Health Care > QUESTIONS & ANSWERS > CCA Exam Prep - Health Records and Data Content (All)
CCA Exam Prep - Health Records and Data Content
Document Content and Description Below
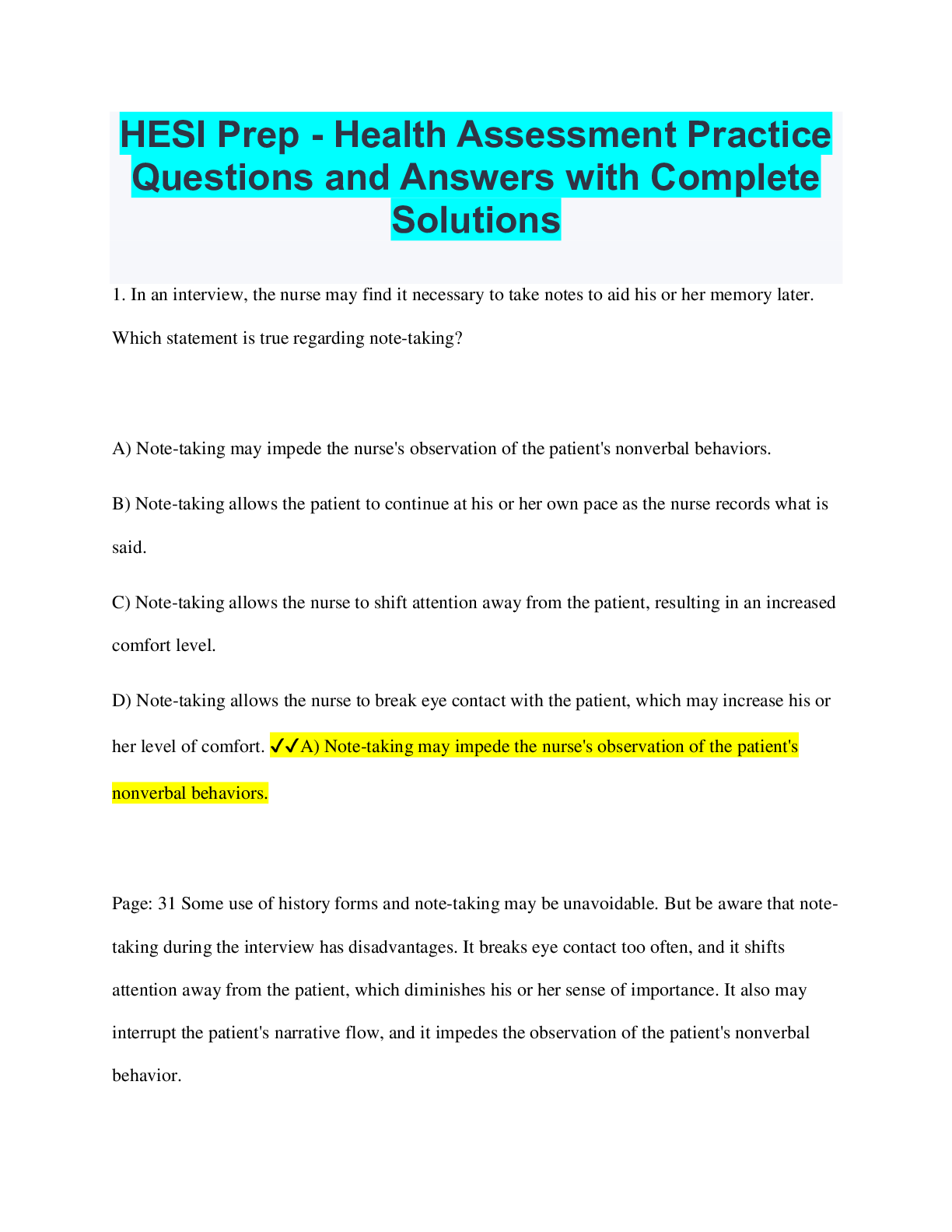
CCA Exam Prep - Health Records and Data Content The Joint Commission and CMS require hospitals to inform families of the opportunity to donate organs, tissue, or eyes. The name of the criteria that... potential donors must meet is ________. a. United Network of Organ Sharing (UNOS) b. Conditions of Participation c. Personal Health Record (PHR) d. Do Not Resuscitate (DNR) - ✔✔a. United Network of Organ Sharing (UNOS) A notation for a hypertensive patient in a physician ambulatory care progress note reads: "Continue with Diuril, 500 mgs once daily. Return visit in 2 weeks." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan - ✔✔d. Plan Documentation of aides who assist a patient with activities of daily living, bathing, laundry, and cleaning would be found in which type of specialty record? a. Home health b. Behavioral health c. End-stage renal disease d. Rehabilitative care - ✔✔a. Home health Who is responsible for writing and signing discharge summaries and discharge instructions? a. Attending physician b. Head nurse c. Primary physician d. Admitting nurse - ✔✔a. Attending physician Which of the following materials is not documented in an emergency care record? a. Patient's instructions at discharge b. Time and means of the patient's arrival c. Patient's complete medical history d. Emergency care administered before arrival at the facility - ✔✔c. Patient's complete medical history All documentation entered in the medical record relating to the patient's diagnosis and treatment is considered as this type of data: a. Clinical b. Identification c. Secondary d. Financial - ✔✔a. clinical Which of the following elements is not a component of most patient records? a. Patient identification b. Clinical history c. Financial information d. Test results - ✔✔c. financial information Which of the following would not be found in a medical history? a. Chief complaint b. Vital signs c. Present illness d. Review of systems - ✔✔b. vital signs Identify where the following information would be found in the acute-care record: "PA and Lateral Chest: The lungs are clear. The heart and mediastinum are normal in size and configuration. There are minor degenerative changes of the lower thoracic spine." a. Medical laboratory report b. Physical examination c. Physician progress note d. Radiography report - ✔✔d. Radiography report Which of the following represents documentation of the patient's current and past health status? a. Physical examination b. Medical history c. Physician orders d. Patient consent - ✔✔b. Medical history What is the function of physician's orders? a. Provide a chronological summary of the patient's illness and treatment b. Document the patient's current and past health status c. Document the physician's instructions to other parties involved in providing care to a patient d. Document the provider's follow-up care instructions given to the patient or patient's caregiver - ✔✔c. Document the physician's instructions to other parties involved in providing care to a patient Even though state laws may be more stringent, CMS requires acute healthcare records to be maintained by the acute health care organization for: a. Ten years b. At least 5 years c. Minimum of 25 years d. Permanent access - ✔✔b. At least 5 years The following is documented in an acute-care record: "Atrial fibrillation with rapid ventricular response, left axis deviation, left bundle branch block." Where would this documentation be found? a. Admission order b. Clinical laboratory report c. ECG report d. Radiology report - ✔✔c. ECG report A patient with known COPD and hypertension under treatment was admitted to the hospital with symptoms of a lower abdominal pain. He undergoes a laparoscopic appendectomy and develops a fever. The patient was subsequently discharged from the hospital with a principal diagnosis of acute appendicitis and secondary diagnoses of postoperative infection, COPD, and hypertension. Which of the following diagnoses should not be tagged as POA? a. Postoperative infection b. Appendicitis c. COPD d. Hypertension - ✔✔a. Postoperative infection The ________ may contain information about diseases among relatives in which heredity may play a role. a. Physical examination b. History c. Laboratory report d. Administrative data - ✔✔b. history Which of the following provides macroscopic and microscopic information about tissue removed during an operative procedure? a. Anesthesia report b. Laboratory report c. Operative report d. Pathology report - ✔✔d. Pathology report According to the Joint Commission Accreditation Standards, which document must be placed in the patient's record before a surgical procedure may be performed? a. Admission record b. Physician's order c. Report of history and physical examination d. Discharge summary - ✔✔c. Report of history and physical examination A method of documenting only abnormal or unusual findings or deviations from the prescribed plan of care is ________. a. Flow charting b. Discharge summary c. Charting by exception d. Care paths - ✔✔c. Charting by exception A notation for a hypertensive patient in a physician ambulatory care progress note reads: "Blood pressure adequately controlled." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan - ✔✔c. Assessment Which part of the problem-oriented medical record is used by many facilities that have not adopted the whole problem-oriented format? a. Problem list as an index b. Initial plan c. SOAP form of progress notes d. Database - ✔✔c. SOAP form of progress notes The following is documented in an acute-care record: "Spoke to the attending re: my assessment. Provided adoption and counseling information. Spoke to CPS re: referral. Case manager to meet with patient and family." Where would this documentation be found? a. Admission note b. Nursing note c. Physician progress note d. Social work note - ✔✔d. Social work note An outpatient clinic is reviewing the functionality of a computer system it is considering purchasing. Which of the following datasets should the clinic consult to ensure all the federally required data elements for Medicare and Medicaid outpatient clinical encounters are collected by the system? a. DEEDS b. EMEDS c. UACDS d. UHDDS - ✔✔c. UACDS A health record with deficiencies that is not complete within the timeframe specified in the medical staff rules and regulations is called a(n): a. Suspended record b. Delinquent record c. Pending record d. Illegal record - ✔✔b. Delinquent record The following is documented in an acute-care record: "Microscopic: Sections are of squamous mucosa with no atypia." Where would this documentation be found? a. History b. Pathology report c. Physical examination d. Operation report - ✔✔b. Pathology report Identify where the following information would be found in the acute-care record: Following induction of an adequate general anesthesia, and with the patient supine on the padded table, the left upper extremity was prepped and draped in the standard fashion. a. Anesthesia report b. Physician progress notes c. Operative report d. Recovery room record - ✔✔c. Operative report What type of data is exemplified by the insured party's member identification number? a. Demographic data b. Clinical data c. Certification data d. Financial data - ✔✔d. Financial data Standardizing medical terminology to avoid differences in naming various medical conditions and procedures (such as the synonyms bunionectomy, McBride procedure, and repair of hallus valgus) is one purpose of ________. a. Transaction standards b. Content and structure standards c. Vocabulary standards d. Security standards - ✔✔c. Vocabulary standards Which of the following reports includes names of the surgeon and assistants, date, duration and description of the procedure, and any specimens removed? a. Operative report b. Anesthesia report c. Pathology report d. Laboratory report - ✔✔a. Operative report The ________ provided the impetus for standardizing health care records with minimum standards early in the twentieth century: a. JCAHO b. AHA c. ACS d. CMS - ✔✔c. ACS Dr. Jones entered a progress note in a patient's health record 24 hours after he visited the patient. Which quality element is missing from the progress note? a. Data completeness b. Data relevancy c. Data currency d. Data precision - ✔✔c. Data currency Where would a coder who needed to locate the histology of a tissue sample most likely find this information? a. Pathology report b. Progress notes c. Nurse's notes d. Operative report - ✔✔a. Pathology report What is the defining characteristic of an integrated health record format? a. Each section of the record is maintained by the patient care department that provided the care. b. Integrated health records are intended to be used in ambulatory settings. c. Integrated health records include both paper forms and computer printouts. d. Integrated health record components are arranged in strict chronological order. - ✔✔d. Integrated health record components are arranged in strict chronological order When correcting erroneous information in a health record, which of the following is not appropriate? a. Print "error" above the entry b. Enter the correction in chronological sequence c. Add the reason for the change d. Use black pen to obliterate the entry - ✔✔d. Use black pen to obliterate the entry Under HIPAA, at the time of admission to the facility or prior to treatment by the provider, patients must be informed about the use of individual identifiable health information by signing the: a. Patient Consent Form b. Notice of Privacy Practices c. Advance Directives d. Property and Valuable List - ✔✔b. Notice of Privacy Practices A notation for a diabetic patient in a physician progress note reads: "FBS 110 mg%, urine sugar, no acetone." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan - ✔✔d. Objective Which of the following contains the physician's findings based on an examination of the patient? a. Physical examination b. Discharge summary c. Medical history d. Patient instructions - ✔✔a. Physical examination What is the function of a consultation report? a. Provides a chronological summary of the patient's medical history and illness b. Documents opinions about the patient's condition from the perspective of a physician not previously involved in the patient's care c. Concisely summarizes the patient's treatment and stay in the hospital d. Documents the physician's instructions to other parties involved in providing care to a patient - ✔✔b. Documents opinions about the patient's condition from the perspective of a physician not previously involved in the patient's care The regulations for health care record content and documentation, guidelines and regulations for which facilities are allowed to take part in or join the Medicare and Medicaid programs is: a. Medical Staff Bylaws b. Conditions of Participation c. Joint Commission Rules d. American College of Surgeon's Regulations - ✔✔b. Conditions of participation Which of the following is not a function of the discharge summary? a. Providing information about the patient's insurance coverage b. Ensuring the continuity of future care c. Providing information to support the activities of the medical staff review committee d. Providing concise information that can be used to answer information requests - ✔✔a. Providing information about the patient's insurance coverage Identify the acute-care record report where the following information would be found:Gross Description: Received fresh designated left lacrimal gland is a single, unoriented, irregular, tanpink portion of soft tissue measuring 0.8 × 0.6 × 0.1 cm, which is submitted entirely intact in one cassette. a. Medical history b. Medical laboratory report c. Pathology report d. Physical examination - ✔✔c. Pathology report Bob Smith was admitted to Mercy Hospital on June 21. The physical examination was completed on June 23. According to Medicare Conditions of Participation, which statement applies to this situation? a. The record is not in compliance because the physical examination must be completed within 24 hours of admission. b. The record is not in compliance because the physical examination must be completed within 48 hours of admission. c. The record is in compliance because the physical examination must be completed within 48 hours of admission. d. The record is in compliance because the physical examination was completed within 72 hours of admission. - ✔✔a. The record is not in compliance because the physical examination must be completed within 24 hours of admission. Documentation regarding a patient's marital status; dietary, sleep, and exercise patterns; and use of coffee, tobacco, alcohol, and other drugs may be found in the: a. Physical examination record b. History record c. Operative report d. Radiological report - ✔✔b. History record A 65-year-old white male was admitted to the hospital on 1/15 complaining of abdominal pain. The attending physician requested an upper GI series and laboratory evaluation of CBC and UA. The x-ray revealed possible cholelithiasis, and the UA showed an increased white blood cell count. The patient was taken to surgery for an exploratory laparoscopy, and a ruptured appendix was discovered. The chief complaint was ________. a. Ruptured appendix b. Exploratory laparoscopy c. Abdominal pain d. Cholelithiasis - ✔✔c. Abdominal pain The following is documented in an acute-care record: "Admit to 3C. Diet: NPO. Meds: Compazine 10 mg IV Q 6 PRN." Where would this documentation be found? a. Admission order b. History c. Physical examination d. Progress notes - ✔✔a. Admission order The following is documented in an acute-care record: "38 weeks gestation, Apgars 8/9, 6# 9.8 oz, good cry." Where would this documentation be found? a. Admission note b. Clinical laboratory c. Newborn record d. Physician order - ✔✔c. Newborn record In the acute care facility, the patient identity management tool that ensures that the right patient connects to the right information relies on: a. Master Patient Index (MPI) b. Case Mix Index (CMI) c. The Organization's clinical staff d. Cancer Registry - ✔✔a. Master Patient Index (MPI) Reviewing the health record for missing signatures, missing medical reports, and ensuring that all documents belong in the health record is an example of ________ review. a. Quantitative b. Qualitative c. Statistical d. Outcomes - ✔✔a. Quantitative In a routine health record quantitative analysis review, it was found that a physician dictated a discharge summary on 1/26/20XX. The patient, however, was discharged two days later. In this case, what would be the best course of action? a. Request that the physician dictate another discharge summary. b. Have the record analyst note the date discrepancy. c. Request the physician dictate an addendum to the discharge summary. d. File the record as complete because the discharge summary includes all of the pertinent patient information. - ✔✔c. Request the physician dictate an addendum to the discharge summary. The admitting data of Mrs. Smith's health record indicated that her birth date was March 21, 1948. On the discharge summary, Mrs. Smith's birth date was recorded as July 21, 1948. Which quality element is missing from Mrs. Smith's health record? a. Data completeness b. Data consistency c. Data accessibility d. Data comprehensiveness - ✔✔b. Data consistency During an audit of health records, the HIM director finds that transcribed reports are being changed by the author up to a week after initial transcription. The director is concerned that changes occurring this long after transcription jeopardize the legal principle that documentation must occur near the time of the event. To remedy this situation, the HIM director should recommend which of the following? a. Immediately stop the practice of changing transcribed reports. b. Develop a facility policy that defines the acceptable period of time allowed for a transcribed document to remain in draft form. c. Conduct a verification audit. d. Alert hospital legal counsel of the practice. - ✔✔b. Develop a facility policy that defines the acceptable period of time allowed for a transcribed document to remain in draft form. Mildred Smith was admitted from an acute-care hospital to a nursing facility with the following information: "Patient is being admitted for organic brain syndrome." Underneath the diagnosis, her medical information along with her rehabilitation potential was also listed. On which form is this information documented? a. Transfer or referral b. Release of information c. Patient rights acknowledgment d. Admitting physical evaluation - ✔✔a. Transfer or referral The hospital is revising its policy on medical record documentation. Currently, all entries in the medical record must be legible, complete, dated, and signed. The committee chairperson wants to add that, in addition, all entries must have the time noted. However, another clinician suggests that adding the time of notation is difficult and rarely may be correct since personal watches and hospital clocks may not be coordinated. Another committee member agrees and says only electronic documentation needs a time stamp. Given this discussion, which of the following might the HIM director suggest? a. Suggest that only hospital clock time be noted in clinical documentation b. Suggest that only electronic documentation have time noted c. Inform the committee that according to the Medicare Conditions of Participation, all documentation must be authenticated and dated d. Inform the committee that according to the Medicare Conditions of Participation, only medication orders must include date and time - ✔✔c. Inform the committee that according to the Medicare Conditions of Participation, all documentation must be authenticated and dated Which organization developed the first hospital standardization program? a. Joint Commission b. American Osteopathic Association c. American College of Surgeons d. American Association of Medical Colleges - ✔✔c. American College of Surgeons Which of the following is an example of clinical data? a. Admitting diagnosis b. Date and time of admission c. Insurance information d. Health record number - ✔✔a. Admitting diagnosis Identify where the following information would be found in the acute-care record: "CBC: WBC 12.0, RBC 4.65, HGB 14.8, HCT 43.3, MCV 93." a. Medical laboratory report b. Pathology report c. Physical examination d. Physician orders - ✔✔a. Medical laboratory report During a review of documentation practices, the HIM director finds that nurses are routinely using the copy-and-paste function of the hospital's new EHR system for documenting nursing notes. In some cases, nurses are copying and pasting the objective data from the lab system and intake-output records as well as the patient's subjective complaints and symptoms originally documented by another practitioner. Which of the following should the HIM director do to ensure the nurses are following acceptable documentation practices? a. Inform the nurses that "copy and paste" is not acceptable and to stop this practice immediately. b. Determine how many nurses are involved in this practice. c. Institute an in-service training session on documentation practices. d. Develop policies and procedures related to cutting, copying, and pasting documentation in the EHR system. - ✔✔d. Develop policies and procedures related to cutting, copying, and pasting documentation in the EHR system. A notation for a diabetic patient in a physician progress note reads: "Occasionally gets hungry. No insulin reactions. Says she is following her diabetic diet." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan - ✔✔a. Subjective A family practitioner requests the opinion of a physician specialist in endocrinology who reviews the patient's health record and examines the patient. The physician specialist records findings, impressions, and recommendations in which type of report? a. Consultation b. Medical history c. Physical examination d. Progress notes - ✔✔a. Consultation A family practitioner requests the opinion of a physician specialist in endocrinology who reviews the patient's health record and examines the patient. The physician specialist records findings, impressions, and recommendations in which type of report? a. Consultation b. Medical history c. Physical examination d. Progress notes - ✔✔b. AAAHC Mary Smith, RHIA, has been charged with the responsibility of designing a data collection form to be used on admission of a patient to the acute-care hospital in which she works. The first resource that she should use is ________. a. UHDDS b. UACDS c. MDS d. ORYX - ✔✔a. UHDDS Under HIPAA, at the time of admission to the facility or prior to treatment by the provider, patients must be informed about the use of individual identifiable health information by signing the: a. Patient Consent Form b. Notice of Privacy Practices c. Advance Directives d. Property and Valuable List - ✔✔ A notation for a diabetic patient in a physician progress note reads: "FBS 110 mg%, urine sugar, no acetone." Which part of a POMR progress note would this notation be written? a. Subjective b. Objective c. Assessment d. Plan - ✔✔ [Show More]
Last updated: 10 months ago
Preview 1 out of 22 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$10.00
Document information
Connected school, study & course
About the document
Uploaded On
Aug 02, 2023
Number of pages
22
Written in
Additional information
This document has been written for:
Uploaded
Aug 02, 2023
Downloads
0
Views
98

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)



.png)
.png)