicarbonate ions The kidneys producing more bicarbonate ions The kidneys reabsorbing more hydrogen ions An increase in respiratory rate 7.What is the acid-base status of a patient with the following values for arterial blood gases serum bicarbonate 36.5 mmol/L (normal range: 22-28) PCO2 75 mm Hg (normal range: 35-45) serum pH 7.0 Compensated metabolic acidosis Decompensated metabolic acidosis Compensated respiratory acidosis 8.Approximately what percentage of bound oxygen is released to the cells for metabolism during an erythrocyte’s journey through the circulatory system 80% 25% 10% 50% 9.Light bubbly or crackling breathing sounds associated with serous secretions are called: rhonchi. stridor. rales. wheezing. 10.What are early signs and symptoms of infectious rhinitis Purulent nasal discharge and periorbital pain Serous nasal discharge, congestion, and sneezing Copious purulent sputum, particularly in the morning Harsh barking cough and wheezing 11.What are typical signs and symptoms of epiglottitis Hyperinflation of the chest and stridor Hoarse voice and barking cough Sudden fever, sore throat, and drooling saliva Sneezing, mild cough, and fever 12.What is the most common cause of viral pneumonia Rhinovirus Influenza virus Haemophilus influenzae Pneumococcus 13.Which of the following describes lobar pneumonia Sudden onset of fever and chills, with rales and rusty sputum Insidious onset, diffuse interstitial infection Viral infection causing nonproductive cough and pleuritic pain Opportunistic bacteria causing low-grade fever with cough and thick greenish sputum 14.How does severe hypoxia develop with pneumonia Acidosis depresses respirations. Oxygen diffusion is impaired by the congestion. Inflammatory exudate absorbs oxygen from the alveolar air. Infection reduces effective compensation by the heart. 15.Rust-colored sputum in a patient with pneumonia usually indicates: secondary hemorrhage in the lungs. Streptococcus pneumoniae is the infecting agent. prolonged stasis of mucous secretions in the airways. persistent coughing has damaged the mucosa in the bronchi. 16.Select the statement related to tuberculosis: The microbe is present in the sputum of all patients with a positive TB skin test. The infection is transmitted primarily by blood from an infected person. TB is usually caused by an acid-fast bacillus, resistant to many disinfectants. The microbe is quickly destroyed by the immune response. 17.When does active (secondary) infection by Mycobacterium tuberculosis with tissue destruction occur When host resistance is decreased When a hypersensitivity reaction is initiated When the BCG vaccine is not administered immediately following exposure to the microbe When Ghon complexes form in the lungs 18.Histoplasmosis is caused by a: fungus. virus. bacillus. protozoa. 19.The basic pathophysiology of cystic fibrosis is centered on a/an: defect of the exocrine glands. impaired function of the endocrine glands. chronic inflammatory condition of the lungs. abnormal immune response in the lungs and other organs. 20.What is a common indicator of cystic fibrosis in the newborn Infant respiratory distress syndrome Failure to excrete meconium Taste of ammonia on the skin Lack of bile secretions 21.Why does hypercalcemia occur with bronchogenic carcinoma Invasion of the parathyroid gland by the tumor Secretion of parathyroid or parathyroid like hormones by the tumor Destruction of the ribs Failure of the kidney to excrete calcium ions 22.What is the pathophysiology of an acute attack of extrinsic asthma Gradual degeneration and fibrosis Continuous severe attacks unresponsive to medication A hypersensitivity reaction involving release of chemical mediators Hyperresponsive mucosa 23.What cause the expanded anteroposterior (A-P) thoracic diameter (barrel chest) in patients with emphysema Air trapping and hyperinflation Persistent coughing to remove mucus Recurrent damage to lung tissues Dilated bronchi and increased mucous secretions 24.Destruction of alveolar walls and septae is a typical change in: chronic bronchitis. acute asthma. emphysema. asbestosis. 25.What is the cause of chronic bronchitis Chronic irritation, inflammation, and recurrent infection of the larger airways A genetic defect causing excessive production of mucus Hypersensitivity to parasympathetic stimulation in the bronchi Deficit of enzymes, preventing tissue degeneration 26.Which of the following is typical of chronic bronchitis Decreased activity of the mucous glands Fibrosis of the bronchial wall Overinflation of bronchioles and alveoli Formation of blebs or bullae on the lung surface 27.What are typical pathological changes with bronchiectasis Bronchospasm and increased mucous secretion Adhesions and fibrosis in the pleural membranes Airway obstructions and weak, dilated bronchial walls Fixation of the ribs in the inspiratory position 28.Which of the following are significant signs of bronchiectasis Persistent nonproductive cough, dyspnea, and fatigue Persistent purulent nasal discharge, fever, and cough Chronic cough, producing large quantities of purulent sputum Wheezing and stridor 29.Why does cor pulmonale develop with chronic pulmonary disease The right ventricle pumps more blood than the left ventricle. Pulmonary fibrosis and vasoconstriction increase vascular resistance. Demands on the left ventricle are excessive. Blood viscosity is increased, adding to cardiac workload. 30.What is caused by frequent inhalation of irritating particles such as silica Fibrosis and loss of compliance Frequent bronchospasm Increased number of mucus-producing glands Distorted shape of the thorax 31.Pulmonary edema causes severe hypoxia because of: decreased diffusion of carbon dioxide from the alveoli. interference with expansion of the lungs. constant cough and hemoptysis. decreased recoil of lungs and ineffective expiration. 32.Which of the following is NOT a cause of pulmonary edema Left-sided congestive heart failure Excessive blood volume (overload) Inhalation of toxic gases Hyperproteinemia and increasing osmotic pressure of the blood 33.Which of the following is a common source of a pulmonary embolus Mural thrombus from the left ventricle Thrombus attached to atheromas in the aorta or iliac arteries Thrombus forming in the femoral veins A blood clot in the pulmonary vein 34.What is a large-sized pulmonary embolus likely to cause Hypertension and left-sided heart failure Atelectasis and respiratory failure Hypotension and right-sided heart failure Pleural effusion and atelectasis 35.How does a large pleural effusion lead to atelectasis The cohesion between the pleural membranes is disrupted. There is decreased intrapleural pressure. The mediastinal contents compress the affected side. Pleuritic pain causes very shallow breathing. 36.When does flail chest usually occur An open puncture wound involves the pleural membranes. The visceral pleura is torn by a fractured rib. Several ribs are fractured at two sites. Increasing fluid in the pleural cavity causes atelectasis. 37.Which of the following is a manifestation of a simple closed pneumothorax Decreased respiratory rate Tracheal deviation toward the unaffected lung Asymmetrical chest movements Increased breath sounds on the affected side 38.Which of the following is an effect of a large open pneumothorax (sucking wound) Mediastinal flutter, impairing venous return Increased venous return Progressive atelectasis of both lungs Overexpansion of the unaffected lung 39.With a tension pneumothorax, which factors contribute to severe hypoxia Decreasing compression of the inferior vena cava More air leaving the pleural cavity on expiration than entering with inspiration Shift of the mediastinal contents toward the affected lung Continually increasing pressure on the unaffected lung 40.Laryngotracheobronchitis is typically manifested by: drooling and difficulty swallowing. hoarse voice and barking cough. sore and scratchy throat with fever. wheezing and dyspnea. 41.Lobar pneumonia is usually caused by: Mycoplasma pneumoniae. Streptococcus pneumoniae. Legionella pneumophila. Pneumocystis carinii. 42.Severe acute respiratory syndrome (SARS) is caused by a/an: rhinovirus. mycoplasma. influenza virus. coronavirus. 43.Which of the following is a significant early sign of bronchogenic carcinoma in a smoker Frequent nonproductive cough Fever, dyspnea, generalized aching Production of large volumes of purulent sputum Hemoptysis and weight loss 44.Which of the following would confirm a diagnosis of primary tuberculosis A positive tuberculin skin test Occurrence of hemoptysis Unproductive cough with absence of sputum Small areas of calcification on a chest X-ray 45.Choose the correct reason for severe hypoxia occurring with pulmonary edema: Diffusion of oxygen into the alveoli is impaired. Fluid in the pleural cavity prevents normal lung expansion. Increased concentration of CO2 impairs diffusion of oxygen. Increased blood flow through the lungs prevents diffusion of gases. 46.Primary atypical pneumonia (PAP) is caused by: Klebsiella oxytoca. Candida albicans. Mycoplasma pneumoniae. Streptococcus pneumoniae. 47.Which factor usually causes metabolic acidosis to develop in association with hypoxia Anaerobic metabolism Failure to excrete CO2 Liver dysfunction Increased blood volume Chapter 10 1.What term is used to describe a deficit of all types of blood cells Leucopenia Neutropenia Pancytopenia Erythrocytosis 2.Capillary walls consist of: multiple endothelial layers. a thick layer of smooth muscle. two or three epithelial layers. a single endothelial layer. 3.Vitamin K is required by the liver to synthesize: heparin. prothrombin. amino acids. bilirubin. 4.Individuals with type O blood are considered to be universal donors because their blood: contains A and B antibodies. contains A and B antigens. lacks A and B antibodies. lacks A and B antigens. 5.What is the cause of sickle cell anemia A defective gene inherited from both parents A chronic bacterial infection Bone marrow depression An autoimmune reaction 6.Which of the following best describes the characteristic erythrocyte associated with pernicious anemia Hypochromic, microcytic Normochromic, normocytic Elongated, sickle-shaped Megaloblastic or macrocytic nucleated cells 7.Jaundice is one typical sign of: sickle cell anemia. aplastic anemia. iron deficiency anemia. acute leukemia. 8.Which of the following is present with pernicious anemia Pancytopenia Hypochlorhydria Leukocytosis Multiple infarcts 9.Why do abnormally low hemoglobin values develop with pernicious anemia Decreased production of erythrocytes Shorter life span of erythrocytes Abnormal structure of hemoglobin chains Deficit of folic acid 10.What are the common early signs of aplastic anemia Painful joints and skeletal deformity Abdominal discomfort and splenomegaly Excessive bleeding and recurrent infections Palpitations and chest pain 11.Which of the following applies to sickle cell trait Most hemoglobin is in the form of HgS Sickling of erythrocytes occurs with severe hypoxia. Painful sickling crises with multiple infarctions occur frequently. A child’s skeletal growth is delayed. 12.In individuals with pernicious anemia, antibodies form to: vitamin B12. intrinsic factor or parietal cells. mucus-producing glands. hydrochloric acid. 13.Which statement applies to the disorder hemophilia A It is transmitted as an X-linked dominant trait. There is usually a total lack of factor VIII in the blood. Males and females can be carriers. Hematomas and hemarthroses are common. 14.Which of the following substances acts as an anticoagulant Prothrombin Heparin Fibrinogen Vitamin K 15.Multiple opportunistic infections develop with acute leukemia primarily because: the number of white blood cells is decreased. many circulating leukocytes are immature. severe anemia interferes with the immune response. decreased appetite and nutritional intake reduce natural defenses. 16.Predisposing factors to leukemia commonly include: exposure to radiation. certain fungal and protozoal infections. familial tendency. cigarette smoking. 17.Multiple myeloma is a malignant tumor involving: plasma cells. granulocytes. bone cells. lymph nodes. 18.Which of the following statements applies to hemochromatosis. It is: caused by excessive iron intake in the diet. results from excessive hemolysis of RBCs. a metabolic error that leads to excess amounts of hemosiderin, causing damage to organs. an inherited defect that results in abnormal hemoglobin. 19.All of the following apply to vitamin K EXCEPT: it is used as an antidote for warfarin (Coumadin). the liver requires it to produce prothrombin. it is a fat-soluble vitamin. the bone marrow requires it to synthesize hemoglobin. 20.In which blood dyscrasia does pancytopenia develop Pernicious anemia Aplastic anemia Iron deficiency anemia Sickle cell anemia Chapter 12 1.Which of the following actions causes the atrioventricular (AV) valves to close Increased intraventricular pressure Depolarization at the AV node Ventricular relaxation and backflow of blood Contraction of the atria 2.Which of the following describes the pericardial cavity It contains sufficient fluid to provide a protective cushion for the heart. It is a potential space containing a very small amount of serous fluid. It is lined by the endocardium. It is located between the double-walled pericardium and the epicardium. 3.The function of the baroreceptors is to: stimulate the parasympathetic or sympathetic nervous system at the sinoatrial (SA) node as needed. adjust blood pressure by changing peripheral resistance. sense a change in blood oxygen and carbon dioxide levels. signal the cardiovascular control center of changes in systemic blood pressure. 4.Which of the following is a result of increased secretion of epinephrine Increased heart rate and force of contraction Decreased stimulation of the SA node and ventricles Vasoconstriction in skeletal muscles and kidneys Vasodilation of cutaneous blood vessels 5.The event that causes the QRS wave on an electrocardiogram (ECG) tracing is: atrial depolarization. atrial repolarization. ventricular depolarization. ventricular repolarization. 6.The cardiac reserve is: afterload. the difference between the apical and radial pulses. the ability of the heart to increase cardiac output when needed. the extra blood remaining in the heart after it contracts. 7.Vasodilation in the skin and viscera results directly from: decreased blood pressure. increased parasympathetic stimulation. relaxation of smooth muscle in the arterioles. increased stimulation of alpha-adrenergic receptors. 8.A partial obstruction in a coronary artery will likely cause: pulmonary embolus. hypertension. angina attacks. myocardial infarction. 9.Cigarette smoking is a risk factor in coronary artery disease because smoking: reduces vasoconstriction and peripheral resistance. decreases serum lipid levels. promotes platelet adhesion. increases serum HDL levels. 10.An atheroma develops from: a torn arterial wall and blood clots. accumulated lipids, cells, and fibrin where endothelial injury has occurred. thrombus forming on damaged walls of veins. repeated vasospasms. 11.Low-density lipoproteins (LDL): promote atheroma development. contain only small amounts of cholesterol. transport cholesterol from cells to the liver for excretion. are associated with low intake of saturated fats. 12.When comparing angina with myocardial infarction (MI), which statement is true Both angina and MI cause tissue necrosis. Angina often occurs at rest; MI occurs during a stressful time. Pain is more severe and lasts longer with angina than with MI. Angina pain is relieved by rest and intake of nitroglycerin; the pain of MI is not 13.Typical early signs or symptoms of myocardial infarction include: brief, substernal pain radiating to the right arm, with labored breathing. persistent chest pain radiating to the left arm, pallor, and rapid, weak pulse. bradycardia, increased blood pressure, and severe dyspnea. flushed face, rapid respirations, left-side weakness, and numbness. 14.The most common cause of a myocardial infarction is: an imbalance in calcium ions. an infection of the heart muscle. atherosclerosis involving an attached thrombus. a disruption of the heart conduction system. 15.Which of the following confirms the presence of a myocardial infarction A full description of the pain, including the sequence of development The presence of elevated serum cholesterol and triglycerides Serum isoenzymes released from necrotic cells and an ECG Leukocytosis and elevated C-reactive protein 16.The most common cause of death immediately following a myocardial infarction is: cardiac arrhythmias and fibrillation. ruptured ventricle or aorta. congestive heart failure. cerebrovascular accident. 17.Which change results from total heart block A prolonged PR interval Periodic omission of a ventricular contraction A wide QRS wave Spontaneous slow ventricular contractions, not coordinated with atrial contraction 18.Which of the following is most likely to cause left-sided congestive heart failure Incompetent tricuspid heart valve Chronic pulmonary disease Infarction in the right atrium Uncontrolled essential hypertension 19.Significant signs of right-sided congestive heart failure include: severe chest pain and tachycardia. edematous feet and legs with hepatomegaly. frequent cough with blood-streaked frothy sputum. orthopnea, fatigue, increased blood pressure. 20.Paroxysmal nocturnal dyspnea is marked by: hemoptysis and rales. distended neck veins and flushed face. bradycardia and weak pulse. cardiomegaly. 21.Which of the following drugs improves cardiac efficiency by slowing the heart rate and increasing the force of cardiac contractions Furosemide Digoxin Epinephrine Nifedipine 22.Effects that may be expected from a beta-adrenergic blocking drug include: increasing systemic vasoconstriction. decreased sympathetic stimulation of the heart. blockage of an angiotensin receptor site. increased release of renin. 23.An incompetent mitral valve would cause: increased blood to remain in the right atrium. hypertrophy of the right ventricle. decreased output from the left ventricle. decreased pressure in the left atrium. 24.Which of the following describes the blood flow occurring with a ventricular septal defect From the left ventricle to the right ventricle From the right ventricle to the left ventricle Increased cardiac output from the left ventricle Mixed oxygenated and unoxygenated blood in the systemic circulation 25.Pericarditis causes a reduction in cardiac output as a result of which of the following Delays in the conduction system, interfering with cardiac rhythm Weak myocardial contractions due to friction rub Excess fluid in the pericardial cavity, which decreases ventricular filling Incompetent valves, which allow regurgitation of blood 26.A source of an embolus causing an obstruction in the brain could be the: femoral vein. pulmonary vein. carotid artery. coronary artery. 27.The basic pathophysiological change associated with essential hypertension is: development of lipid plaques in large arteries. recurrent inflammation and fibrosis in peripheral arteries. degeneration and loss of elasticity in arteries. increased systemic vasoconstriction. 28.Uncontrolled hypertension is most likely to cause ischemia and loss of function in the: kidneys, brain, and retinas of the eye. peripheral arteries in the legs. aorta and coronary arteries. liver, spleen, and stomach. 29.A friction rub is associated with: infectious endocarditis. arrhythmias. pericarditis. an incompetent aortic valve. 30.The outcome for many aortic aneurysms is: early diagnosis and repair. thrombus formation and pulmonary embolus. rupture and hemorrhage. pressure on adjacent organs or structures. 31.Shock is defined as: failure of the heart to supply sufficient blood to body cells. general hypoxia, causing damage to various organs. decreased circulating blood and tissue perfusion. loss of blood, causing severe hypoxia. 32.A compensation for shock would include: increased heart rate and oliguria. lethargy and decreased responsiveness. warm, dry, flushed skin. weak, thready pulse. 33.Neurogenic (vasogenic) shock results from systemic vasodilation due to: increased peripheral resistance and less blood in the microcirculation. increased permeability of all the blood vessels, leading to hypovolemia. slower, less forceful cardiac contractions. increased capacity of the vascular system and reduced venous return. 34.A prolonged period of shock is likely to cause: damage to, and increased permeability of, pulmonary capillaries. increased permeability of the glomerular capillaries of the kidneys. increased pH of blood and body fluids. increased systemic vasoconstriction. 35. Shock develops in patients with severe burns as a result of: extensive hemorrhage. pain and loss of plasma. direct damage to the heart. extensive hemolysis of erythrocytes. 36.A cardiac pacemaker would most likely be inserted in cases of: angina pectoris. heart block. congestive heart failure. ventricular fibrillation. 37.Which of the following statements regarding aneurysms is true Aneurysms are always caused by congenital malformations. The greatest danger with aneurysms is thrombus formation. Manifestations of aneurysms result from compression of adjacent structures. Aneurysms involve a defect in the tunica media of veins. 38.Heart block, in which a conduction delay at the AV node results in intermittent missed ventricular contractions, is called: first-degree block. second-degree block. bundle-branch block. total heart block. Chapter 17 1.Which of the following is the primary site for absorption of nutrients Stomach Duodenum Ileum Ascending colon 2.When highly acidic chyme enters the duodenum, which hormone stimulates the release of pancreatic secretions that contains very high bicarbonate ion content Gastrin Secretin Cholecystokinin Histamine 3.Which of the following stimulates increased peristalsis and secretions in the digestive tract Sympathetic nervous system Vagus nerve Increased saliva Absence of food in the system 4.Which of the following is contained in pancreatic exocrine secretions Bicarbonate ion Hydrochloric acid Activated digestive enzymes Insulin 5.What does the term gluconeogenesis refer to Breakdown of glycogen to produce glucose Conversion of excess glucose into glycogen for storage Formation of glucose from protein and fat Breakdown of glucose into carbon dioxide and water 6.The visceral peritoneum: lines the abdominal wall. hangs from the stomach over the loops of small intestine. contains many pain receptors. forms the outer covering of the stomach. 7.Severe vomiting can lead to metabolic acidosis because of increased: ketones produced. CO2 retained in the lungs and kidneys. hypovolemia and lactic acid production. metabolic rate. 8.What does the defecation reflex require Stimulation by the sympathetic nervous system Contraction of the internal anal sphincter Coordination through the sacral spinal cord Voluntary relaxation of pelvic muscles 9.What does congenital esophageal atresia cause Direct passage of saliva and food from the mouth into the trachea Repeated reflux of gastric secretions into the esophagus No fluid or food entering the stomach Gastric distention and cramps 10.Oral candidiasis is considered to: be a common bacterial infection in infants and young children. cause painful ulcerations in the mucosa and tongue. cause white patches in the mucosa that cannot be scraped off. be an opportunistic fungal infection of the mouth 11.What is a common cause of hiatal hernia An abnormally long esophagus Increased intra-abdominal pressure Stenosis of the hiatus in the diaphragm A small fundus in the stomach Which of the following individuals is likely to develop acute gastritis A long-term, heavy cigarette smoker Patient with arthritis taking enteric-coated aspirin on a daily basis A person with an autoimmune reaction in the gastric mucosa An individual with an allergy to shellfish Prolonged or severe stress predisposes to peptic ulcer disease because: of reduced blood flow to the gastric wall and mucous glands. of reduced bicarbonate content in bile and pancreatic secretions. stress increases the number of acid- and pepsinogen-secreting cells. increased epinephrine increases motility Which of the following would a perforated gastric ulcer likely cause Severe anemia Chemical peritonitis Severe gastric hemorrhage Pyloric obstruction What is frequently the first manifestation of stress ulcers Abdominal discomfort between meals and at night Nausea and diarrhea Hematemesis Sharp colicky pain with food intake Following gastric resection, the onset of nausea, cramps, and dizziness immediately after meals indicates: a large volume of chyme has entered the intestines, causing distention. severe hypoglycemia has developed. the pylorus is restricting the flow of chyme. bile and pancreatic secretions are irritating the small intestine. What is the likely effect of long-term exposure to a hepatotoxin Full recovery to normal tissue after the toxic material has been removed Acute onset of vomiting, steatorrhea, and jaundice Continued mild inflammation of the liver without permanent damage Gradual irreversible damage to the liver and cirrhosis A factor that may precipitate encephalopathy with cirrhosis is the elevated: serum urea. conjugated bilirubin. serum ammonia. serum pH. What is the primary cause of esophageal varices Increased hydrostatic pressure in the veins Alcohol irritating the mucosa Failure to inactivate estrogen Poor nutritional status What is the primary cause of increased bleeding tendencies associated with cirrhosis Anemia and leucopenia Jaundice and pruritus Recurrent infections Deficit of vitamin K and prothrombin Which factors contribute to ascites in patients with cirrhosis Increased aldosterone and deficit of albumin Severe anemia and increased serum bilirubin Hypokalemia and increased serum ammonia Hyperproteinemia and persistent hypotension What are the typical changes occurring with Crohn’s disease Degeneration and flattening of the villi in the small intestine Multiple herniations of the mucosa through weak areas of the muscularis A continuous area of mucosal inflammation and ulceration in the rectum and colon Inflamed areas of the wall of the ileum alternating with thick fibrotic or normal areas Chapter 18 Which of the following structures is most likely to be located in the renal medulla Proximal convoluted tubule Glomerulus Loop of Henle Afferent arteriole Wrong Which of the following describes the correct flow of blood in the kidney Afferent arteriole to the peritubular capillaries to the venule Efferent arteriole to the glomerular capillaries to the peritubular capillaries Peritubular capillaries to the glomerular capillaries to the venule Afferent arteriole to the glomerular capillaries to the efferent arteriole Which statement about the bladder is TRUE The bladder wall lacks rugae. Three openings from the urinary bladder form the trigone. It contracts when stimulated by the sympathetic nervous system. Continuous peristalsis in the bladder wall promotes urine flow. Which substance directly controls the reabsorption of water from the collecting ducts Renin Aldosterone Angiotensin Antidiuretic hormone Under what circumstances do cells in the kidneys secrete renin The urine pH decreases. Blood flow in the afferent arteriole decreases. Serum potassium levels are high. Serum osmotic pressure increases. Which pathophysiological process applies to acute post-streptococcal glomerulonephritis Streptococcal infection affects both the glomerular and tubule functions Ischemic damage occurs in the tubules, causing obstruction and decreased glomerular filtration rate (GFR) Immune complexes deposit in glomerular tissue, causing inflammation Increased glomerular permeability for unknown reasons Renal disease frequently causes hypertension because: albuminuria increases vascular volume. congestion and ischemia stimulate release of renin. antidiuretic hormone (ADH) secretion is decreased. damaged tubules absorb large amounts of filtrate. Common causes of urolithiasis include all of the following EXCEPT: hypercalcemia. hyperlipidemia. inadequate fluid intake. hyperuricemia. What is the common initial sign of adenocarcinoma of the kidney Gross hematuria Microscopic hematuria Sharp flank pain Oliguria Which of the following would likely cause chronic renal failure Cystitis with pyelonephritis in the right kidney Circulatory shock Diabetes Obstruction of a ureter by a renal calculus Wilms’ tumor is: a malignant tumor in the bladder. an encapsulated mass in one kidney. not considered to have a genetic origin. manifested in adulthood. Circulatory shock causes: decreased GFR and increased renin secretion. increased ADH and decreased aldosterone secretion. immediate tubule necrosis and obstruction. sympathetic nervous system (SNS) stimulation and vasodilation of afferent and efferent arterioles. Chapter 9 What is the chemical transmitter released at the neuromuscular junction Norepinephrine GABA Serotonin Acetylcholine Which of the following describes a Colles’ fracture The distal radius is broken. The distal fibula is broken. A vertebra appears crushed. A spontaneous fracture occurs in weakened bone. What limits joint movement in osteoarthritis The osteophytes and irregular cartilage surface The wider joint space Decreased amount of synovial fluid in the cavity Fibrosis involving the joint capsule and ligaments What is the basic pathology of rheumatoid arthritis Degenerative disorder involving the small joints Chronic inflammatory disorder affecting all joints Systemic inflammatory disorder due to an autoimmune reaction Inflammatory disorder causing damage to many organs Which of the following distinguishes septic arthritis Multiple joints that are swollen, red, and painful at one time Presence of mild fever, fatigue, and leukocytosis Purulent synovial fluid present in a single, swollen joint Presence of many antibodies in the blood Immovable joints are called: amphiarthroses. synarthroses. diarthroses. synovial joints. Fluid-filled sacs composed of synovial membrane located between structures such as tendons and ligaments and act as additional cushions are called: articular capsules. bursae. synovial sacs. hyaline chambers. Chapter 16 Fluid-filled sacs composed of synovial membrane located between structures such as tendons and ligaments and act as additional cushions are called: articular capsules. bursae. synovial sacs. hyaline chambers. Why does polyuria develop with diabetes mellitus Increased thirst and hypoglycemia Ketoacidosis Osmotic pressure due to glucose Diabetic nephropathy What causes loss of consciousness in a person with diabetic ketoacidosis Toxic effects of excessive insulin Excessive glucose in the blood Metabolic acidosis Lack of glucose in brain cells Which of the following does NOT usually develop as a complication of diabetes Osteoporosis Nephropathy Impotence Peripheral neuropathy Which of the following hormonal imbalances causes diabetes insipidus Increased insulin Decreased glucocorticoids Deficit of ADH Deficit of T3 and T4 Which signs are typical of Graves’ disease Facial puffiness, bradycardia, and lethargy Exophthalmos and tachycardia delayed physical and intellectual development Goiter and decreased basal metabolic rate (BMR) Which of the following is an effect of long-term glucocorticoid therapy Decreased secretion from the adrenal cortex gland An increased inflammatory response to irritants Hypotension and poor circulation Increased number of hypersensitivity reactions Which of the following conditions may precipitate or exacerbate hyperglycemia Hypothyroidism Cushing’s disease Addison’s disease Growth hormone deficit Hyperosmolar hyperglycemic nonketotic coma (HHNC) more frequently develops in patients with: type 1 diabetes. type 2 diabetes. Grave’s disease. hyperparathyroidism. Which of the following is a major function of the hormone norepinephrine Inhibition of an excessive stress response Visceral and cutaneous vasoconstriction Increased force of heart contraction Vasodilation in skeletal muscle Early signs of hyperglycemia include polyphagia, which means: thirst. increased urine output. hunger. glucose in the urine. Catabolic effects of Cushing’s syndrome include: osteoporosis. hypertension. increased erythrocyte production. moon face and buffalo hump. [Show More]
Last updated: 1 year ago
Preview 1 out of 60 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 09, 2020
Number of pages
60
Written in
Additional information
This document has been written for:
Uploaded
May 09, 2020
Downloads
0
Views
92


.png)
.png)


.png)