Health Care > QUESTIONS & ANSWERS > CPC Final Exam Prep Questions and Answers Latest Updated All Answers Correct! (All)
CPC Final Exam Prep Questions and Answers Latest Updated All Answers Correct!
Document Content and Description Below
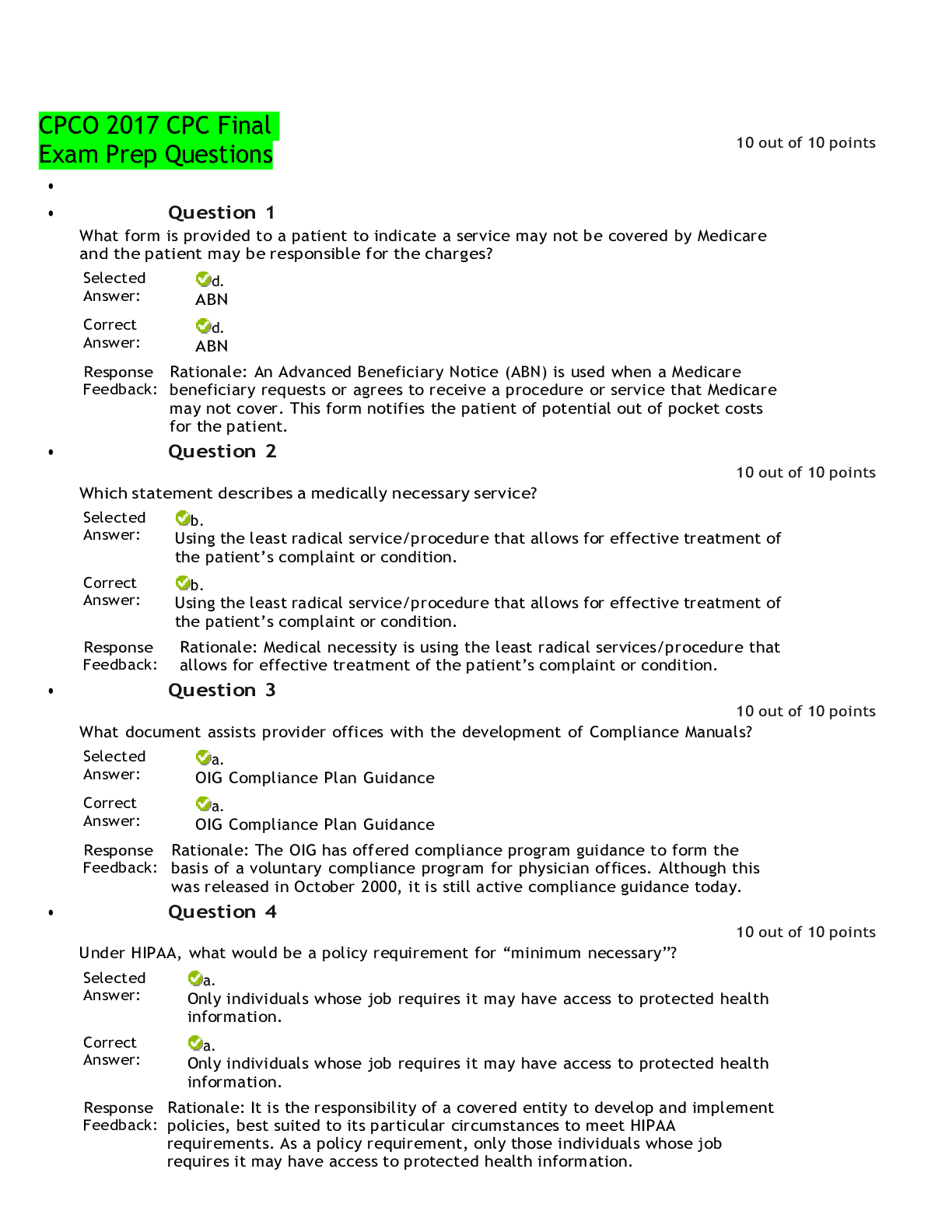
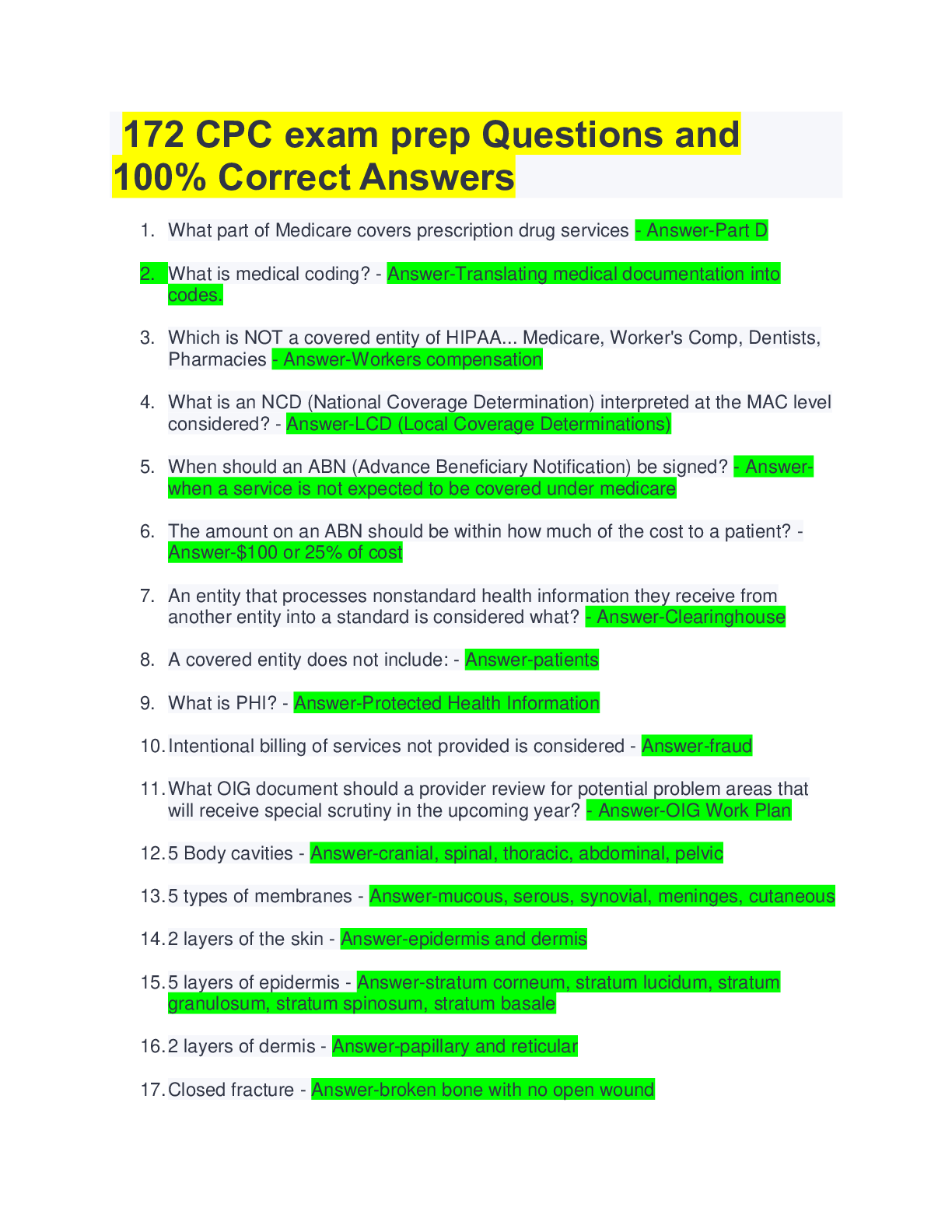
Question 1 10 out of 10 points What form is provided to a patient to indicate a service may not be covered by Medicare and the patient may be responsible for the charges? Selected Answer: d. AB... N Correct Answer: d. ABN Response Feedback: Rationale: An Advanced Beneficiary Notice (ABN) is used when a Medicare beneficiary requests or agrees to receive a procedure or service that Medicare may not cover. This form notifies the patient of potential out of pocket costs for the patient. Question 2 10 out of 10 points Which statement describes a medically necessary service? Selected Answer: b. Using the least radical service/procedure that allows for effective treatment of the patient’s complaint or condition. Correct Answer: b. Using the least radical service/procedure that allows for effective treatment of the patient’s complaint or condition. Response Feedback: Rationale: Medical necessity is using the least radical services/procedure that allows for effective treatment of the patient’s complaint or condition. Question 3 10 out of 10 points What document assists provider offices with the development of Compliance Manuals? Selected Answer: a. OIG Compliance Plan Guidance Correct Answer: a. OIG Compliance Plan Guidance Response Feedback: Rationale: The OIG has offered compliance program guidance to form the basis of a voluntary compliance program for physician offices. Although this was released in October 2000, it is still active compliance guidance today. Question 4 10 out of 10 points Under HIPAA, what would be a policy requirement for “minimum necessary”? Selected Answer: a. Only individuals whose job requires it may have access to protected health information. Correct Answer: a. Only individuals whose job requires it may have access to protected health information. Response Feedback: Rationale: It is the responsibility of a covered entity to develop and implement policies, best suited to its particular circumstances to meet HIPAA requirements. As a policy requirement, only those individuals whose job requires it may have access to protected health information. Question 5 10 out of 10 points According to the example LCD from Novitas Solutions, measurement of vitamin D levels is indicated for patients with which condition? Selected Answer: b. fibromyalgi a Correct Answer: b. fibromyalgi a Response Feedback: Rationale: According to the LCD, measurement of vitamin D levels is indicated for patients with fibromyalgia. Question 6 10 out of 10 points Select the TRUE statement regarding ABNs. Selected Answer: a. ABNs may not be recognized by non-Medicare payers. Correct Answer: a. ABNs may not be recognized by non-Medicare payers. Response Feedback: Rationale: ABNs may not be recognized by non-Medicare payers. Providers should review their contracts to determine which payers will accept an ABN for services not covered. Question 7 10 out of 10 points Who would NOT be considered a covered entity under HIPAA? Selected Answer: d. Patients Correct Answer: d. Patients Response Feedback: Rationale: Covered entities in relation to HIPAA include Health Care Providers, Health Plans, and Health Care Clearinghouses. The patient is not considered a covered entity although it is the patient’s data that is protected. Question 8 10 out of 10 points When presenting a cost estimate on an ABN for a potentially noncovered service, the cost estimate should be within what range of the actual cost? Selected Answer: c. $100 or 25 percent Correct Answer: c. $100 or 25 percent Response Feedback: Rationale: CMS instructions stipulate, “Notifiers must make a good faith effort to insert a reasonable estimate…the estimate should be within $100 or 25 percent of the actual costs, whichever is greater.” Question 9 10 out of 10 points Which act was enacted as part of the American Recovery and Reinvestment Act of 2009 (ARRA) and affected privacy and security? Selected Answer: b. HITECH Correct Answer: b. HITECH Response Feedback : Rationale: The Health Information Technology for Economic and Clinical Health Act (HITECH) was enacted as a part of the American Recovery and Reinvestment Act of 2009 (ARRA) to promote the adoption and meaningful use of health information technology. Portions of HITECH strengthen HIPAA rules by addressing privacy and security concerns associated with the electronic transmission of health information. Question 10 10 out of 10 points What document is referenced to when looking for potential problem areas identified by the government indicating scrutiny of the services within the coming year? Selected Answer: c. OIG Work Plan Correct Answer: c. OIG Work Plan Response Feedback: Rationale: Twice a year, the OIG releases a Work Plan outlining its priorities for the fiscal year ahead. Within the Work Plan, potential problem areas with claims submissions are listed and will be targeted with special scrutiny. Sunday, November 19, 2017 9:04:26 AM MST The minimum necessary rule applies to Selected Answer: b. Disclosures to or requests by a health care provider for treatment purposes. Correct Answer: d. Covered entities taking reasonable steps to limit use or disclosure of PHI Response Feedback : Rationale: The Privacy Rule generally requires covered entities to take reasonable steps to limit the use or disclosure of, and requests for, protected health information to the minimum necessary to accomplish the intended purpose. The minimum necessary standard does not apply to the following: · Disclosures to or requests by a health care provider for treatment purposes. · Disclosures to the individual who is the subject of the information. · Uses or disclosures made pursuant to an individual’s authorization. · Uses or disclosures required for compliance with the Health Insurance Portability and Accountability Act (HIPAA) Administrative Simplification Rules. · Disclosures to the Department of Health & Human Services (HHS) when disclosure of information is required under the Privacy Rule for enforcement purposes. · Uses or disclosures that are required by other law. Question 2 0 out of 4 points According to the AAPC Code of Ethics, which term is NOT listed as an ethical principle of professional conduct? Selected Answer: d. Commitmen t Correct Answer: b. Efficiency Response Feedback: Rationale: It shall be the responsibility of every AAPC member, as a condition of continued membership, to conduct themselves in all professional activities in a manner consistent with ALL of the following ethical principles of professional conduct: · · Integrity · Respect · Commitment · Competence · Fairness · Responsibility Question 3 0 out of 4 points How many components are included in an effective compliance plan? Selected Answer: c. 9 Correct Answer: d. 7 Response Feedback: Rationale: The following list of components, as set forth in previous OIG Compliance Program Guidance for Individual and Small Group Physician Practices, can form the basis of a voluntary compliance program for a provider practice: • Conducting internal monitoring and auditing through the performance of periodic audits; • Implementing compliance and practice standards through the development of written standards and procedures; • Designating a compliance officer or contact(s) to monitor compliance efforts and enforce practice standards; • Conducting appropriate training and education on practice standards and procedures; • Responding appropriately to detected violations through the investigation of allegations and the disclosure of incidents to appropriate Government entities; • Developing open lines of communication, such as (1) discussions at staff meetings regarding how to avoid erroneous or fraudulent conduct, and (2) community bulletin boards, to keep practice employees updated regarding compliance activities; and • Enforcing disciplinary standards through well-publicized guidelines. These seven components provide a solid basis upon which a provider practice can create a compliance program. Question 4 4 out of 4 points According to the OIG, internal monitoring and auditing should be performed by what means? Selected Answer: a. Periodic audits. Correct Answer: a. Periodic audits. Response Feedback : Rationale: A key component of an effective compliance program includes internal monitoring and auditing through the performance of periodic audits. This ongoing evaluation includes not only whether the provider practice’s standards and procedures are in fact current and accurate, but also whether the compliance program is working, (for example, whether individuals are properly carrying out their responsibilities and claims are submitted appropriately). Question 5 4 out of 4 points When coding an operative report, what action would NOT be recommended? Selected Answer: b. Coding from the header without reading the body of the report. Correct Answer: b. Coding from the header without reading the body of the report. Response Feedback: Rationale: Operative report coding tips include reviewing the documentation in the detail of the procedure to further clarify or define both procedures and diagnoses. Question 6 4 out of 4 points Which of the following choices is NOT a benefit of an active compliance plan? Selected Answer: a. Eliminates risk of an audit. Correct Answer: a. Eliminates risk of an audit. Response Feedback: Rationale: Although voluntary, a compliance plan may offer several benefits, among them: • Faster, more accurate payment of claims. • Fewer billing mistakes. • Diminished chances of a payer audit. • Less chance of violating self-referral and anti-kickback statutes. Additionally, the increased accuracy of provider documentation that may result from a compliance program actually may assist in enhancing patient care. Question 7 4 out of 4 points HIPAA stands for Selected Answer: d. Health Insurance Portability and Accountability Act Correct Answer: d. Health Insurance Portability and Accountability Act Response Feedback: Rationale: Health Insurance Portability and Accountability Act (HIPAA) Question 8 4 out of 4 points In what year was HITECH enacted as part of the American Recovery and Reinvestment Act? Selected Answer: a. 2009 Correct Answer: a. 2009 Response Feedback : Rationale: The Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, was signed into law on February 17, 2009, to promote the adoption and meaningful use of health information technology. Question 9 4 out of 4 points The Medicare program is made up of several parts. Which part covers provider fees without the use of a private insurer? Selected Answer: d. Part B Correct Answer: d. Part B Response Feedback : Rationale: Medicare Part B helps to cover medically necessary provider services, outpatient care and other medical services (including some preventive services) not covered under Medicare Part A. Medicare Part B is an optional benefit for which the patient pays a monthly premium, an annual deductible, and generally has a 20% co-insurance except for preventive services covered under the healthcare law. Question 10 4 out of 4 points Healthcare providers are responsible for developing ____ ____ and policies and procedures regarding privacy in their practices. Selected Answer: c. Notices of Privacy Practices Correct Answer: c. Notices of Privacy Practices Response Feedback: Rationale: Healthcare providers are responsible for developing Notices of Privacy Practices and policies and procedures regarding privacy in their practices. Question 11 4 out of 4 points Evaluation and management services are often provided in a standard format such as SOAP notes. What does the acronym SOAP stand for? Selected Answer: c. Subjective, Objective, Assessment, Plan Correct Answer: c. Subjective, Objective, Assessment, Plan Response Feedback: Rationale: S-Subjective, O-Objective, A-Assessment, P-Plan Question 12 4 out of 4 points What type of health insurance provides coverage for low-income families? Selected Answer: b. Medicai d Correct Answer: b. Medicai d Response Feedback: Rationale: Medicaid is a health insurance assistance program for some lowincome people (especially children and pregnant women) sponsored by federal and state governments. Question 13 0 out of 4 points The OIG recommends that provider practices enforce disciplinary actions through well publicized compliance guidelines to ensure actions that are ______. Selected Answer: a. Frequent Correct Answer: b. Consistent and appropriate Response Feedback: Rationale: The OIG recommends that a provider practice’s enforcement and disciplinary mechanisms ensure that violations of the practice’s compliance policies will result in consistent and appropriate sanctions, including the possibility of termination, against the offending individual. Question 14 4 out of 4 points What is the value of a remittance advice? Selected Answer: c. It states what will be paid and why any changes to charges were made. Correct Answer: c. It states what will be paid and why any changes to charges were made. Response Feedback: Rationale: The determination of the payer is sent to the provider in the form of a remittance advice. The remittance advice explains the outcome of the insurance adjudication on the claim, including the payment amount, contractual adjustments and reason(s) for denial. Question 15 4 out of 4 points HITECH provides a ____ day window during which any violation not due to willful neglect may be corrected without penalty. Selected Answer: c. 30 Correct Answer: c. 30 Response Feedback: Rationale: HITECH also lowers the bar for what constitutes a violation, but provides a 30-day window during which any violation not due to willful neglect may be corrected without penalty. Question 16 4 out of 4 points AAPC credentialed coders have proven mastery of what information? Selected Answer: d. All of the above Correct Answer: d. All of the above Response Feedback: Rationale: AAPC credentialed coders have proven mastery of all code sets, evaluation and management principles, and documentation guidelines. Question 17 4 out of 4 points What form is used to submit a provider’s charge to the insurance carrier? Selected Answer: d. CMS-1500 Correct Answer: d. CMS-1500 Response Feedback: Rationale: Once documentation is translated into codes, it is then sent on a CMS-1500 form to the insurance carrier for reimbursement. Question 18 4 out of 4 points The minimum necessary rule is based on sound current practice that protected health information should NOT be used or disclosed when it is not necessary to satisfy a particular purpose or carry out a function. What does this mean? Selected Answer: b. Providers should develop safeguards to prevent unauthorized access to protected health information. Correct Answer: b. Providers should develop safeguards to prevent unauthorized access to protected health information. Response Feedback : Rationale: The minimum necessary standard requires covered entities to evaluate their practices and enhance safeguards as needed to limit unnecessary or inappropriate access to and disclosure of protected health information. Only those individuals whose job requires it may have access to PHI. Only the minimum protected information required to do the job should be shared. Question 19 0 out of 4 points What is the purpose of National Coverage Determinations? Selected Answer: d. To set standards for all payers on coverage items. Correct Answer: b. To explain CMS policies on when Medicare will pay for items or services. Response Rationale: National Coverage Determinations (NCD) explain CMS policies on [Show More]
Last updated: 1 year ago
Preview 1 out of 314 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 25, 2022
Number of pages
314
Written in
Additional information
This document has been written for:
Uploaded
Apr 25, 2022
Downloads
0
Views
69

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)
 (1).png)
.png)
.png)
.png)

